What is known about the disease?
Cervical cancer (ICD-10 code: C53) is an epithelial malignant tumor. It begins to grow on the mucous surface of the cervix or in the cervical canal from transformed (atypical) cells of the integumentary or glandular epithelium.
The key cause of intraepithelial malignant transformation is the influence of oncogenic human papillomaviruses (HPV 16,18 and some other types) on cells.
Location of the cervix. Where does cervical cancer start?
Read more about the stages of development, diagnosis, symptoms and modern methods of treating early forms of this disease: Cervical cancer - the first signs, manifestations and symptoms. How to determine?
Return to contents
Anatomical structure
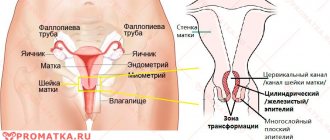
The development of cervical cancer is closely related to the characteristics of its structure. Contrary to popular belief, the cervix cannot be considered an independent separate organ. This is the lower part of the uterus, which is distinguished by its anatomical narrowness and small size.
Visually, the neck resembles a muscular tube, which reaches a length of several centimeters. The importance of the cervix in the structure of the organs of the reproductive system cannot be overestimated. The cervix occupies an intermediate position between the uterus and vagina, being a kind of barrier. The cervix protects the uterine cavity from infections and takes part in conception and childbirth.
It is known that cancer can develop from two different tissues that cover different parts of the cervix. The epithelium comes in two varieties:
- flat multilayer, located in the vaginal part;
- single-layer cylindrical, lining the surface of the cervical canal.
A gynecological examination is an examination of the vaginal part of the cervix. This is due to the fact that only this small area of the cervix is visible to the naked eye. For example, the supravaginal part, which occupies a significant area, is invisible.
Examining the vaginal part of the cervix in the speculum, the doctor sees a homogeneous pale pink epithelium, characterized by a smooth surface. This appearance is due to flat stratified epithelium.
The cellular elements of stratified epithelium are arranged in three layers.
- Basal. It is noteworthy that the cells of this layer are immature. Externally they look round. In addition, each cell contains one large nucleus. The basal layer is the deepest. It is bordered by adjacent vessels, nerves and muscles that represent the stroma.
- Intermediate. This layer consists of raised, maturing cells. Despite their immaturity, the cellular elements appear flattened. As cells develop, their nucleus becomes smaller.
- Surface. Mature cells are localized here, characterized by a flat shape and one small nucleus. Cellular elements function according to their location. Thanks to their ability to slough off, squamous stratified epithelium has the ability to renew itself.
The cervical canal, which is located inside the cervix, is essential. The cervical canal is narrow. It connects the vagina and uterine cavity.
It is known that the vagina is inhabited by various microorganisms that can enter the uterine cavity through the cervical canal. However, thanks to the glands that produce protective mucus, the uterine cavity remains sterile.
The surface of the cervical canal differs from the vaginal part of the cervix, since they are formed by different types of epithelium. The cervical canal is covered with a single-layer cylindrical epithelium, which gives the mucosa a reddish color and velvety feel.
The lower edge of the cervical canal opens into the vagina, forming the so-called internal os. Here is the transformation zone, which represents the junction of squamous and columnar epithelium. From above, the cervical canal forms an internal os that opens into the uterine cavity.
Stages of cervical cancer
To describe the severity of the tumor process in the case of cervical cancer, the TNM classification, standard for any malignant neoplasm, and the special (adopted in 2009 to describe specifically cervical cancer) FIGO system are used.
Stage 1 of cervical cancer – designated I or T1N0M0. At this stage, the primary tumor (T1) is located exclusively within the cervix, rarely affects regional lymph nodes (N0), and does not metastasize (M0) to other organs. Read more: Stage 1 (first) cervical cancer - prognosis, treatment, symptoms
Stage 2 of cervical cancer (II or T2N0M0) occurs with minimal damage to the lymphatic system (N0-1), without metastases (M0). But the primary tumor is already quite large: it grows from the cervix into the vagina, onto the body of the uterus and into the periuterine connective tissue. Read more: Stage 2 (second) cervical cancer - prognosis, treatment and symptoms
Stage 3 CC (III or T3N01M0) – a locally advanced tumor actively metastasizes to regional lymph nodes (N1-2), affects almost the entire vaginal tube and/or grows into the tissue surrounding the uterus up to the pelvic walls. Read more: Stage 3 (third) cervical cancer – how long do they live after treatment?
Features of stage 4
Classification of stage 4 cervical cancer
| Stage 4 (according to FIGO) | Stage 4 (according to TNM) | Description |
| IVA or 4a stage | Т4N1-2М0 | The tumor infiltrates beyond the cervix and body of the uterus, capturing adjacent organs and tissues on its way, including the bladder and rectum. The pelvic lymph nodes (N1-2) are affected. Tumor metastases outside the pelvis at stage IVA are not yet detected (M0). |
| IVB or 4b stage | AnyNanyM1 | At the advanced stage IVB, the size of the primary tumor is not decisive (the area of the primary lesion can correspond to T4 or T1, T2, T3). The decisive fact here is the spread of the tumor through the lymphatic and circulatory system beyond the pelvis with the formation of secondary foci - metastases (M1)* |
*Where stage 4 cervical cancer metastasizes: - more often: in the inguinal, retroperitoneal, para-aortic, supraclavicular lymph nodes, designated: M1(lym) - in the lungs and/or pleura: M1(pul) and/or M1(ple) - in liver: M1(hep) - to the bones and/or bone marrow: M1(oss) and/or M1(mar) - to the ovaries and fallopian tubes, any other organs M1(oth) - in rare cases: to the brain M1( bra).
Cervical cancer stages 4a and 4b Return to contents
Tumor size: T = Tumor, tumor
The number next to the "T" tells you the size of your main tumor and the tissue it has damaged.
Tx
— Doctors do not have enough data to assess the size of the tumor.
T0
- the main tumor was not detected.
Tis
- the so-called “carcinoma in situ” - cancer cells are found in the superficial layer of uterine tissue.
T1a
- the tumor has grown no deeper than the first, inner layer of the uterus - the endometrium, or has damaged less than half the thickness of the second - the myometrium.
T1b
- the tumor has grown deeper than half of the second layer of the uterine wall.
T2
- oncology has spread to the tissue of the cervix, but has not spread beyond the organ itself (uterus + cervix).
T3a
—The cancer has affected the outer lining of the uterus (serous), fallopian tubes, or ovaries.
T3b
- the tumor has spread to the vagina or surrounding tissues - parametrium.
T4
—The cancer has damaged the lining of the bladder or colon.
How long do people live with stage 4 cervical cancer?
Survival at the terminal stage of cervical cancer largely depends on the characteristics of the patient’s body and the properties of the tumor.
To predict life expectancy for stage 4 cervical cancer, the prognosis is compiled individually.
According to statistics, 7-12 women out of 100 live more than 5 years with a diagnosis of stage 4 cervical cancer (five-year survival rate is approximately 7-12%)
The two-year survival rate at stage IVB does not exceed 11%, that is, out of 100 women, only 11 live for more than 2 years.
Worsens the prognosis: - presence of metastases (stage IVB) - histological type of tumor: adenocarcinoma - poorly differentiated tumor: G 3-4 - high proliferative index of tumor growth: Ki-67 more than 50%.
Return to contents
Tumor differentiation: G = Grade, assessment
Differentiation is an indicator that tells how much cancer cells differ from normal cells - those from which they turned into tumor cells.
To determine the degree of differentiation, the doctor will take a small amount of tumor tissue from you and send it to the laboratory for testing. The more the cells have changed, the worse they respond to treatment and the faster they grow and multiply.
GX
suggests that doctors do not know how different cancer cells are from healthy ones.
G1
— tumor cells are very similar to healthy ones. This is a highly differentiated cancer of the uterine body. Such tumors grow slowly and are well treated.
G2
- moderately differentiated cancer of the uterine body. Its cells do not grow quickly and respond well to treatment.
G3
- low-grade cancer of the uterine body, the cells of which are very different from healthy ones. It is poorly treated, but grows quickly.
G4
- undifferentiated cancer of the uterine body. His cells are not at all similar to the healthy ones from which they were formed. Such tumors are the most difficult to treat and develop quickly.
Often, instead of the letter “G” in the diagnosis, you can see a verbal description of differentiation: for example, “well differentiated cancer of the uterine body.”
Marika Otkhozoria,
gynecologist, candidate of medical sciences, clinic “Medicine 24/7”
“The degree of tumor differentiation indicates a possible prognosis for the course of the disease and determines the treatment regimen.
The prognosis for patients with highly differentiated uterine cancer is very good - life expectancy for almost 90% of them is more than 5 years. In cases of poorly differentiated tumors, this figure is much lower - approximately 65%."
Symptoms of stage 4 cervical cancer
- Bleeding from the genital tract of various types: - contact (during sexual intercourse, lifting weights, defecation, gynecological examination, etc.) - spontaneous, associated or not associated with the menstrual cycle - bleeding after menopause
- Pathological leucorrhoea (discharge from the genital tract): - bloody, bloody - bloody with an unpleasant odor - purulent with an admixture of blood with an unpleasant odor
- Pain in stage 4 cervical cancer: - in the lower abdomen - in the lower back - in the sacrum - in the rectum - pain can radiate to the groin, buttock, thigh - pain in the bones (with metastases in the bones) - metastatic pain (pain in the location of the secondary tumor focus)
- With metastatic lesions of the pelvic and inguinal lymph nodes: - persistent swelling of the legs (one or both)
- When cancer spreads to the bladder: - frequent urge to urinate - incomplete emptying of the bladder - persistent cystitis - blood in the urine - vesico-vaginal fistulas
- When the tumor compresses the ureters: - hydronephrosis, pyonephrosis - uremia
- When cancer spreads to the rectum: - persistent constipation - mucus in the stool - blood in the stool - fistula between the vagina and rectum
- With metastases to the ovaries and/or liver: - ascites
- In case of metastatic damage to the lymph nodes and other internal organs: - palpable enlargement of the lymph nodes - dysfunction of the affected organ
- Symptoms of general intoxication: - weakness, poor health, sudden loss of strength - nausea, loss of appetite, weight loss - not always: prolonged increase in body temperature
Signs of cervical cancer
Reasons for late diagnosis
Clinically pronounced cervical cancer is easily recognized during a routine gynecological examination.
Why, at the time of initial detection, in approximately 30-40% of patients, cervical cancer is already detected at advanced stages 3-4 that are difficult to treat?
The main reasons for late diagnosis of cervical cancer
- Lack of popularization and organization of cervical cervical cancer screening
- False negative PAP test result (in 20% of cases, the cellular composition of the cytogram does not reflect the presence of a malignant process)
- Poor training and/or insufficient oncological alertness of obstetricians and gynecologists
- Errors in primary diagnosis and subsequent incorrect treatment
- A woman’s negligent attitude towards her own health (irregular, extremely rare visits to the gynecologist, ignoring the recommendations of the attending physician, low awareness of the disease and/or underestimation of the seriousness of her condition...)
- Low socio-economic standard of living of the patient
The only way to “not lead yourself” to advanced cancer is a regular, at least once every 6-12 months, preventive examination by a qualified gynecologist.
“If a woman dies of cervical cancer, then someone else besides cancer is to blame for her death” Charles Cameron
Return to contents
Lymph nodes: N = Nodes, regional lymph nodes
The doctor definitely needs to know whether your lymph nodes have been affected by cancer (= link to an article about lymph nodes) - this is necessary both to determine the stage of the disease and to select the correct therapy. The lymphatic system supplies our tissues with fluid and helps fight infections and harmful substances, and the lymph nodes in it act as filters.
Lymph nodes that belong to a specific area of the body are called regional. For the uterus, regional lymph nodes are considered to be pelvic and para-aortic.
Information about the condition of the lymph nodes is coded with the letter “N”:
NX
— Doctors do not know whether your lymph nodes are affected by cancer.
N0
- lymph nodes are healthy.
N1
- cancer was found in the pelvic lymph nodes.
N2
— the para-aortic lymph nodes were affected by cancer.
Lymph nodes: structure, functions, research methods October 9, 20202004 3
Methods for diagnosing stage 4 cervical cancer
Gynecological examination
A recto-vaginal examination and examination “on the chair” are performed using a gynecological “mirror” and/or an optical colposcope.
With advanced cancer, the initial examination easily reveals characteristic changes in the cervix.
PAP test
Cytological examination of smears from the surface of the cervix and cervical canal (ecto- and endocervix).
Histological verification of diagnosis
The final diagnosis of cervical cancer must be confirmed by histological examination of a sample of tumor tissue.
Histology - the study of tissue structure under a microscope - is a decisive method for diagnosing any tumor.
Without a histological analysis, it is impossible to unambiguously establish a diagnosis of cervical cancer.
Biomaterial (a sample of tissue suspicious for cancer) for histological examination is obtained by means of a knife biopsy; if necessary, diagnostic curettage of the cervical canal is performed.
Read more about cervical biopsy here: Cervical biopsy - how it is done and what it shows, preparation and progress of the operation
Immunohistochemistry
This is a modern technique for clarifying the diagnosis of malignant neoplasms.
Immunohistochemical analysis of a biopsy specimen (or a tissue sample removed during extensive surgery) complements but does not replace histology.
The results of immunohistochemistry determine the “biological portrait” of the tumor: - degree of malignancy G (G1 - low-grade, with a good prognosis; G2 - moderately malignant; G3-4 - very malignant, poor prognosis) - tissue affiliation (in the case of undifferentiated and/or metastatic tumors) — sensitivity of the tumor to radiation, hormones and/or chemotherapy (to select the optimal treatment tactics) — degree of tumor aggressiveness (Ki-67) — etc.
Proliferative index Ki-67 – what is it? This is an indicator of the activity (rate of growth and spread) of the tumor, or more precisely, an index of the rate of reproduction (mitotic division) of malignant cells.
The higher the Ki-67 index, the more aggressive the tumor behaves, the worse the prognosis.
The Ki-67 value can indicate how sensitive the tumor is to treatment.
If after a course of radiation and/or chemotherapy the level of Ki-67 decreases, one can hope for clinical remission of the disease.
Prediction of disease-free survival according to the Ki-67 index
(V.L. Vinokurov et al., 2008)
| Proliferative activity index (for squamous cell cancer) | Estimated average life expectancy after radiation treatment |
| Ki-67 ‹50% | 80 months |
| Ki-67 ›50% | 47 months |
Ultrasound
Echography (ultrasound) and Doppler ultrasound (vascular ultrasound) of the pelvic area, abdominal cavity and retroperitoneal space are carried out to detect signs of spread of the malignant process beyond the cervix.
To assess tumor metastasis, ultrasound of the inguinal and supraclavicular lymph nodes is performed.
MRI or CT with intravenous contrast
Contrast magnetic resonance imaging of the pelvis and abdominal cavity assesses the depth of tumor invasion into the periuterine tissue and adjacent organs, and identifies tumor metastases to distant organs and bones.
PET or PET-CT, PET-MRI
A highly informative (unfortunately, not always accessible) method for detecting invasion and metastases of cervical cancer is positron emission tomography.
Hybrid device for simultaneous positron emission and magnetic resonance imaging (PET-MRI) Additional studies
To assess the prevalence and identify secondary tumor foci, to plan optimal treatment tactics according to indications, the following is carried out:
- Chest X-ray
- Urography
- Cystoscopy
- Rectosigmoscopy
- Renal scintigraphy
- Scintigraphy and radiography of skeletal bones
- MRI of the brain
- and etc.
Return to contents
Treatment tactics and prognosis
In most cases, when a woman is diagnosed with late-stage cancer in the uterus, she will receive palliative treatment. Its essence is to maintain vital functions at a decent level for as long as possible.
To slow down the growth and reproduction of cancer cells in organs distant from the uterus, modern antitumor drugs are introduced. For the same purpose, courses of radiation therapy may be recommended. Often these two methods are used in combination.
However, since the woman’s body is significantly weakened due to cancer, radiation and chemotherapy are difficult for her to tolerate. Most often, women refuse such palliative treatment. They are given adequate medications to reduce the severity of pain, hepatoprotectors to improve liver function, as well as vitamins to increase immune barriers.
Experts urge people not to give up - research to find cures for late-stage cancer is being conducted all over the world. Therefore, there is always a chance to win.
Source: pro-rak.ru
Treatment of stage 4 cervical cancer
To cure stage 4 cervical cancer completely is unlikely.
Objectives of treating advanced late-stage cancer: - achieving partial remission of the disease - providing adequate pain relief, symptomatic treatment - optimal maintenance of all body functions - improving physical and psycho-emotional state, increasing the quality and life expectancy of the patient
Chemoradiation therapy
Remote radiotherapy of stage IVA cervical cancer is carried out according to an individual plan, taking into account all indications, contraindications, and the general condition of the patient.
Modern 3D conformal radiation therapy (3D-CRT) provides good results. The latest equipment allows you to convert and direct radiation beams to tumor areas, minimizing the radiation dose to healthy tissue.
Modern installation (linear accelerator) for 3-dimensional conformal radiation therapy
Simultaneously with radiation, the patient receives chemotherapy (Cisplatin + others)
Chemotherapy drugs for the treatment of cervical cancer (used in combination): Cisplatin Carboplatin Irinotecan Ifosfamide 5-fluorouracil Methotrexate Paclitaxel Doxorubicin Cyclophosphamide Gemcitabine
After completion of chemoradiotherapy, it is possible to prescribe maintenance (adjuvant) chemotherapy according to an individual plan and symptomatic palliative treatment.
Return to contents
Forecasts
At stage 4 there is no room for predictions, because it is impossible to cure the disease, but life expectancy of up to 5 additional years is quite realistic. Survival rates range from 33 to 60 percent of all patients.
To do this you need:
- Find quality professionals who know what they do and why.
- Have a good mood and try not to lose faith in the best.
- Find support in loved ones or friends.
All these factors will help the patient endure painful chemotherapy and then maintain the body in proper condition.
Is surgery necessary for stage 4 cervical cancer?
The standard operation for stage 4 cervical cancer is partial or total pelvic exenteration.
Such operations in rare cases serve as an alternative to chemoradiotherapy for primary patients with stage 4A, if the tumor has not spread to the pelvic wall.
What is partial pelvic exenteration?
This is a gynecological operation of the 5th type, during which the following are removed: - the body and cervix (with or without appendages) - a section of the vagina - the parametrium (all peri-uterine tissue with regional lymph nodes) - the terminal (final) section of the ureter - and/or a section of the urinary tract bladder - and/or part of the colon
What is total pelvic exenteration?
This is a voluminous, mutilating, but life-prolonging operation during which the following are removed: - body and cervix (with or without appendages) - parametrium with regional lymph nodes - vagina - bladder - rectum
When is surgery possible?
(indications for exenteration):
- Primary patient with stage 4A (without tumor lesions of the pelvic walls)
- Presence of fistulas (vesicovaginal or rectovaginal)
- Ineffectiveness of chemoradiation therapy
- Isolated tumor recurrence in the pelvis
Contraindications to exenteration surgery
- Unilateral lower limb edema (edema of one leg)
- Sciatica
- Ureteral block (hydronephrosis)
The triad of these symptoms indicates cancer has grown to the walls of the pelvis (the tumor is inoperable).
Currently, with the improvement of radiation therapy, pelvic exenteration for the treatment of cervical cancer is used extremely rarely.
Treatment of cervical cancer stage IVB
At a late stage of the disease, there are already distant metastases - secondary tumor foci in various organs.
The main treatment for stage IVB CC is intravenous systemic chemotherapy with the mandatory inclusion of platinum-containing drugs (Cisplatin + others) and symptomatic palliative treatment.
In some cases, radiation therapy is carried out according to an individual plan.
Targeted therapy
Targeted (from: target - goal) or molecular targeted therapy of malignant tumors is a new, very promising direction in the drug treatment of common (advanced) forms of cervical cancer.
The principle of targeted therapy is the targeted blocking of a number of receptor proteins located on the surface of the cancer cell, which are responsible for nutrition, active growth and metastasis of the tumor.
Expected effects of targeted therapy: - increasing the sensitivity of the tumor to radiation and chemotherapy (which significantly improves the effectiveness of treatment) - achieving long-term remission after treatment - improving the prognosis of relapse-free survival.
The most studied targeted anticancer drugs
/included in systemic chemotherapy regimen/
| Tradename | Active substance | Description |
| Tarceva® | Erlotinib | Blocks thyroxine kinase - epidermal growth factor site (EGFR). Inhibits the growth and/or leads to the death of a clone of tumor cells. |
| Iressa | Gefitinib | Competitively binds thyroxine kinase - epidermal growth factor site (EGFR). Stops proliferative reproduction and activates the natural death of cancer cells. |
| Nexavar | Sorafenib | Potent inhibitor of intracellular kinases. Disturbs nutrition and suppresses the growth of tumor metastases. |
| Erbitux | Cetuximab | Chimeric monoclonal antibody of the IgG1 class. Suppresses tumor growth and metastasis. |
| Avastin | Bevacizumab | Recombinant humanized monoclonal antibody, EGFR inhibitor. Inhibits nutrition and tumor growth. |
Targeted drugs for the treatment of cervical cancer
Further study, improvement and widespread introduction into medical practice of targeted and multi-targeted drugs provides a real opportunity for successful treatment of patients with advanced stage 3-4 cervical cancer.
Return to contents
Pathogenesis
Cervical cancer is not an overnight process. In its development, pathology goes through several stages, which include both precancerous and malignant changes.
Cervical cancer is a natural completion of precancerous changes, which imply dysplasia. Initially, changes in the cellular structure appear, which lead to the appearance of malignancy and signs of aggressive growth.
The pathological influence of certain factors causes the appearance of atypia in cells, manifested by changes in the shape and structure of cells. Modified cellular elements cannot function adequately in the epithelium, which leads to various disorders.
Dysplasia has several degrees of severity.
- The mild degree is designated as CIN I. At this stage, pathological changes are observed that affect only the lower layer. However, cervical cancer rarely develops, since the body usually copes with the changes on its own. In the unfavorable case, oncology can occur in approximately five years.
- The average grade is called CIN II. Half of the epithelial layer is involved in the pathological process. Self-regression is possible, but unlikely. The appearance of cervical cancer usually occurs after three years.
- Severe degree is called by gynecologists as CIN III. The division into layers is lost, atypical cells are located throughout the epithelial thickness. If left untreated, cervical cancer can be detected within a year.
It is noteworthy that third-degree dysplasia is considered a pre-invasive cancer. In this case, signs of malignancy are revealed without invasion into the stroma. Third-degree dysplasia and preinvasive cancer have a common diagnostic and treatment algorithm. The prognosis with timely treatment is favorable. Cured pathology does not affect life expectancy.
Treatment
Many types of treatment cannot be used at the last stage of oncology, which is explained by the large size of the tumor and the presence of multiple secondary foci. Let's consider the main methods of treating cervical cancer:
Surgery. If at stages 1, 2 and 3 of the disease surgery acts as the most effective method of treatment, then in this case this approach will be ineffective. Even if the primary focus (cervix, uterine body and part of the vagina) is removed, it will be impossible to stop the growth of the tumor, since the tumor metastasizes to other organs.
Chemotherapy. Involves taking potent drugs that negatively affect cancer cells. As a result of the use of such medications, pathological cells are destroyed and lose their ability to grow and reproduce. The doctor carries out an individual selection of medications, which can be solutions for intravenous infusions or tablets. Chemotherapy is prescribed in courses with some interval between them. This type of treatment at stage 4 of the disease is quite effective.
Radiation therapy (radiotherapy). I use x-rays on the patient's body. Cancer cells are more susceptible to such rays than healthy tissue, so the tumor is destroyed first. With metastatic cervical cancer, radiation in some cases may be the only chance for remission.
Most often, doctors are inclined to complex treatment, which includes chemotherapy, radiotherapy, immunotherapy and supportive therapy to restore vitality.