Procedure for taking cervical scrapings
Typically, the material required for research is collected using a special spatula and brush, which capture a very large number of cells from the upper epithelium of the cervix, thereby providing a larger amount of material for study on laboratory glass. Such equipment does not damage the material, which means there is no need to worry that the results of the cells being studied may be inaccurate. After taking a scraping, the material is processed using a special fixing solution, then it is stained with the necessary dye and sent for examination to a morphologist who studies the material in detail, at the end he gives a detailed cytological conclusion.
This procedure is absolutely painless and imperceptible, however, there are some contraindications when collecting such material. For example, cervical scrapings should not be taken during menstruation or any other discharge from the vaginal area. The procedure is also contraindicated during inflammatory processes in the genital organs. The fact that an inflammatory process is occurring in a woman’s body, or more precisely in the genitals, is not difficult to determine by a number of signs (the presence of white or yellow discharge, itching, burning and discomfort). Thus, before taking scrapings from a sick woman, treatment should be carried out and the infection should be eliminated. Gynecologists recommend taking a scraping as soon as menstruation ends or on the eve of its start. Before the procedure, it is contraindicated to have sex without a condom and douche, so as not to disturb or wash out the cervical flora.
Histological examination of scrapings and aspirates from the cervical canal and uterine cavity
Histological examination of scrapings and aspirates from the cervical canal and uterine cavity
- This is an examination of the patient’s surgical material under a microscope. The purpose of the study is to detect pathological deviations from the normal structure of tissues, identify malignant cells or their precursors, and the degree of prevalence of the pathological process. Histological studies in gynecology make it possible to establish a diagnosis for various diseases of the female reproductive system with the greatest degree of certainty. Using histological analysis, the function and structure of tissue cells is studied.
With the help of histological examination, inflammation or tissue degeneration, the type of tumor, and its nature are accurately determined. For histological examination, the material obtained from scraping or aspirate is prepared in a special way (placed in a fixing liquid, filled with paraffin, dried, thin sections are made with a special device, then they are stained and placed under a microscope).
How is scraping obtained?
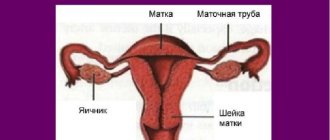
The vagina and uterine cavity are connected by the cervical canal, which passes through the cervix. The cavity of the uterus and cervical canal is lined with mucous membrane. For analysis, by scraping with special instruments, they try to obtain this shell and not affect the next layer. Sometimes a test scraping is done - a small area of the mucous membrane of the cervical canal or some areas of the uterine cavity is scraped off. Most often, a complete curettage is done and all the resulting material is collected, making sure to note where the sample was taken from. Curettage is performed under anesthesia.
How is aspirate obtained?
A more gentle method to obtain the contents of the uterine cavity is the vacuum aspiration method. At the moment, modern, improved vacuum syringes are used for such purposes. With the help of such a syringe, the contents of the uterine cavity are sucked out, and the delicate mucous membrane is less injured. No special preparation is required for this procedure. Vacuum aspiration is usually performed in a antenatal clinic and lasts several minutes; no special anesthesia is required.
The histological conclusion, drawn up on the basis of changes in the tissue under study recorded by the morphologist, allows one to confirm an existing clinical diagnosis or establish a new one, and is considered by doctors and their patients as the final stage of diagnosis.
Important! Histological examination can detect pathology at an early stage of the disease.
Indications
Scraping and aspirate for histological examination from the cervical canal and uterine cavity are done in order to:
- identify the cause of infertility;
- determine hormonal levels;
- identify the presence of a malignant formation;
- with uterine bleeding of unknown etiology.
Preparation
Conditions for preparation are determined by the attending physician.
Interpretation of results
The conclusion may contain an indicative or final diagnosis, in some cases only a “descriptive” answer. The approximate answer allows you to determine the range of diseases for differential diagnosis. The final diagnosis of the pathologist is the basis for formulating a clinical diagnosis. A “descriptive” answer, which may occur when there is insufficient material or clinical information, sometimes allows us to make an assumption about the nature of the pathological process. In some cases, when the sent material turns out to be scanty and insufficient for a conclusion, and the pathological process may not have been included in the piece being examined, the pathologist’s conclusion may be “false negative.” In cases where the necessary clinical and laboratory information about the patient is missing or is ignored, the pathologist’s response may be “false positive.” In order to avoid “false negative” and “false positive” conclusions, it is necessary, together with a clinician, to conduct a thorough clinical and anatomical analysis of the detected changes with a discussion of the results of the clinical and morphological examination of the patient.
Evaluation of cytological examination results
So, what can be determined by the amount of material sought? If the material taken is complete, or, as it is also called, adequate, then the smear is considered to be of good quality, containing a significant number of the desired cell types. Insufficiently complete material is the material where endocervix cells are absent, as well as squamous epithelial cells, which may be present in small quantities. Inferior material is considered to be material from which it is impossible to judge the presence (or, conversely, absence) of any pathological changes that have occurred in the cervix.
If the conclusion reads “cytogram without features,” this means that all epithelial cells are normal, and the cytogram corresponds to your age. In the case of inflammatory changes in the epithelium, in a woman’s body, for example, the number of leukocytes, cocci or various types of harmful bacilli may increase. The latter may also be a signal of the presence of infectious agents (including yeast and Trichomonas). In addition, the conclusion may indicate the likelihood or firm belief of the presence of malignant cells and malignant neoplasms.
Cytological examination of scrapings from the cervix (exocervix, 1 glass)
Examination of cervical scraping (exocervix, 1 glass)
- carried out for the purpose of diagnosing changes in the epithelium of the exocervix and diagnosing early precancerous diseases and cervical cancer.
The exocervix
is the outer part of the cervix that comes into contact with the vagina (the vaginal part of the cervix).
Cytological examination of cervical scrapings has helped save the lives of millions of women, since with this method it is possible to detect pre-cancer or cervical cancer while it is still curable.
Risk factors for developing cervical cancer:
- infection with human papillomavirus (oncogenic serotypes HPV16, HPV18, HPV31, HPV33, HPV45, etc.);
- smoking;
- chlamydial or herpes infection;
- chronic inflammatory gynecological diseases;
- long-term use of contraceptives;
- several births;
- family history of cervical cancer;
- early onset of sexual activity;
- frequent change of sexual partners;
- insufficient intake of vitamins A and C from food;
- immunodeficiencies and HIV infection.
Screening women aged 25–64 years at 5-year intervals can lead to an 84% reduction in mortality, and screening 25–63 year-olds at 3-year intervals can lead to a 90% reduction in mortality.
The risk of developing invasive cancer is 5 to 10 times higher in women who have never been screened. It is recommended that women who are sexually active undergo a smear for oncocytology annually during a routine examination by a gynecologist.
Indications:
- screening and diagnosis of precancerous and cancerous diseases of the cervix.
Preparation
In women of reproductive age, it is advisable to take a smear for examination no earlier than the 5th day from the start of the menstrual cycle or no later than 5 days before the expected start of menstruation.
24 hours before collection, you must stop using vaginal medications, spermicides, lubricants, and avoid sexual intercourse. You should not douche the day before your smear test.
If there is a visual pathology on the cervix, a smear should be taken regardless of the above factors.
Recommendations for passing the study
With regular preventive examination of all women over 25 years of age (it is recommended to take the test annually).
When examining girls under 25 years of age who are sexually active.
Starting from the age of 25 years, cytology must be taken every 2 years. If the next smear for atypia reveals any undesirable changes, then subsequent examinations will need to be carried out more often: 1–2 times a year (depending on the changes detected).
Interpretation of results
I. Amount of material.
- The material is complete (adequate) - a smear of good quality, containing a sufficient number of appropriate cell types.
- The material is insufficiently complete (insufficiently adequate) - the material does not contain endocervical cells and/or metaplastic cells, squamous epithelial cells are in insufficient quantities or the cellular composition is poor.
- The material is defective (inadequate) - it is impossible to judge from the material the presence or absence of pathological changes in the cervix.
II. Interpretation of results.
- The cytogram is without features
- epithelial cells are within normal limits, the cytogram corresponds to the age and normal. - Inflammatory changes in the epithelium -
an increased number of leukocytes; during infection - a significant number of cocci and rods. It is possible to detect infectious agents (indicating the pathogen), for example Trichomonas, yeast. - Suspicion of malignancy.
- Individual malignant cells.
- A large number of malignant cells, malignant neoplasm.
- If minimal changes are detected or if a malignant formation is suspected, it is recommended to conduct testing for oncogenic serotypes of the human papillomavirus.
Only your gynecologist can adequately interpret the results of cytology.
Do not rush to interpret the smear results yourself, as some data may unduly frighten you. What can influence the result?
- In girls under 20 years of age, false-positive results are possible due to changes in the epithelium due to transient hormonal disorders.
- The preparation was not carried out properly: smears were taken during menstruation and are represented by a large number of endometrial cells and blood; the preparations contain spermatozoa; the smear is contaminated with spermicidal and antibacterial creams, lubricant from condoms, ultrasound gel; Before the collection of cytological material, a bimanual examination was performed (contamination of the material with talc).
- The conditions for obtaining the material and preparing the drug were not met.