Complexes with this research
IVF planning Examination for preliminary preparation of a woman for the IVF procedure RUR 12,290 Composition
Miscarriage Identification of the main causes of miscarriage RUR 37,670 Composition
Women's reproductive health RUB 3,610 Composition
IN OTHER COMPLEXES
- Women's safety RUB 1,890
- Pregnancy planning. Cervical screening and STIs RUB 4,450
- Women's check-up No. 2 5,970 RUR
- Entry into IVF RUB 21,660
Carrying out the procedure
First, the obstetrician-gynecologist examines the vagina and cervix in speculums and assesses the condition of the mucous membranes; a digital gynecological examination should not be done before the smear. If the epithelium covers a large amount of mucus, it must be removed. Then the cervix is scraped (exocervix), using an Eyre spatula. After this, a scraping is taken from the cervical canal (endocervix), and the material is collected using a special cytobrush (Cervix Brash). It is inserted into the canal and 4-5 circular movements are performed. After collection, the resulting material is applied to glass, the smear is air-dried and fixed with alcohol or a special preparation (for Papanicolaou examination). The resulting preparations are then placed in a container and delivered to the laboratory. If liquid oncocytology is performed, then the brush is immersed in a liquid fixative, rinsed, and the tip of the brush is removed and left in the fixative.
The next stage of the study is laboratory. Laboratory assistants register the samples received. Then the smears are stained with special dyes (according to Leishman). Liquid cytology preparations are centrifuged or filtered.
The finished preparations are sent to the analytical stage, which is carried out using microscopy. The evaluation criteria are:
- Cell type;
- Cell sizes;
- Inclusions in cells;
- Maturity;
- Features and changes of kernels;
- Cytoplasm.
After evaluating the results, the laboratory issues a conclusion, which is sent to the attending physician.
Detailed description of the study
Cervical cancer is the most common gynecological malignancy in the world. Thus, in Russia alone, more than 17,000 new cases of the disease are diagnosed annually, most often affecting women from 40 to 60 years of age.1 Among the causes of cervical cancer are trauma as a result of numerous abortions or ruptures during childbirth, chronic inflammation and erosion, and hereditary predisposition. Particular attention is paid to HPV or human papillomavirus as a trigger in the development of the disease.
Risk factors also include: • early onset of sexual activity • multiple sexual partners • unprotected intimate contacts • smoking Cytological screening is aimed at the early detection of pretumor and tumor diseases of this localization. Liquid cytology is an alternative to the classic smear for oncocytology, which has a number of advantages: • the material being studied is placed in a special transport liquid, this eliminates the loss of part of the material (when applied to a glass slide, some of the cells may be damaged) • the isolated material can be used repeatedly for the necessary analyzes, in including for immunocytochemical studies • cells are distributed evenly in the liquid medium, in contrast to a smear, where “multi-layering” can be observed
Preparing for the study
The study does not require special preparation, but there are several recommendations that must be followed to avoid getting a false result. The study cannot be performed during menstruation. For inflammatory diseases of the genital organs. If during the examination a woman experiences pain, itching or burning in the vagina.
IMPORTANT! You cannot douche before the test, you must abstain from sexual intercourse for at least 48 hours and you must abstain from urination for 2 hours before the hemotest. If these rules are not followed, results may be inaccurate or altered.
What else is prescribed with this study?
Antigen for squamous cell carcinoma (SCC) (carcinoma of the cervix, nasopharynx, esophagus, ear and other localizations)
8.14. Venous blood 1 day
RUR 2,200 Add to cart
HPV 16/18/31/33/35/39/45/51/52/56/58/59 type, DNA (HPV, PCR, genotyping) scraping, count.
19.57. Scraping 1 day
RUR 1,690 Add to cart
Gynecological smear for flora
16.1. Scraping 2 days
590 RUR Add to cart
Immunocytochemical screening for cervical cancer: p16ink4, Ki67 (prescribed additionally or together with cytological examination of scrapings of the cervix and cervical canal using the BD SurePath FocalPoint LIQUID CYTOLOGY method)
29.21. Scraping 7 days
5 100 RUR Add to cart
Comprehensive study of the microflora of the urogenital tract
170.0. Scraping 5 days
RUB 1,280 Add to cart
Microscopic examination of smear with Gram stain (with Nugent score)
168.0. Scraping 1 day
510 RUR Add to cart
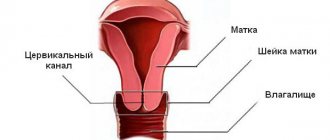
Anatomy
Behind the labia majora and minora is the vaginal vestibule, behind which the vagina is located directly. It is a hollow muscular organ located in the pelvis. The vagina occupies a position between the bladder and urethra in front and the rectum in back. The distal end is attached to the cervix. The cervix is an anatomical formation in the lower segment of the uterus. The cervical canal of the cervix is an anatomical through hole that passes through the middle of the cervix and directly connects it and the vagina. It may be absent if embryogenesis is abnormal; this condition is called atresia. Normally, the cervical canal is filled with mucus, which protects the uterus from the penetration of microorganisms and other foreign agents.
To understand the essence of a cytological study, it is necessary to understand that in different parts of the reproductive tract the organs are covered with different epithelium. On the surface of the vagina and the vaginal part of the cervix there is a non-keratinizing squamous multilayered epithelium, and in the cervical canal there is a cylindrical epithelium. If the cylindrical one extends beyond the canal, this is called ectopia, which is considered a physiological norm and cannot be treated.
Decoding the results
Classification of cytological changes according to Papanicolaou:
- Class 1 – negative result (norm – no atypical cells, cells have the same shape and size);
- Class 2 – morphological changes were detected that appeared under the influence of inflammation of the vagina or cervix;
- Class 3 – there is a suspicion of a malignant process, single cells with morphological abnormalities are found;
- class 4 – individual cells with malignant changes;
- Class 5 – signs of malignant tissue changes were detected.
Microbiological examination of the cervix and cervical canal
When conducting a cytological examination, it is possible to simultaneously carry out microbiological diagnostics. Based on this, a final diagnosis cannot be made, but infectious diseases of the genital tract can be suspected.
- Trichomonas colpitis - when trichomonas are detected;
- Candidiasis (better known as thrush) - when fungi of the genus Candida are detected;
- Bacterial vaginosis – decrease in lactoflora (normal vaginal flora), detection of cocci, gonococci, rods or mixed flora;
- Chlamydia – chlamydia detected;
- Changes in the epithelium under the influence of HPV.
To make a final diagnosis, additional research is necessary:
- Microbiological method – sowing of flora with subsequent determination of the type of pathogen and its sensitivity to antibacterial drugs;
- PCR diagnostics (polymerase chain reaction) is a modern diagnostic method based on determining the DNA of pathogens of infectious diseases.
Additional methods for diagnosing malignant neoplasms of the female reproductive system
In addition to oncocytology, there are other studies to confirm tumor diseases of the female reproductive system. These include:
- Ultrasound examination - carried out using an ultrasound machine, allows you to detect changes in the pelvic organs;
- Hysterosalpingography (HSG) is a method of examining the uterus and fallopian tubes, in which their cavities are filled with a contrast agent and an X-ray or ultrasound examination is performed. Allows you to detect obstruction and structural changes in organs;
- Hysteroscopy is an endoscopic examination of the uterine cavity. The advantage of the method is that it can go from diagnostic to therapeutic (allows minor surgical interventions, such as polypectomy or biopsy);
- Immunohistochemical analysis is a laboratory method for determining the necessary cells using labeled antibodies;
- Determination of tumor markers in the blood - substances that are secreted by tumor cells and are not found normally.
George N. Papanicolaou – Father of Cytology
The content of the article
Cytology would never have arisen if not for one Greek doctor who one day decided to check whether... guinea pigs had their menstrual periods. The doctor who discovered this remarkable diagnostic method was George N. Papanicolaou, who later became a professor at Cornell Medical Center in New York and director of the Papanicolaou Cancer Research Institute in Miami.
The future scientist was born in 1883 on the Greek island of Euboea. Since childhood, Papanicolaou has been interested in natural sciences. In 1899 he began his medical studies at the University of Athens. However, he dreamed of studying natural science in Germany, which was categorically opposed by his father, who wanted his son to become a military doctor. It was this fact that became decisive in the fate of the student.
Inspired by Hertwig, a zoologist from Munich, the student became interested in the question of sex determination in embryos. He managed to get a job as an assistant in the pathology department of a New York hospital. There he planned to learn the secret of the origin of sex by practicing on experimental animals.
At the time, it was widely believed that guinea pigs did not menstruate. However, during Pap research, he discovered that this was not the case. Guinea pigs have menstruation, but it is short-lived and barely noticeable. At the same time, he discovered cyclically changing cells in the vaginal mucus of animals. The Greek doctor wondered if this could be related to processes occurring in the uterus and ovaries, and whether such cells exist in women.
So, George N. Papanicolaou, a man who had never shown much interest in gynecology (at least at first), made the first smears from a woman's vagina, of course not knowing what discovery he had made.
The doctor began his research on his wife, and later received permission to take several smears from patients in one of the maternity hospitals in New York. Several months later, after making countless swabs, he noticed cancer cells in a sample from a young and seemingly completely healthy woman.
Cervical cancer cells
The doctor shared his discovery with the medical community. A group of gynecologists began to conduct tests using all methods available at that time, but they were unable to confirm the results obtained by Papanicolaou. However, the Greek doctor was sure that he was not mistaken. And later the woman actually experienced cancerous changes in the cervix.
Today we know that cervical cancer can take years to develop before it becomes visible.
Pros and cons of liquid-based cytology
The undoubted advantage of the method is its high reliability, which is achieved due to the high-quality medical preparations used, necessary for the analysis, as well as due to the very essence of the method, which implies the absolute entry of the collected biomaterial into the examined space of the microscope. That is, even a small fraction of cells infected with cancer will be detected by the study.
Another important feature of the analysis procedure is that the possibility of distortion of the result by external factors, such as the ingress of foreign bodies (the amount of secretions that, by chance, may come into contact with the sample insignificantly) is significantly reduced.
For reference. Among other things, the liquid substance in which the material is located is a kind of protection against mechanical damage to cells, and this makes it possible to clearly distinguish between healthy cells and those infected with disease.
The advantages of the method also include some laboratory nuances:
- Compared to various methods of analysis, liquid cytology analysis significantly increases the shelf life of a biomaterial sample, which simplifies its transportation for research in the laboratory.
- The biomaterial sample is prepared quite quickly, which reduces the time required to obtain research results.
- During the sampling procedure, the laboratory technician receives a quantity of biomaterial sufficient to conduct several studies at once.
- The study of liquid cytology occurs according to a clearly formed plan in accordance with the established rules of the World Health Organization, which stipulates the same research procedure in various diagnostic centers around the world.