What is bougienage
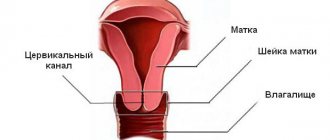
What is it - bougienage of the cervical canal? The procedure is a forced expansion of the lumen of the cervix using special instruments - a bougie. The procedure is recommended for patients with diagnosed narrowing, partial fusion or complete obstruction (atresia) of the cervical canal.
Quite often, bougienage of the cervix is the only way to treat pathology that helps restore reproductive function. In addition, bougienage of the cervical canal is used to treat women during menopause with a diagnosed serosometer.
The manipulation does not pose a risk to the patient’s health if it is performed by qualified specialists using modern equipment designed to solve a specific problem.
Causes of pathology
Partial or complete atresia (fusion) of the cervical canal can be caused by many factors. Most often, a condition requiring bougienage of the cervix is formed as a result of:
- development of endocervicitis;
- poorly performed therapeutic or diagnostic curettage;
- medical abortions;
- cauterization of the cervical canal mucosa with electric current;
- conization.
If the cervix is obstructed, false amenorrhea develops. The menstrual cycle is completely preserved. Endometrial detachment and accompanying bleeding are also present, but due to the closed lumen of the cervical canal, the contents of the uterus are thrown into the fallopian tubes and sometimes into the abdominal cavity. Predisposed women develop endometriosis. It causes severe inflammation and pain.
Cervical stenosis quite often forms after curettage. As a result, the patient develops hematometra, a condition in which blood accumulates in the uterine cavity. If you do not receive qualified medical care, then the next stage is severe inflammation of the uterine cavity, as well as peritonitis.
Indications and features of the procedure
Bougienage is prescribed for the following conditions:
- infectious pathologies (herpes, syphilis, chlamydial infection, toxoplasmosis);
- taking medications for a long time;
- exposure to ionizing radiation on the body;
- carrying out the procedure of curettage of the uterus;
- cauterization of the uterine epithelial layers using electrocoagulation or the use of silver nitrate;
- cancer of the cervix and uterine body;
- abortion;
- endometritis or endocervicitis;
- stenosis or atresia of the cervix;
- hypertrophic scarring.
How and why erosion is cauterized
The procedure is carried out in a hospital setting, using general anesthesia. Local anesthesia is not prescribed because it is ineffective. The type of anesthesia is determined by the doctor after a thorough examination of the patient’s body.
The operation implies that a special instrument, a bougie, will be inserted into the cervical canal. Without anesthesia, the patient would be in pain ,
because it leads to traumatization of the mucous membranes. The bougies increase gradually, otherwise the neck is likely to rupture.
Trauma to the tissue always leads to re-closure of the cervical canal. Correctly performed dilation of the cervical canal guarantees the absence of complications.
Bougienage is not done if it has developed as a result of a malignant process. In this case, more radical operations are necessary. Bougienage is prohibited if the duration of false amenorrhea in a woman is more than six months. In this case, plastic recanalization of the cervix is performed.
Tests must be taken 1-2 weeks before surgery
Preparation
Bougienage of the cervical canal is a gynecological procedure that requires special preparation. It is performed under general anesthesia, since forced dilation of the cervix is a rather unpleasant and painful manipulation.
Before bougienage of the cervical canal, a woman is prescribed the following clinical tests:
- biochemical blood test;
- general blood analysis;
- analysis for sexually transmitted infections;
- colposcopy - examination of the cervix using a special medical device;
- blood for AIDS and syphilis (Wasserman reaction);
- blood for hepatitis C and B;
- coagulogram - the analysis determines the rate of blood clotting;
- microscopy of a vaginal smear and material obtained from the entrance of the cervical canal;
- ECG is a necessary analysis to determine the condition of the heart and select the appropriate type of anesthetic;
- fluorography;
- bacterial culture from the vagina and CC;
- Ultrasound examination of the organs of the pelvic region.
Before prescribing bougienage, a woman must consult an anesthesiologist, who will select the appropriate anesthesia for the patient.
Cost of cervical canal bougienage surgery
The price depends on many factors: the level of the clinic, the type of anesthesia, the need to stay in the ward and inpatient observation. Too low a cost for bougienage of the cervical tract may indicate a low level of medical institution and dubious qualifications of the doctor. An inflated figure is also not always justified, because it consists not only of staff pay and the use of drugs, but also of advertising costs.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: 1717 Date of publication: 10.23.2017
Gynecologists - search service and appointment with gynecologists in Moscow
How to do it
Since bougienage is a medical procedure, it is performed in a hospital setting. Pain relief can be general or local - the choice depends on the degree of narrowing of the cervical canal. If the cervix is completely closed, general anesthesia is used; if the narrowing is minor, then local anesthesia is used. The total time that bougienage takes does not exceed 30 minutes.
The procedure looks like this:
- The woman is placed in a gynecological chair and receives intravenous anesthesia. After this, the gynecologist treats the external genitalia with an antiseptic solution.
- Then a speculum is inserted into the vagina, allowing access to the cervix. If local anesthesia is used, the doctor gives three injections of the selected drug, numbing the working area.
- After the anesthetic has taken effect, the physician inserts the narrowest bougie, dilating the cervical canal.
- Then a tool with a slightly larger diameter is used and then the size of the bougie is increased. Gradually increasing the size of the instruments allows for gentle dilatation of the cervix.
- At the end of the procedure, the gynecologist again sanitizes with an antiseptic solution.
As a rule, after completion of bougienage and complete recovery from anesthesia, a woman can go home. But in some cases, the patient is discharged only after a day.
Reviews
Gynecologists note that in some women even the medical term “bougienage” causes panic, which becomes a reason to refuse surgical intervention. However, you should not be afraid of the procedure. If the question arises about the need for surgery, doctors advise choosing a medical institution where qualified gynecologists practice, and not focusing on the cost of the operation.
Taking preventive measures and committing to a healthy lifestyle can protect the fairer sex from the need for bougienage. Experts warn that the surgical procedure does not help in all cases, and the presence of contraindications makes it impossible to perform it.
According to patients who have undergone bougienage, the procedure is painless thanks to correctly administered anesthesia and gradual widening of the passage. To avoid complications, it is important to strictly follow the instructions of your doctor during home rehabilitation. Women call the most unpleasant consequence of the intervention postoperative discharge, which quickly disappears if an experienced gynecologist handled the dilation.
Postoperative period
The recovery period after bougienage of the cervical canal is two weeks. This is the period required for the cervix to heal completely.
With frequent relapses of atresia, the woman will be recommended to install an artificial alloplastic canal.
The total duration of outpatient therapy after the cervical bougienage procedure is seven to ten days. During this period, the woman is prescribed anti-inflammatory and local wound-healing suppositories.
Early period
After the bougienage is completed, the patient will have to spend several more hours in the hospital. If endometrial curettage was performed at the same time, she will have bleeding similar to menstruation.
Deviations that require immediate medical attention and consultation are:
- increased bleeding;
- severe pain in the lower abdomen;
- increase in body temperature.
If there are no deviations in the condition, then after complete recovery from anesthesia the patient is allowed to go home.
The following appointments are scheduled:
- antibiotics (intramuscular or in tablet form);
- antifungal agents to prevent the development of thrush;
- anti-inflammatory drugs for topical use.
Bougienage of the cervical canal has no effect on pregnancy planning. Fertilization of the egg can also occur in the current cycle if the cause of infertility was cervical atresia.
Prevention of infection
The following measures can be used to prevent cholecystitis:
- timely treatment of inflammatory diseases of the cervix;
- careful management of labor and careful cleaning;
- refusal of uncontrolled use of chemical methods of contraception, as well as vaginal irrigation with aggressive solutions;
- detection and treatment of diseases of the female reproductive system.
To minimize the risk of primary infection, a woman needs to lead a healthy lifestyle. This recommendation especially applies to the gestation period. At this time, it is necessary to avoid infection with infectious pathologies that can affect the condition of the endocervix.
Is it possible to prevent uterine access closure?
It is impossible to predict the fusion of the cervical opening. The transition from the reproductive period to the menopausal period is itself a factor suggesting a change in the condition of the pelvic organs.
From this moment on, the woman should regularly visit the gynecologist (at least 2 times a year) and have a smear for cytology.
During manual examination, the doctor may detect narrowing of the cervical foramen and suggest possible atresia in the future.
This condition can be avoided if you follow simple recommendations throughout your life:
- avoid promiscuous sexual intercourse without the use of barrier contraceptives, as they increase the risk of sexually transmitted diseases;
- treat infectious and inflammatory diseases in a timely manner, as they increase the likelihood of the formation of adhesions;
- use contraceptives to prevent abortions leading to cervical canal injuries;
- reduce the frequency of interventions in the uterine cavity that require cervical dilatation;
- avoid stress that aggravates the menopause;
- observe the rules of personal hygiene.
If during menopause there is dryness in the vagina, burning, strange discharge or other complaints, then you should immediately contact a gynecologist.
After the examination, the doctor will prescribe symptomatic treatment that will help stop the fusion in time.
Women all over the world take hormonal replacement medications, which helps them not only prevent uterine occlusion, but also improve their well-being by getting rid of the symptoms of menopause.
Author of the article
Practicing gynecologist-endocrinologist, certified specialist.
Source
Hormonal changes that occur during menopause affect all organs and systems in the body. The organs of the reproductive system undergo the most changes. And atresia of the cervical canal in postmenopause is, although quite rare, but a natural phenomenon. Is it worth treating this condition and can it lead to any serious consequences?