Among female gynecological diseases there are many pathologies of a viral and bacterial nature. One of these is salpingitis, in which thickening of the fallopian tube occurs as a result of the progression of inflammation. The main danger is that patients develop a complication in the form of obstruction of the oviduct, which leads to the inability to become pregnant.
Quite often, this pathology is diagnosed together with oophoritis, when the ovaries are also involved in the pathological process. In medicine, the disease is called adnexitis, which is better known as inflammation of the appendages. Let's consider how the causes provoke thickening of the fallopian tubes, as well as how treatment is carried out.
Reasons for the development of the disease
The exact causes of fallopian tube cancer are unknown. Some risk factors increase the likelihood:
- Age. Most often, this disease is diagnosed at 50–60 years of age.
- Women who have never given birth or breastfed a child are at increased risk.
- Family history: presence of close relatives (mother, sister, daughter) who have been diagnosed with cancer of the fallopian tube, ovary or breast.
- Mutations in the BRCA1 and/or BRCA2 genes. These genetic defects are hereditary, meaning they are present in all cells of the body from birth.
- BRCA genes encode proteins that are involved in repairing damaged DNA. If their function is impaired, the risk of developing ovarian cancer, breast cancer and some other malignant tumors increases.
- Lynch syndrome is a hereditary non-polyposis colorectal cancer. One of the genes that causes it also increases the risk of developing fallopian tube cancer.
There are also factors that have a protective effect:
- Use of oral contraceptives.
- Childbirth and breastfeeding. The more children a woman has, the lower her risks.
There is a theory that the likelihood of developing fallopian tube cancer increases with chronic genitourinary infections. However, there is no evidence of this yet.
Treatment of hydrosalpinx (sactosalpinx)
Timely detection and treatment of hydrosalpinx (sacto salpinx ) is due to the risk of atrophy of the ciliated (ciliated) epithelium of the fallopian tubes. The rhythmic movements of the cilia that line the fallopian tube help propel the egg through the fallopian tubes into the uterine cavity. With atrophy of the cilia, the risk of ectopic (tubal) pregnancy and infertility increases significantly.
In addition, this pathology is a source of constant infection, where, like in an incubator, ideal conditions are created for the proliferation of bacteria. With the long-term existence of the pathological process and the absence of adequate treatment, adhesions are formed that limit the source of inflammation. Thus, an adhesive process is formed in the pelvis, causing chronic pain (plastic peritonitis), which increases the risk of ectopic pregnancy and infertility.
In case of acute salpingitis and the formation of hydrosalpinx (sactosalpinx, pyosalpinx), hospitalization is necessary. Antibiotics, antihistamines, and cold applied to the pelvic area are prescribed.
Symptoms of fallopian tube cancer
All women experience fallopian tube cancer differently. Often, symptoms are absent or mild, especially in the early stages of the disease.
Possible manifestations of fallopian tube cancer:
- Vaginal bleeding between periods or postmenopause.
- Leucorrhoea is a clear, white or pink discharge from the vagina.
- Pain, feeling of pressure, colic and cramps in the lower abdomen.
- An increase in abdominal size usually occurs when a malignant tumor spreads to the peritoneum and ascites, an abnormal accumulation of fluid in the abdominal cavity, develops.
All these symptoms are nonspecific. Most often, they indicate other diseases that are not related to oncology. To understand their causes, you need to visit a doctor and undergo an examination.
Leading medical specialists see patients at the Medicine clinic 24/7. You can make an appointment at a time convenient for you. The doctor will carefully evaluate your symptoms, conduct an examination and prescribe the necessary diagnostic methods.
Request a call back. We work around the clock
Possible complications
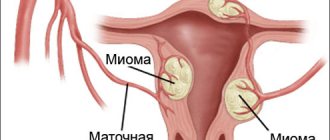
The uterus with the fallopian tubes is equipped with a common circulatory, lymphatic and nerve-fibrous vascular connection.
The functioning of the endocrine system, adrenal glands, thyroid gland and mammary glands depends on their functioning. The most common and significant complications.
- An inflammatory or infectious process can develop immediately or a little later after surgery. It begins with an increase in body temperature.
- Hematomas in the peritoneum or fatty tissue are formed due to impaired hemostasis and blood loss. Possibly due to poor quality of transfusion therapy.
- Sometimes extensive bleeding occurs, especially if medical recommendations are not followed.
- Nausea + vomiting – as a result of anesthesia or the introduction of carbon dioxide during laparoscopy.
- The formation of scars and adhesions is a common occurrence after any type of surgery. Lead to dysfunction of the genital organs and infertility.
- Failure of the hormonal system.
- Recurrence of ectopic pregnancy, formation of a cyst or fibroid.
Complaints of ailments often arise in the postoperative period after a fallopian tube rupture of the following type:
- headache and dizziness;
- emotional instability (tears, irritation, neurosis);
- there is a rush of blood in the upper part of the body;
- hyperhidrosis (increased sweat production).
Symptoms may intensify before the arrival of the first or next menstruation after surgery. A similar clinical picture is not observed in everyone, but only in 40–42% of patients.
Headache is a symptom
2–3 months after rupture and removal of the tube, 35% of women experience menstrual irregularities. The following changes may occur:
- breast enlargement – in 15% of patients;
- engorgement of the glands – in 6%;
- overweight;
- Stretch marks appear on the body, increased hair growth is noted;
- dysfunction and enlargement of the thyroid gland – 26%;
- in rare cases, patients experience complete cessation of ovulation;
- During diagnosis, enlargement of the ovary on the affected side is often observed, which over time undergoes sclerotic changes.
Such symptoms are especially pronounced if both tubes had to be removed during an ectopic pregnancy. The appearance of clinical signs largely depends on the physiological characteristics of the body.
Stages
Staging of fallopian tube cancer is based on the size and other characteristics of the primary tumor (T), the presence of lesions in regional lymph nodes (N) and distant metastases (M). Gynecological oncologists around the world use the FIGO classification:
- Stage I - the malignant tumor is located in only one fallopian tube and has not spread beyond it.
- Stage II —malignant tumors in one or both fallopian tubes that have spread to other pelvic organs.
- Stage III —malignant tumors in one or both fallopian tubes that have spread to the peritoneum (the lining that covers the abdominal cavity and the surface of internal organs) or regional lymph nodes.
- Stage IV - fallopian tube cancer with distant metastases.
What is sactosalpinx?
Sactosalpinx is a disease of the fallopian tube in which watery contents accumulate in its lumen. In most cases, this is a clear, pale yellow serous fluid (hydrosalpinx) or, if infected, pus - such formations are called pyosalpinx.
The development of sactosalpinxes, which can be unilateral or bilateral, is usually associated with a narrowing of the tube due to the adhesive process. In this case, the fluid normally secreted by the walls does not exit into the uterus, but is retained in the cavity of the tube, collecting in one “bag” (simple hydrosalpinx) or several similar formations (follicular hydrosalpinx of the fallopian tube ). In some cases, the contents of the “bag” can periodically pour into the cavity of the tube and the uterus (ventilated hydrosalpinx), but over time it accumulates again.
Diagnosis of fallopian tube cancer
When a woman consults a gynecologist with the symptoms described above, the doctor first performs palpation (feeling) of the abdomen and a gynecological examination on the chair. If the tumor is large enough, it can be detected already at this stage. Then an ultrasound is usually performed, as this is one of the fastest, simplest and most accessible diagnostic methods. Ultrasound examination is carried out through the abdominal wall and transvaginally using a specially shaped sensor inserted through the vagina. This helps to better visualize the pelvic organs.
If a tumor is found, the only way to determine whether it is malignant is to perform a biopsy. A sample of tumor tissue must be obtained and sent to a pathology laboratory for examination under a microscope. There are two options here, depending on the treatment tactics:
- If surgery is planned first, a biopsy is usually not performed before surgery. Surgeons strive to completely remove the tumor tissue and then send it for histological examination. Depending on the result, further tactics are determined.
- If treatment begins with chemotherapy, a biopsy must first be performed. This will help you choose the right antitumor drugs. The doctor chooses the best way to obtain a sample of tumor tissue. The least traumatic procedures are fine-needle biopsy and collection of exudate (liquid that can accumulate in the abdominal or pleural cavity - in case of cancer, tumor cells are present in it).
All types of biopsies are performed at the Medicine 24/7 clinic. Histological examination of tumor tissue and cytological examination of fluids with tumor cells are performed in a modern laboratory by leading pathomorphologists. In addition, modern authoritative professional societies in some cases recommend molecular genetic research of cancer cells. This allows you to quickly establish an accurate diagnosis and prescribe optimal treatment.
A computed tomography scan of the pelvis, abdomen and chest is performed. This study helps to visualize the primary tumor, assess its size, location, and extent of spread to surrounding tissues. Using computed tomography, lesions in the lymph nodes and distant metastases are detected, their location and quantity are assessed.
If metastases in the brain and spinal cord are suspected, magnetic resonance imaging is prescribed.
Positron emission tomography using radiopharmaceuticals that accumulate in cancer cells and PET scanners help detect metastatic foci in different parts of the body.
With cancer of the fallopian tubes, the level of the tumor marker CA125 in the blood increases. But this analysis is not used for diagnosis on its own. In addition to a malignant tumor, the cause of increased CA125 levels can be endometriosis, fibroids, inflammatory diseases, and pregnancy. This method of diagnosing fallopian tube cancer is especially inaccurate in women under 50 who have not yet gone through menopause.
Modern methods of treatment
Fallopian tube cancer is treated in the same way as ovarian cancer. The main methods are surgery and chemotherapy. The choice of treatment tactics primarily depends on the stage and location of the malignant tumor, age, and health status of the woman.
Surgery
Sometimes, before surgical removal of the tumor, minimally invasive laparoscopic interventions are performed in order to more accurately determine the stage (this is not always possible to do from images) and correctly plan treatment.
The extent of surgical intervention depends on the stage of the tumor. The following types of operations are performed (often combined):
- Salpingo-oophorectomy can be performed in the early stages. The affected fallopian tube and ovary are removed from one or both sides. After unilateral salpingo-oophorectomy, a woman retains the ability to become pregnant and give birth to a child.
- Hysterectomy - removal of the uterus and, if necessary, surrounding tissue. Only the body of the uterus (subtotal hysterectomy, or uterine amputation) or the body and cervix may be removed (total hysterectomy, or hysterectomy).
- Removal of lymph nodes in the pelvic area, para-aortic lymph nodes.
- Cytoreductive operations are performed in late stages. Their goal is to remove as much tumor tissue as possible.
Surgical interventions are performed both openly, through incisions, and laparoscopically, using special instruments inserted through punctures. The advantages of laparoscopic operations are that they are accompanied by less tissue trauma, a lower risk of complications, and a shorter recovery period. Robot-assisted surgery is also used.
Chemotherapy
Most often, chemotherapy is given after surgery (adjuvant treatment) to destroy any remaining cancer cells. In most cases, a combination of chemotherapy drugs carboplatin and paclitaxel is used.
In some cases, neoadjuvant chemotherapy is prescribed before surgery. It helps to reduce the size of tumor foci, which ultimately makes them easier to remove and reduces the volume of surgical intervention.
Sometimes, in addition to systemic chemotherapy, intraperitoneal chemotherapy is performed: antitumor drugs are administered directly into the abdominal cavity.
For fallopian tube cancer, targeted hormonal therapy is also used. For example, in some cases, inhibitors of PARP are used, an enzyme that takes part in the repair of damaged DNA, and inhibitors of angiogenesis, the formation of new blood vessels that feed a malignant tumor.
Radiation therapy
Radiation therapy for fallopian tube cancer is rarely used. It can be prescribed after a course of chemotherapy, surgery, or in late stages of a malignant tumor to contain the progression of the disease and reduce symptoms.
Treatment of ascites and peritoneal carcinomatosis in fallopian tube cancer
Peritoneal carcinomatosis is a condition in which cancer cells spread along the surface of the inner lining of the abdominal cavity. Ascites is an accumulation of fluid in the abdominal cavity, which occurs as a result of peritoneal carcinomatosis and damage to the lymph nodes and liver.
For ascites, the primary treatment is laparocentesis (paracentesis), a procedure during which a puncture is made in the wall of the abdominal cavity and fluid is removed. For its constant outflow, peritoneal catheters and port systems are installed. Systemic and intraperitoneal chemotherapy helps reduce ascites.
The Medicine 24/7 clinic uses a modern method of treating peritoneal carcinomatosis - hyperthermic intraperitoneal chemotherapy (HIPEC). The essence of this method is that surgeons remove all tumor foci in the abdominal cavity, and then inject a heated solution of chemotherapy into it for a while. It effectively penetrates all remaining small tumor foci and destroys them.
We will call you back
Leave your phone number
Forecast
Five-year survival rates are estimated cumulatively among all patients with ovarian and fallopian tube cancer. At different stages of the disease they are:
- If the tumor does not spread beyond the fallopian tube - 92%. Unfortunately, only 15% of women can be diagnosed with cancer at such an early stage.
- If a malignant tumor has spread to neighboring organs, to the lymph nodes - 75%.
- For distant metastases - 29%.
Is pregnancy possible after treatment for fallopian tube cancer? Sometimes this disease occurs in women of reproductive age, and they often ask oncologists this question. If the tumor was detected at an early stage, and only one fallopian tube with an ovary was removed, then in the future the woman can become pregnant and give birth to a child. It is also important to understand that chemotherapy drugs affect ovarian tissue, and after a course of antitumor therapy, a woman may become infertile. If you would like to preserve reproductive function, this issue should be discussed with your doctor in advance. He may advise storing the eggs in a cryobank until treatment begins.
Clinic Medicine 24/7 accepts women with ovarian cancer at any stage. We use the most modern types of treatment, the latest anticancer drugs, and work in accordance with the latest versions of international treatment standards.
The material was prepared by gynecologist, oncologist at the Medicine 24/7 clinic, candidate of medical sciences Alimardonov Murad Bekmurotovich.
Prevention
Rejection of bad habits
During the recovery period after a ruptured tube during ectopic pregnancy, it is necessary to adhere to all medical prescriptions.
- Ensure proper care of sutures (if laparotomy is performed).
- At first you cannot take a bath, wash only in the shower.
- Completion of a course of antibacterial, anti-adhesive and physical therapy. Sometimes the use of vaginal suppositories is prescribed.
- Wear compression underwear for a month + you must abstain from intimacy. The beginning of sexual activity must be approved by a doctor.
- Keep a calendar of the menstrual cycle, where the dates of the first and last day of menstruation will be noted.
- Balance your diet - temporarily exclude legumes, whole milk, yeast baked goods, baked goods, cereals and liquids with gas.
- Introduce a daily routine, moderate exercise (walking, swimming, yoga).
- To refuse from bad habits.
- Regularly undergo examination by a gynecologist + routine examination.
- Take oral contraceptives prescribed by a specialist for six months.
- When the body is ready for a new pregnancy, plan conception according to the doctor’s recommendations.