Frequent thrush in women, the causes of which should be determined by a doctor, in most cases requires complex treatment. According to statistics, almost every woman has to deal with fungi that cause thrush. For some, healing occurs very quickly, while others have to undergo treatment for a long time, as the acute form of the disease turns into recurrent candidiasis. Treatment of recurrent thrush is always associated with some difficulties, since the fight against pathology occurs against the background of reduced immunity. Permanent thrush in itself does not pose a particular health hazard, but it does cause a lot of inconvenience.
Causes of constant thrush - very often repeated
Thrush is a disease that causes panic in every woman.
There are very few lucky women who are not familiar with the discharge and discomfort that accompanies candidiasis. During thrush, a woman experiences itching, burning and other troubles that interfere with a full life. Many girls are forced to give up intimacy during exacerbations of candidiasis, becoming emotionally unstable and unsure of themselves.
The situation is especially difficult in patients with frequently relapsing disease.
What can vulvovaginitis be confused with?
Candidiasis is similar to the symptoms of some sexually transmitted diseases: chlamydia, gonorrhea, trichomoniasis, mycoplasmosis, ureaplasmosis. With STDs, as with thrush, itching and burning may occur, discharge of various colors (yellow, green, brownish, cream) with a fishy, sour, rotten or onion odor may appear. With an STD, sexual intercourse becomes difficult. Urination causes burning.
It’s worse if vulvovaginitis is complicated by an STD. If only thrush is present in the body, without STDs, it is quite easy to recognize it by its characteristic white discharge. Also, with candidiasis, there are no rashes on the genitals, which happens with sexually transmitted diseases. Enlarged lymph nodes are not typical for candidiasis. An increase in body temperature is observed with STDs; with thrush, the temperature remains at normal levels.
Why does thrush often recur?
Frequent manifestations of thrush in patients are considered to be more than 3 recurrences of the disease per year. If thrush visits reach 4 or more times in 12 months, it is worth talking about a recurrent form - chronic thrush.
The reasons for frequent recurrences of candidiasis are similar to those for which a woman becomes ill with the acute form:
- insufficient body resistance;
- uncontrolled use of antibiotics;
- lack of hygiene;
- concomitant diseases;
- pregnancy period, etc.
The only difference is that the symptoms are less pronounced.
Decreased immunity
Low immunity is one of the reasons for frequent episodes of thrush, which is why the body cannot cope with the proliferation of pathogenic microflora.
If thrush develops in different places (intestines, vagina, mouth) and does not respond to treatment, then you can suspect that the cause is HIV.
Chronic inflammatory diseases and prolonged bacterial infections also negatively affect the stability of the immune system.
Endocrine system problems
In most cases, diabetes mellitus leads to pathologies of the endocrine system. Since diabetes mellitus entails disruptions in the amount of sugar, the metabolism of fats and proteins is also disrupted. Therefore, diabetes mellitus accompanies thrush in two ways at once. Penetrating into a sweet environment, pathogenic fungi actively feed and reproduce, increasing the risk of developing candidiasis.
In addition, many diseases of the endocrine system can also serve as a good aid for the development of thrush. This is due to the fact that with such pathologies, metabolic processes and hormone balance are disrupted.
Medicines
Taking medications, especially antibiotics, is one of the most common causes of thrush.
Despite the fact that antibiotics are an effective method of treating many dangerous ailments, taking them has side effects. Since the principle of action of antibiotics is not selective, they eliminate not only pathogenic organisms, but also disrupt the natural microflora in the vagina.
Pregnancy
The cause of thrush during pregnancy is the active proliferation of fungi on the vaginal mucosa.
Despite the fact that Candida fungi are present in the body of every woman, but in small quantities, they do not pose any particular danger. But, during pregnancy, fungi actively multiply, which is accompanied by a decrease in immunity
Due to the transformations of the female body during pregnancy, the proliferation of fungi causes inflammation, which is accompanied by the appearance of vaginal discharge, itching and burning.
Thrush during pregnancy requires the fastest and most effective treatment, which was unusual before the birth. Otherwise, it increases the risk of infection of the child during its passage through the birth canal.
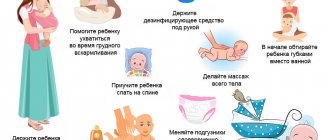
Insufficient hygiene
Today, most women try to take care of themselves as much as possible, especially worrying about the cleanliness of their intimate places. But even such clean people make mistakes, which makes a woman vulnerable to thrush.
To avoid getting into the risk zone, you should remember simple hygiene rules.
Avoid frequent use of sanitary pads or change them frequently
Although pads were designed to absorb menstruation, today a thinner alternative, panty liners, is in widespread demand. But such hygiene products can harm the female body, as they create a humid environment and interfere with heat transfer. Under such conditions, the fungus develops even more actively, increasing the intensity of discharge and causing vaginal infections. If it is not possible to completely abandon daily routines, try to change them at least every 4 hours.
Monitor the composition of lubricants and other piquant means for love pleasures
Often, petroleum jelly and other components of oil-based lubricants can provoke the development of infection. As a safe sexual lubricant, you should use products containing high-quality oils with a neutral pH. In addition, you should not use improvised means that are not intended for lubrication (for example, vegetable fats, cream, etc.) so as not to disturb the acid-base balance of the vagina and not provoke irritation of the mucous membrane.
Avoid vaginal douches
Some women practice vaginal douche as a means of vaginal hygiene. But, this is a dangerous procedure that can lead to bacterial imbalance. In addition, many gynecologists agree that it is the vaginal douche that is the source of diseases of the pelvic organs, as well as thrush. To wash, just use water and neutral soap, then wipe dry with a cotton towel.
Keep your genitals dry after using the toilet
It is very important that a woman’s intimate area remains dry after going to the toilet. To do this, it is enough to use toilet paper after urinating, wiping in the direction from the vagina to the anus.
By following these simple rules and monitoring the hygiene of your sexual partner, you can reduce the risk of developing thrush and other diseases of the genitourinary system.
Age
As medical statistics show, most often thrush manifests itself during moments of hormonal surges. Such moments occur during a transitional period in a girl’s development, pregnancy and menopause.
Representatives of the fair sex from 20 to 40 years old are at risk.
Contraceptives
The use of hormonal drugs as contraceptives can lead to imbalance of hormones in a woman’s body. Therefore, very often patients complain of specific discharge after taking oral medications to prevent unwanted pregnancy.
Most often, the problem is faced by girls whose birth control pills contain an increased dose of progesterone and estrogen. Also, taking such contraceptives increases the amount of glycogen in the vaginal tissues, which promotes the proliferation of fungi.
Thrush every month: what to do?
Chronic thrush is common.
Therefore, a woman has to constantly treat urogenital candidiasis, which can appear almost every month before menstruation. With a chronic disease, periods of calm and exacerbation are guaranteed to occur at least 4 times a year. It is clear that this state of affairs is not caused by candida, although they are the causative agents of the disease.
The reason for the disease becoming chronic is due to a number of factors, the main one of which is the low level of protection of the body by the immune system, and the consequence of this is the chronic form of thrush.
Why does thrush become chronic?
thrush every month The reasons for the development of the chronic form of the disease are related to the general condition of the body.
At the same time, the chronic form does not have the classic pattern of exacerbation and remission of the disease - in some women, exacerbations occur as scheduled every month during the premenstrual period.
Alternatively, patients may complain of an exacerbation of the disease after the holidays, with the onset of the winter season, submitting annual reports at work, etc. In any case, in the chronic form, an exacerbation of the disease should occur no later than 3 months after the next course of treatment.
According to various sources, the chronic form of vaginal candidiasis is observed in 5-25% of all affected women. If it is the fate that more than 80% of female representatives have encountered this disease at least once in their lives, then on average the total percentage of the chronic form of the disease is about 10-20% of all women. Such solid figures are associated with the following factors:
- Thoughtless and uncontrolled use of antibiotics. At the moment, this is a serious problem that leads to the destruction of the immune system. It is worth taking into account the fact that the body gets used to antibiotic drugs, and in order to achieve the desired effect, each time you have to take increasingly stronger antibiotics. The destruction of one's own immunity makes the body defenseless against diseases. Often, such antibiotic lovers have a whole bunch of chronic diseases - in addition to thrush, there are often chronic diseases of the bronchi and gastrointestinal tract. Since the body's resistance is practically zero, such people suffer from acute respiratory viral infections every season with the obligatory exacerbation of chronic bronchial diseases;
- Another actual cause of chronic thrush is the use of hormonal drugs - most often these are birth control pills. Fluctuations in hormonal levels also negatively affect the microflora, while part of this microflora is one of the barriers to pathogenic and conditionally pathogenic bacteria and fungi. The death of bacteria that restrained the proliferation of candida is guaranteed to ensure rapid growth of colonies. Also, in general, the level of immunity drops, so any cold can weaken the body, which in turn provokes another exacerbation of thrush;
- Pregnancy. For many women, thrush became chronic during pregnancy and breastfeeding. This is due to hormone surges, first the hormonal background changes for bearing a child, then for milk production, and the level of immunity during pregnancy is naturally reduced, in general, all this creates excellent conditions for Candida colonies. Against the background of this level of body protection, any dysbacteriosis or use of antibiotics can provoke another outbreak of the disease. By the way, with chronic thrush, exacerbation can occur every month due to hormonal fluctuations before the onset of menstruation. Women experience another surge in the activity of Candida colonies during menopause - changes in hormonal levels also make the body defenseless against infections; as a rule, during menopause all chronic diseases become aggravated;
- Chronic diseases - this factor is also guaranteed to indicate a low level of immunity. Since chronic diseases most often cannot be treated, for example, tuberculosis or diabetes mellitus, AIDS, chronic thrush will be a constant companion to such diseases;
- Cases of chronic candidiasis due to strict diets are no less common among young girls - a weakened body does not have the resources to maintain immunity, so periodic exacerbation of all chronic diseases is inevitable. The result of a strict diet is most often not only lost kilograms, but also acquired chronic thrush. If you do not adjust your diet, which will allow the immune system to recover, then no medications will help get rid of the disease;
- Excessive concern for your own health can also, oddly enough, cause an imbalance in the body. Advertising companies are actively promoting the idea of consuming “live” bacteria, every day. Such an amount of microflora cannot but affect the human microflora, which inevitably changes, and the bacteria themselves come into conflict for a place in the human body. The result of such a process is inevitably dysbacteriosis, and in the meantime candida multiply, filling the vacated space;
- As for the microflora in the vagina, beneficial lactic bacteria, the so-called eubiotics, create an acidic environment in the vagina, which is optimal for candida. Likewise, the acid balance in the vagina is affected by fatty and sugary foods, so it is worth reviewing the basics of nutrition and making it healthy.
Symptoms of chronic candidiasis
- Small scale of damage to the mucous membrane - chronic candidiasis does not go beyond its limits;
- There is slight swelling on the mucous membrane;
- The color of the genitals indicates slight redness;
- The mucous membranes are dry, there is no moist shine, and cracks appear on the surface of the tissues;
- A small amount of vaginal discharge;
- Alternatively, the chronic form of thrush can occur with virtually no discharge and does not cause concern.
Treatment
When prescribing a test to detect this disease, it is better to take a blood test - a smear test may give incorrect results. It is also necessary to check the vaginal mucosa for the presence of other diseases - often chronic thrush accompanies sexually transmitted diseases, so if candidiasis appears every month, then a visit to a specialist is required.
https://www.youtube.com/watch?v=po46NB8tFZY
As for therapy, it is carried out according to individual schemes - this is always a long process. You won’t be able to get rid of the chronic form by taking one pill.
Most often, the patient is prescribed vaginal suppositories, which are placed in the vagina several times a week for several months; the doctor must accurately select the dosage of the drug.
Treatment cannot be delayed - as soon as signs of the disease appear, you must consult a doctor:
- Itching in the genital area;
- Burning sensation both during urination and during sexual intercourse.
This state of affairs indicates the need for an urgent visit to an obstetrician-gynecologist.
Source: https://womanjournal.org/zdorovie/zabolevaniya/1703-pochemu-molochnica-stanovitsya-hronicheskoy.html
What to do if thrush recurs frequently
To avoid frequent manifestations of thrush, a woman must visit a gynecologist, undergo a full examination and get tested. After a clear diagnosis, the patient is advised to follow the recommendations and prescriptions of the attending physician.
Since thrush is an infectious disease, it must be eliminated using complex methods. In addition, it is important to immediately get rid of the causative agent of candidiasis, then monitor the effectiveness of treatment. At the final stage, re-infection must be avoided.
Drug therapy for fungal infection
Drug therapy for thrush is a set of measures that include hygiene procedures, taking medications, and observing dietary restrictions.
When prescribing medications to a patient, the doctor must take into account the severity of the disease and the picture of the inflammatory process. Therapy can be adjusted taking into account the individual characteristics of the female body.
Today the pharmaceutical market is very diverse, so buying drugs for thrush is not difficult. But, you should not self-medicate. Not all drugs can be combined with each other. Only a gynecologist should prescribe a treatment regimen.
Drug therapy can be carried out with antifungal agents in combination with immunostimulants and drugs that get rid of the root cause of thrush.
Vaginal suppositories are widely popular:
Your doctor may prescribe vaginal tablets, such as:
Local remedies in the form of creams and ointments, such as nystatin ointment, Ginofort, Miramistin, etc., can also be prescribed.
Physiotherapy
If thrush does not respond to treatment, especially in its chronic form, the doctor may recommend physical therapy to the patient.
Most often, magnetic therapy and laser treatment are used to treat thrush. Electrophoresis using zinc and mud therapy are also considered highly effective.
The main goal of physiotherapeutic treatment is to increase local immunity in the vagina.
Immunity Boosters
Since thrush often develops in women with insufficient immunity, patients are often included in the therapeutic course of immunostimulants.
In order to increase the body's resistance, doctors recommend:
- complexes of vitamins and minerals (Vitrum, Alphabet, magnesium preparations);
- restorative agents for vaginal microflora and elimination of intestinal dysbiosis (Linex, Bifiform, Hilak);
- homeopathic medicines;
- herbal preparations.
If you skip this point of treatment, the thrush will quickly worsen and the woman will begin to be bothered by discomfort and discharge.
Restoration of microflora
Since Candida fungi destroy the upper layer of the epithelium, it is very important to take measures to restore it. Otherwise, taking lactobacilli will not be justified; beneficial microorganisms will die after 7 days.
Today, the following medications are most often used to restore damaged microflora:
- Gynoflor, Pimafucin, Terzhinan (in the form of vaginal tablets);
- Bifilakt, Lactobacterin, Vagilak (in the form of suppositories).
On average, the duration of treatment varies from 3 to 14 days, depending on the severity of the disease and individual characteristics.
For recurrent forms of thrush, it is also recommended to take general medications in the form of tablets, Diflucan, Fluconazole. It is advisable to take such drugs twice with an interval of 7 days.
Diet
During the treatment of thrush, patients are advised to exclude from the diet foods that have a beneficial effect on the development and reproduction of fungi.
So, it is advisable to completely abandon:
- spicy and pickled foods;
- alcoholic drinks;
- whole milk;
- sweets;
- yeast-based baked goods;
- fresh baked goods;
- bananas and grapes.
Every day it is useful to eat fermented milk products, fresh fruits and vegetables, and garlic.
As a rule, there is no need to reduce caloric intake.
Sanitary pads and tampons: risks of candidiasis
Tampons, pads, wipes and other intimate hygiene products are gaining increasing popularity due to their practicality. But, according to some doctors, such hygiene products can provoke the development of diseases of the female genitourinary system.
It has been proven that tampons can trigger the development of toxic shock syndrome. Also, if the tampon is inserted incorrectly, microcracks can form in the mucous membrane.
To avoid such complications, it is enough to use tampons as intended and only during menstruation.
The wide variety of sanitary pads has made them an integral part of the lives of many women. Since many ongoing studies have not yet clearly established whether sanitary pads contribute to the development of thrush, there is no reason to prohibit the use of such hygiene products. Therefore, if a woman has no contraindications, it is safe to use pads, including daily ones.
Advice from immunologists on the treatment of recurrent vaginal candidiasis
The main reason for the development of recurrent candidiasis is reduced immunity. In order to increase the period of remission, you need to contact an immunologist. He will determine the reason why the immune system cannot cope with the disease and prescribe a course of therapy. Experts recommend:
- Complete treatment. This will help reduce the likelihood of recurrence of the pathology.
- Eliminate the influence of provoking factors.
- Eat properly. The diet should not include harmful foods, such as fast food or those with a lot of flavorings and carcinogens.
- To refuse from bad habits. Alcohol and smoking negatively affect not only the lungs and liver. They have a bad effect on vaginal microflora and immunity.
- Avoid sexual intercourse for the duration of treatment.
- Do not use hormonal agents or antibiotics. In cases where treatment of another disease is impossible without these drugs, it is necessary to take drugs to maintain microflora.
- Follow the rules of intimate hygiene.
It is much more difficult to cure the recurrent form of vaginal candidiasis, in contrast to the acute form.
For this purpose, a complex of medications is prescribed, the main ones being antifungal. Their main advantage is the possibility of local influence. The drugs are also available in the form of ointments and creams. They have no side effects and are easy to use. The form of the drug allows the active substance to quickly reach the site of the pathological process and act directly on pathogenic microorganisms. This helps to achieve the desired effect faster.
Reviews
Elizaveta, 22 years old
“Since I have known thrush for a long time (more than 3 years), I have tried various means to eliminate the disease - all without much result. But, having changed many gynecologists, one day I found an intelligent specialist. He prescribed me to take herbal infusions in the form of tea and for douching. In addition, I was prescribed Pimafucin suppositories. After just half a year, there was no trace left of my chronic form of thrush!”
Olga, 36 years old
“My salvation is any fluconazole-based products. Since thrush worsens almost every month, the medicine cabinet is filled with all kinds of suppositories, tablets and creams containing the active ingredient fluconazole. After the first day of treatment, I managed to get rid of the symptoms of the disease. I continue therapy for 5-7 days.”
Daria, 26 years old
“The doctor structured my treatment in 2 steps: immediately taking antifungal drugs, then restoring the microflora. I found a great remedy for myself - Laktozhinal. This drug is not only good for recovery, but also perfectly increases the resistance of local immunity. After this therapy, I got rid of frequent visits from candidiasis, and for 1.5 years I have been living a full life without discharge or discomfort.”
Why does thrush come back again and again?
The question of why thrush comes back is faced by approximately half of the people who have ever struggled with the disease, because at the present stage only one tablet can defeat the fungus. This happens most often because the treatment was aimed at eliminating the symptoms of the disease. While the cause that caused these symptoms remains in the body, and continues to bloom wildly.
The most common causes of candidiasis
The disease is caused by Candida fungus, which is present in small quantities in the vagina of even a healthy woman. It develops rapidly only under favorable conditions.
These factors include:
- antibiotic treatment;
- violation of hygiene of intimate areas;
- sexual infections;
- dysbacteriosis;
- taking oral contraceptives;
- hormonal changes;
- poor nutrition (lots of flour and sweets in the absence of fermented milk products and fruits);
- weakened immunity;
- reduced body resistance.
Vaginal candidiasis is a very common phenomenon, with which half of women have encountered it at least once. The causes of frequent thrush can be varied, and it is often difficult to determine the trigger. To do this, tests are taken and an examination is prescribed.
The reason for the recurrence of the disease in a woman can also be a violation of the rules in the intimate sphere of life:
- use of low-quality condoms and lubricants;
- wearing synthetic underwear (especially in hot weather);
- frequent change of sexual partners;
- use of unsuitable personal hygiene products with an aggressive effect on natural microflora;
- frequent douching, which washes away the natural microflora of the vagina;
- polygamy of the partner and his failure to comply with the rules of personal hygiene.
For your information! Men also experience thrush, which most often affects the head of the penis. As a carrier of the fungus, a partner can infect a woman during sex without a condom.
What to do if thrush recurs or torments constantly? This form of the disease is recurrent and requires qualified treatment.
Thrush before menstruation
Fungi of the genus Candida are present in the body of most women. They are detected during laboratory testing of a smear, but usually do not cause any discomfort. Their growth is inhibited by beneficial microorganisms that inhabit the vagina.
In the second phase of the cycle, girls experience a change in hormonal levels. After ovulation, progesterone is produced, which suppresses muscle contractility and can suppress the immune system. This is necessary so that in the event of conception, the protective system of the female body does not perceive the fetus as a foreign object. Even a slight decrease in immunity in some patients can cause a relapse of vaginal candidiasis.
Statistics show that most often episodes of the disease appear in the autumn-winter period. Pathology can occur in young girls and girls who are not sexually active. Women during menopause also experience relapses, but due to the fact that the amount of estrogen decreases and the vaginal microflora changes.
Disease categories
Persistent thrush, which makes itself felt often, can be of two categories, into which the disease is conventionally divided:
Persistent
This form is characterized by strong manifestations. The Candida fungus develops, making itself known with vivid symptoms that are simply impossible not to notice.
Recurrent
In this form, the manifestations of the disease are mild and the symptoms of the disease are blurred. Some discomfort occurs, but does not cause significant problems. In this case, only one symptom can clearly manifest itself.
This form of the disease is fraught with danger precisely in the absence of symptoms. A woman may not even be aware that she has the disease and, as a result, may not seek medical help. At the same time, candidiasis continues to develop and the situation becomes already advanced.
For your information! At least 5 out of 100 women have frequent thrush.
Routes of infection
It is quite easy to become infected with Candida fungus, because it is found everywhere. A person usually becomes infected with opportunistic fungi. It is possible that more pathogenic strains can penetrate and cause the disease.
The main routes of penetration of the fungus:
- intrauterine through amniotic fluid,
- when passing through the birth canal,
- when applied to a breast on which fungi are found,
- household route (infection occurs through hands, kisses),
- penetration with meat, vegetable, fruit, dairy foods,
- carriers are young domestic animals,
- sexual intercourse, including oral sex.
Candidiasis is often a side effect of taking antibiotics. The most common complication is amoxicillin, an antibiotic from the penicillin group. Women who take antibiotics too often for any cold are at greater risk. It is they who have very severe thrush and diarrhea. With immunodeficiency, invasive candidiasis spreads not only to the vaginal area, but also to the intestines. The disease also occurs against the background of hormonal imbalances, for example, due to oral contraception.
Treatment: effective and mandatory
Since it is impossible to completely eliminate the fungus from the body, during treatment the goal is to take control of the disease and reduce the activity of the causative agent of candidiasis. In a normal state of immunity in a healthy woman, fungi are suppressed by the defenses of the body itself. Decreased immunity leads to Candida activity and the return of the disease.
Goals of therapy:
- Sanitation of foci of infection.
- Restoration of healthy microflora (not only in the vagina, but also in the intestines).
- Bringing local vaginal immunity back to normal.
The course of treatment usually begins immediately after the end of menstruation. This approach is based on the natural decrease in local immunity during this period, but in case of severe symptoms that greatly bother the woman, treatment should begin regardless of the day of the cycle. Duration of therapy in most cases: from one and a half to two weeks.
To treat acute or chronic forms, the doctor selects a set of measures:
- antifungal drugs;
- means to enhance immunity;
- preparations to restore healthy microflora;
- physiotherapy, etc.
For your information! When the disease occurs against the background of other health problems, medications should be selected for their treatment as well.
Drug therapy for fungal infection
Treatment of thrush must necessarily include one of the means of combating the fungus. Among the most popular drugs that are often prescribed are the following:
- Fluconazole;
- Ketoconazole;
- Pimafucin;
- Migentin and others.
Treatment with these drugs is carried out as prescribed by the attending physician and in strict accordance with the instructions for the drug. Medicines to eliminate candidiasis can be prescribed by your doctor orally and for topical use. In case of unexpressed symptoms, how to treat persistent candidiasis is determined only by a doctor. Systemic agents, as well as local ones, are selected individually in accordance with the treatment regimen.
Physiotherapy
As part of a set of measures for the treatment of candidiasis, a woman may be advised to undergo physiotherapy. They act as an adjunct to primary therapy and may include:
- laser use;
- electrophoresis;
- magnetotherapy.
The use of physiotherapeutic methods of influence is aimed at:
- elimination of fungi that cause candidiasis;
- normalization of the internal environment of the body;
- stimulation of the immune and nervous system.
Some serious diseases are contraindications to the use of physiotherapy. These include: severe hypertension, cancer and others.
Immunity Boosters
To strengthen the immune system, the doctor prescribes immunomodulators. These funds are designed to support the body and improve its resistance to infections.
Among the means that help strengthen the immune system are preparations based on medicinal plants:
In addition to plant-based medicines, women are prescribed vitamin complexes. For example, Duovit, Vitrum and others
Restoration of microflora
The pharmacy chain offers means for restoring normal microflora. In order for the drug to normalize the balance of beneficial microorganisms, it must be selected individually for each woman.
When making a prescription, the doctor takes into account:
- presence of other diseases;
- form of the disease;
- presence of complications;
- the state of the microflora before the start of therapy;
- intensity of development of pathogenic microorganisms.
In a set of measures, both vaginal probiotics (in the form of suppositories) and preparations for oral administration (in the form of capsules or tablets) can be recommended. The most effective probiotics are those containing lactobacilli.
For your information! In a healthy woman, 90% of the vaginal microflora is made up of lactobacilli, 9% is bifidobacteria, and only 1% is opportunistic microflora.
Diet
If thrush in women is frequent, then it is recommended to make adjustments to your diet. Significantly reduce, or better yet eliminate completely, the following products:
- alcohol;
- sweets;
- bakery products.
Such a diet is not strict; it will help you recover faster, being part of the course of treatment. In the future, it is also advisable not to consume a lot of sweets and baked goods, so as not to create favorable conditions for the return of the disease.
At the same time, we should not forget about fermented milk products, vegetables and fruits. Their use, on the contrary, helps maintain a normal microflora balance and maintain a strong immune system.
Sanitary pads and tampons: risks of candidiasis
If the use of modern sanitary pads is not performed correctly, then their rare change can play the role of a trigger for the development of the disease. If the rules for using hygiene products during menstruation are violated, the risk of developing fungus increases significantly.
The situation is even more serious with tampons that are inserted internally. If you are prone to chronic thrush, it is better to avoid this personal hygiene product. Panty liners are also undesirable, as they disrupt air circulation and contribute to the development of the greenhouse effect - a favorable environment for candidiasis.
Treatment
The first thing you need to do is contact a gynecologist. Many patients try to cope with vaginal candidiasis on their own by purchasing over-the-counter treatment products at the pharmacy. Incorrectly selected drugs turn out to be ineffective against pathogens, resulting in a relapse every month. To choose a medicine that will really help, you need to take a smear and determine the sensitivity of fungi to antifungal substances.
Typically, patients are prescribed complex therapy, which involves oral administration of medications and local use of antiseptics. In addition to antifungal medications, the doctor recommends the use of drugs to increase the body's resistance. They are prescribed in the form of suppositories for vaginal use or tablets.
Lifestyle and diet play a big role in the treatment of recurrent thrush. It is recommended to give up alcohol, especially beer. You should not indulge in sweets and baked goods. It is necessary to give preference to vegetables, fruits, fermented milk products, and high protein dishes. It is important to monitor the functioning of the intestines, since the immune status of the body depends on its functioning.
A prerequisite is personal hygiene. Panty liners become a good breeding ground for pathogens, so it is better to discard them. You should not wear synthetic underwear and wash with regular soap. It is necessary to give preference to breathable fabrics and use special products for intimate hygiene.
Thrush begins with itching
Prevention of frequent thrush
If you are prone to frequent candidiasis, efforts should be directed toward preventing relapses. Simple preventative measures can help with this:
- complete treatment of any infectious diseases;
- careful adherence to personal hygiene;
- balanced diet with a minimum amount of sweets;
- refusal of panty liners and tampons;
- do not constantly use antibacterial products for intimate hygiene, as they eliminate healthy microflora;
- responsible choice of underwear and clothing (to prevent the development of the greenhouse effect);
- maintaining a healthy lifestyle, including hardening, physical activity and walking;
- using condoms when having sex with a new partner;
- taking oral contraceptives and other drugs that can affect the vaginal microflora only as prescribed by a doctor.
The fungus is highly resilient and remains in a woman’s body even after treatment. At the same time, it may not be determined in the laboratory, but may manifest itself when favorable conditions arise. For a complete recovery, you must follow your doctor's recommendations and not self-medicate.
Important Tips
In most cases, when problems of an intimate nature arise, women do not run to be examined by a gynecologist, but begin to actively storm various forums, asking their new friends and acquaintances about how they dealt with this problem. In some cases, their answers can indeed help, but we should not forget that among them there are no specialists who have studied this disease for years. They can judge it only based on their own experience of fighting the disease, and therefore their opinion can never be objective.
In a number of issues, they are certainly able to advise a practical solution. Among these, for example, is advice to change the intimate hygiene product that a woman uses. It has been noted that thrush can most often occur periodically in cases where a woman simply incorrectly identified the cause of its development. The products a woman uses to cleanse herself must be specifically designed for this area. Regular shower gels, soaps and shampoos can harm the vaginal microflora, which is only necessary for fungus.
The choice of candles is also not ignored. Here the questions concern not only the choice of the most effective and popular suppositories, but also their cost. In fact, this is not such a wrong question either. Many famous, advertised candles are not as effective as they promise to be. And experienced women already know about this. Those who experience thrush most often have tried a whole series of suppositories and can somewhat judge their quality and ability to help. Even doctors note the fact that cheaper candles are better than expensive ones.
Some advise taking additional tests, which is also a good recommendation for young ladies.
An infection that may be in the patient’s body will help him with this. In this case, it is necessary to carry out complex treatment in order to achieve the desired results and get rid of candidiasis forever.
Causes of persistent thrush
There are many factors why thrush returns. A relapse of the disease can be triggered by an interrupted course of therapy, failure to comply with basic aspects of personal hygiene, untreated endocrine pathology and a decrease in the body’s overall resistance to bacteria, fungi or viruses.
After sex
Many women complain that they have constant thrush after sex.
A number of reasons may contribute to this:
- Some men are carriers of Candida fungi, although they themselves do not experience any clinical symptoms or signs. During any unprotected sexual intercourse, microflora is exchanged between partners, including pathogenic ones. Thus, the woman will receive a return of the disease after each sex, so examination of her regular partner will be the right decision for a speedy and complete recovery.
- The use of barrier contraceptives (spermicides such as Farmatex or Benatex, condoms) can also provoke the occurrence of recurrent candidiasis. Some chemicals included in contraceptive barrier products cause changes in the acid-base balance of the vagina, irritate its mucous membrane and contribute to the development of a localized allergic reaction. The resulting local decrease in immunity activates opportunistic flora, which includes yeast-like fungi.
- Involvement in non-traditional types of sex, especially without the use of protective equipment, contributes to contamination of the vagina, which later manifests itself as chronic or recurrent thrush.
During pregnancy
During pregnancy, the female body undergoes significant physiological changes, which in one way or another can activate pathological processes.
- Sluggish HIV infection, chronic somatic diseases of the endocrine (for example, diabetes mellitus), cardiovascular system, chronic leukemia can worsen during pregnancy. As a result, the immune system also suffers, which becomes unable to fight the saprophytes of the human body.
- Hormonal levels change. To maintain pregnancy, the body begins to intensively produce a special hormone - progesterone, which, in addition to performing its main function, promotes a specific change in the epithelial membranes of the internal organs of the reproductive system. They become loose and juicy, local blood flow increases, and the acidity of vaginal secretions increases, which is why pregnant women are more susceptible to thrush.
- Constant thrush often occurs during pregnancy as a consequence of chronic constipation. When carrying a child, a woman's intestines may malfunction. And stagnation of feces, in turn, causes increased fermentation and rotting of digested foods, which ultimately contributes to dysbiosis and excessive proliferation of fungal colonies in the intestinal lumen and vagina.
- Iron deficiency anemia often accompanies pregnancy and leads to hypovitaminosis, degenerative changes in the skin and mucous membranes. The result is a relapse of genital candidiasis.
Before your period
Some girls and women are concerned about exacerbations of thrush before or after menstruation.
There are reasons for this:
- Before menstruation, there is often a slight hormonal shift that can affect the development of candidiasis.
- During menstruation, ideal conditions are created in the vaginal cavity for the reproduction and activity of fungi and bacteria.
- The use of intimate hygiene products (pads or tampons), which contain fragrances and some chemicals, negatively affects the biocenosis of the vagina, as a result of which thrush occurs.
- Non-compliance and violation of rules in personal hygiene, rare change of underwear.
Elimination of causes
Some women, who have once dealt with frequent thrush, become more experienced and wiser, and their advice is worthwhile. The problem may even lie in the food you eat!
It is worth eliminating at least for a while the consumption of:
Another negative factor for the vaginal microflora, as some participants in the conversation emphasize, is douching. In order to get rid of thrush, douching with certain solutions is recommended. However, some ladies tend to overdo it. The fact is that douching is allowed twice a day, but no more than three days, since during further procedures healthy bacteria will be washed out of the vaginal microflora, which protect the woman’s body not only from thrush, but also from some other diseases. Such advice can also be considered adequate and useful.
But you should not believe the dosages indicated on the Internet, as this may lead to complications or cause side effects. For such information, and a complete list of recommendations, you should continue to contact your gynecologist.
And of course, various folk remedies are offered for a more successful fight against thrush:
- One of the most effective methods is the use of cotton swabs or bandages, rolled up independently and soaked in white wood oil or a mixture of one teaspoon of aloe juice and the same amount of melted honey. It is necessary that the liquid is completely absorbed into the tampon, which then needs to be inserted into the vagina. It's best to do this before bed. At the same time, to avoid leakage, it is advisable to use a menstrual hygiene product - a pad.
- Douching can be done with an infusion of fillet and iron ore herbs. The solution is prepared for one use. It is worth pouring one teaspoon of each herb into a container, and then pour a glass of boiling water. Leave for some time. It is enough to wait until the broth has cooled to room temperature, then you can use it for its intended purpose.
Thrush does not always live on the genitals; sometimes the location of the fungus is the woman’s intestines. In this case, you need to check its condition. It may turn out that in the field of gynecology candidiasis was cured, but due to the presence of spores in another place, the disease arose from time to time. Typically, to treat thrush in this case, dietary supplements are prescribed, as well as agents that will help restore the intestinal microflora.
In most cases, when genital candidiasis is detected in a woman, doctors prescribe only local antifungal drugs to treat it. Or the patient herself, without going to the hospital, self-medicates on the advice of friends or close relatives, which ultimately leads to a relapse of the disease. Remember, without finding out the main cause of persistent thrush, it is impossible to carry out adequate and effective treatment.
Treatment: what to do with recurring thrush?
And now in detail about how to treat recurrent thrush...
Tips and recommendations for diagnosis and prevention
To avoid relapses in the future, a woman should know what to do if she has persistent thrush:
- Before starting treatment for a pathology, it is necessary to find out its root cause. That is, treatment of the underlying disease should come to the fore, and only then drug correction of vaginal dysbiosis.
- It is mandatory to involve a regular sexual partner to undergo examination in order to exclude candidiasis in him.
- To avoid thrush, it is recommended to carefully monitor intimate hygiene and not use aggressive products or laundry soap. During menstruation, hygiene products should be changed regularly.
- With any long-term antibacterial therapy, the intestinal and vaginal flora must be protected by pro- or prebiotics.
- It is advisable to exclude foods containing easily digestible carbohydrates, smoked meats, blue cheeses, confectionery products, alcohol and marinades from the diet.
- If unpleasant symptoms appear, you should promptly consult a doctor for help.
Drugs and medications
Itraconazole, Nitrofungin, Fluconazole are systemic agents of the azole series. After their use for a short course or within three days, 85% of patients eliminate yeast-like fungi.
Topical medications include Terzhinan, Hexicon and Clotrimazole, which are available in the form of vaginal tablets or suppositories. As a rule, as part of complex therapy, a ten-day course is sufficient to sanitize the vagina. You need to use one suppository intravaginally at night.
One of the stages of therapy is the elimination of dysbiosis with the help of intestinal and vaginal probiotics: “Linex”, “Bifiform”, “Acilact”, “Bifidumbacterin”. The course is at least 14 days.
To increase the body's defenses, you can use echinacea extract, alcohol tincture of eleutherococcus, "Imudon". The duration of their use should be at least 4-6 weeks.
Symptoms of the disease
Candidiasis is caused by candida, of which there are more than 200 species. Vaginal and other internal candidiasis are often caused by the microorganism Candida albicans.
With vulvovaginitis, a woman discovers:
- cheesy white discharge from the vagina,
- swelling of the mucous membranes,
- redness of the mucous membrane,
- itching or burning may occur,
- there is a sour smell,
- there is discomfort when urinating,
- Possible pain during intercourse.
Urogenital candidiasis can be transmitted sexually. When treating thrush, a woman needs to treat her partner as well. If advanced thrush is detected, it is necessary to pay attention to other organs: intestines, bladder.
With intestinal candidiasis, the patient may notice increased gas formation, white flakes in the stool, and frequent diarrhea. The disease is usually a side effect of severe dysbiosis, in which beneficial microflora dies and pathogenic microflora, on the contrary, multiply.
Sometimes treatment does not produce results, this is most often due to the fact that complex treatment is necessary. Complications with candidiasis occur if:
- the patient has a weakened immune system, it is necessary to do an immunogram,
- in addition to infection with the Candida fungus, other pathogens are present in the genital tract (Trichomonas, chlamydia, ureaplasma, etc.),
- the focus of the disease is in the large intestine,
- the mucous membrane is damaged, the membranes will need to be restored,
- the partner is also infected, the husband may need to be sanitized,
- decreased estrogen levels.
Complex treatment is aimed at restoring the body’s defenses and removing candida fungi from those organs that are the primary focus. During therapy, topical use of antifungal drugs is continued.
What causes thrush to appear periodically?
A disease that often repeats over a long period of time is called chronic. This also applies to thrush (vaginal candidiasis). If acute outbreaks are observed, alternating with remission, 3-4 times a year, then most often the disease is chronic. But there is no need to be alarmed that constant discomfort will continue to accompany the girl. It’s just that the very nature of fungal infections is such that incomplete or insufficient destruction of them is not effective. This is due to the rapid multiplication of the infection. Under such conditions, a repeated set of symptoms appears within a few days. But it is possible that a re-exacerbation will occur in a month.
Why do so many women suffer from this disease? Any gynecologist can answer this question. Every day, they encounter patients suffering from this disease. And these, out of the entire flow of ladies, amount to up to 25%. Thrush appears due to a whole range of reasons. It is very difficult to pinpoint exactly what influenced the appearance of fungal microorganisms. This often requires a large amount of research and consultation with a gynecologist. Thrush occurs, most often from Candida albicans. This fungus does not pose a big threat. Primary infection, if you consult a doctor in a timely manner, can be quickly and easily treated. After all, most pharmaceutical antifungal drugs are effective in combating this virus.
But often, recurring thrush may not always be caused by albicans. It is estimated that more than a third of patients who have repeated symptoms of candidiasis develop other, complex subtypes of infections. In the first stages of development of recurrent thrush, doctors are prone to the theory of “insufficient or ineffective treatment.” Only laboratory studies can confirm or refute their guesses. And if the pasev tank indicates a different type of fungal presence, then this does not predict anything good for the patient. After all, most of the drugs that deal with Candida albicans will not be effective.
Difficulty in identifying factors that repeatedly provoke thrush
Only a doctor can understand the question of what caused a recurrent or even chronic disease. This is very difficult to do. The specialist needs to fully understand the intricacies of his patient’s daily life. Factors of a more personal nature are also taken into account. These include intimate hygiene and sexual activity. The number of factors influencing the recurrence of thrush is very large. Most often, the main ones are:
- Reduced level of immunity. It may be associated with: the development or consequences of other chronic diseases, a lack of vitamins and microelements, as well as a negligent attitude towards one’s own health.
- Susceptibility to fungal infections. This “sensitivity” is sometimes the main cause of not only thrush, but also other diseases.
- Chronic diseases. There are a lot of varieties of these. The most acute and dangerous are HIV and diabetes.
- Allergic tendency of the patient.
- Sexually transmitted diseases. They may be caused by neglect of contraception or a woman's promiscuous sex life.
- Hormonal surges caused by diseases or the use of medications.
It is necessary to conduct sexual activity with extreme caution. Even having one, permanent sexual partner can affect the return of the disease to the girl. So, if one person undergoes treatment, the “other half” of the infected person should also undergo it. Even modern methods of contraception cannot provide a girl or man with complete safety from candidiasis infection.