Postpartum period
(syn.
puerperal period
) - a period that begins after the birth of the placenta and lasts 6-8 weeks, during which the changes that arose in the woman’s body during pregnancy and childbirth undergo involution.
Some signs that allow one to distinguish a woman who has given birth from one who has not given birth remain for life. Thus, the external uterine pharynx becomes slit-like, the cervix takes a cylindrical shape, the folding of the vaginal mucosa decreases, it becomes more capacious, the size and shape of the mammary glands changes, etc. Along with the processes of involution, most expressed in the genital organs, endocrine and excretory functions of the mammary glands. Certain changes occur in the endocrine, nervous, cardiovascular and other systems of the body. A feeling of motherhood appears. A woman during this period is called a postpartum woman. Rice.
1. Schematic representation of the process of involution of the uterus, the formation of the internal uterine os and the cervical canal (sagittal section of the pelvis): a - the birth canal and the uterus immediately after childbirth; b - birth canal and uterus on the second day after birth (reduction in the size of the uterus, formation of the internal uterine os). The greatest involutive changes occur in the uterus. Immediately after birth, the uterine fundus is located 4-5 cm below the navel (or 12-15 cm above the pubic symphysis). The body of the uterus is adjacent to the anterior abdominal wall and retains greater mobility due to the stretching of the ligamentous apparatus and a decrease in its tone. The fundus and upper part of the body of the uterus (approx. 5 cm) have the greatest thickness in a contracted uterus. Contractions in the area of the isthmus and cervix immediately after childbirth are little expressed (the thickness of their walls is about 0.5 cm), they develop only at the end of the postpartum period. Immediately after birth, the diameter of the internal uterine pharynx is 10-12 cm, which allows, if necessary, to insert a hand into the uterine cavity, remove retained parts of the placenta, check the integrity of the walls of the uterus, and massage the uterus with a fist. By the end of the first day after birth, the internal uterine os is traversable for only two fingers, and after 3 days - for one finger. Such rapid formation of the uterine os is due to contraction of the circular muscle fibers surrounding the internal os (Fig. 1). The external uterine os closes in the 3rd week. after childbirth. Involution of the uterus in the postpartum period occurs quite quickly. Immediately after birth, the weight of the uterus is on average 1000 g, the length of its cavity is 15-20 cm, the transverse size of the body of the uterus is 12-13 cm. Over one day, the level of the fundus of the uterus decreases by one transverse finger (2 cm), reaching the 5th the day of the middle distance between the navel and pubis; on the 9-10th day. the fundus of the uterus descends behind the pubis. The weight of the uterus by the end of the first week is 500 g, by the end of the 2nd week - 350 g and by the end of the postpartum period - 50-60 g, its length from the fundus to the external uterine os decreases to 8-9 cm, the width of the uterus in the area its bottom is up to 5-5.5 cm. The volume of the uterine cavity at the end of the postpartum period is 3-5 cm3.
The rate of uterine involution depends on the characteristics of pregnancy and childbirth. In case of multiple pregnancy, polyhydramnios, large fetus and weakness of labor, the involution of the uterus in the P. p. is somewhat slowed down. Involution of the uterus is negatively affected by previous inflammatory processes of the uterus and its appendages, the presence of fibromatous nodes in it, infantilism, and restriction of the motor activity of the postpartum mother due to the presence of somatic diseases or complications in the uterus.
When the myometrium contracts, the blood and lymphatic vessels are compressed, some of them become obliterated. Newly formed muscle cells during pregnancy undergo fatty degeneration and resorption; the main cells are significantly reduced in size.
The inner surface of the uterus after childbirth is an extensive wound surface with the most pronounced destructive changes in the area of the placental area (see), where there are many thrombosed vessels. The entire inner surface of the uterus is covered with fragments of the decidua (see) and blood clots.
Rice. 2. Microspecimens of lochia in the postpartum period: a - lochia at the end of the first day after birth, a predominance of erythrocytes is noted; b — lochia on the third day after birth, an increase in the number of leukocytes; 1 - epithelial cell, 2 - decidual cell, 3 - leukocytes, 4 - erythrocytes, 5 - bacteria.
During the physiological course of the postpartum period, the uterine cavity remains sterile during the first 3-4 days. In cleansing the inner surface of the uterus, a large role belongs to phagocytosis (see) and especially extracellular proteolysis. As a result of the breakdown of leukocytes and microbes, enzymes with high proteolytic activity are released. Proteolytic enzymes (see Peptide hydrolases) and antitoxins (see) destroy bacteria, neutralize toxins and promote the melting and rejection of fragments of the decidua and blood clots that are released from the uterus along with many leukocytes. These secretions represent a wound secretion and are called “lochia” (Greek, lochia genera). In the first days of P. p., the lochia are bloody due to a significant admixture of blood; from the 3-4th day, the lochia become serous and bloody and contain many leukocytes (Fig. 2). From the 16th to 20th day, the lochia is liquid and light-colored. By the 6th week. the discharge of lochia from the uterus stops.
Epithelization of the inner surface of the uterus occurs in the process of rejection of the remnants of the decidua (see Postpartum diseases) and ends by the 20th day of P. p., and in the area of the placental area - only by the end of P. p. Retention of lochia in the uterus (lochiometra) for due to its bending in the isthmus area, decreased contractility of the uterus and blockage of the internal uterine pharynx with blood clots and fragments of membranes (see Postpartum diseases) can contribute to the development of endometritis, myometritis (see Metroendometritis). Involution processes occur in the ovaries, fallopian tubes, ligaments of the uterus, vagina and perineum, but they are less pronounced than in the uterus.
The function of the mammary glands after childbirth reaches its highest development. Already during pregnancy, under the influence of estrogens, milk ducts are formed, under the influence of progesterone, proliferation of glandular tissue occurs. With the cessation of the hormonal function of the placenta, the action of the lactogenic hormone of the anterior pituitary gland begins (see Prolactin). This is associated with increased blood flow to the mammary glands (engorgement) on the 3-4th day of P. p., which is a preparatory act for lactation (see). To maintain lactation, breastfeeding is necessary (see Feeding children). It affects the involution of the uterus, since in this case it contracts through a reflex (through the sympathetic nervous system) and hormonal (under the influence of oxytocin) pathway.
Postpartum changes also occur in other organs and systems. The postpartum woman feels tired and needs rest and sleep. Body temperature is normal or slightly elevated in the first days of the postpartum period. Soon after birth, a single rise in temperature (up to 38°) is possible, sometimes with chills, which is explained by increased muscle work during childbirth.
Immediately after birth, significant changes in hemodynamics are observed, which are associated with the redistribution of blood as a result of the cessation of uteroplacental circulation, contraction of the uterus and a decrease in its blood supply, as well as changes in water metabolism and the removal of a significant amount of fluid from the body. There is greater lability of the pulse under the influence of external stimuli. Blood pressure is normal, sometimes slightly reduced. Often in the first days after childbirth, urinary retention is observed, which is associated with a decrease in the tone of the bladder and ureters, and relaxation of the anterior abdominal wall. The intestines are in an atonic state, and there is a tendency to constipation.
Involution of the uterus after childbirth is normal
Postpartum or puerperal is the period from the moment the placenta leaves until the moment when the reverse development (involution) of those organs and systems that have undergone changes in connection with pregnancy begins.
A woman after childbirth is called a postpartum woman. The postpartum period lasts from 6 weeks. The postpartum period is divided into early postpartum period and late postpartum period. Early postpartum period.
- this is the first 2-4 hours. after childbirth, during which the mother is in the maternity ward. Most often, complications associated with the pathology of contractile activity of the uterus after childbirth, as well as anomalies of placenta attachment (remnants of placental lobules in the uterus) are manifested by the occurrence of bleeding in the first hours after childbirth; therefore, for 2-4 hours the postpartum woman is in the maternity ward under constant supervision.
Immediately after birth, the fundus of the uterus is palpated at the level of the navel. Its length along the probe - the distance from the external pharynx to the bottom - is 15-20 cm.
After childbirth, it is necessary to examine the cervix in the speculum and the soft tissues of the birth canal. All postpartum women must undergo an examination. If an injury to the soft tissues of the birth canal, cervix, vaginal walls, or perineum is detected, they must be sutured. During this period, it is necessary to monitor the general condition of the postpartum woman, the color of the skin, mucous membranes, pulse pattern, blood pressure, condition of the uterus, and temperature. From time to time, it is necessary to massage the uterus through the anterior abdominal wall to remove blood clots accumulated in it; paying attention to the consistency of the uterus, its size, pain and the nature of discharge from the genital tract.
Late postpartum period
- this is the time from the moment the mother is transferred to the postpartum department until the changes in the woman’s body caused by pregnancy and childbirth disappear; lasts from 6 to 8 weeks.
Reverse development (involution) of the uterus
During the first week of the postpartum period, the weight of the uterus is halved, i.e., reaches 500 g. By the end of the second week, it weighs 350 tons, by the end of the third - 250 g. By 6-8 weeks after birth, the reverse development of the uterus stops. The uterus of a woman giving birth weighs about 75 g.
The height of the fundus of the uterus immediately after birth is 4 cm below the navel; the next day the fundus of the uterus rises and stands at the level of the navel due to the restoration of muscle tone of the pelvic diaphragm. On the 4th day after birth, the uterine fundus is usually determined at the middle of the distance between the navel and the womb. On days 8-9, the fundus of the uterus can still be palpated at the level of the pubis or 2 cm above it. On average, the fundus of the uterus drops by 2 cm every day.
Epithelization of the inner surface of the uterus.
Epithelization of the inner surface of the uterus is completed by 7-8 days of the postpartum period, with the exception of the placental area, where this process is slower and ends at the end of 6-8 weeks.
Lochia is postpartum discharge (blood, mucus and melted organic matter). Total number of lochia for 6-8 weeks. is estimated at 500-1500g. In the first 2-3 days, lochia has a bloody character, consists of red blood cells, and is called lochia rubra. On days 4-5, lochia takes on a bloody-serous appearance (lochia serosa) with a predominance of leukocytes. A week after birth, mucus, squamous epithelial and decidual cells appear in the uterine discharge, and red blood cells almost disappear. In this form, lochia has a grayish-white color and is called lochia alba. By the end of 3 weeks, the discharge almost stops.
Function of the mammary glands.
— The mammary glands begin to actively develop during pregnancy. In the postpartum period, an increase in their function is observed - endocrine, which promotes the reverse development of the uterus, and secretory, which promotes the formation and secretion of milk. And for the first 2-3 days, the mammary glands secrete colostrum, and from 3-4 days - milk.
Postpartum Clinic
The physiological postpartum period is characterized by the woman’s good general condition, normal temperature and heart rate, correct involution of the uterus, the presence of normal quantity and quality of lochia, normal function of the mammary glands (sufficient lactation), ensuring six feedings.
In the postpartum period, two “physiological” increases in temperature are observed. The first occurs up to 12 hours after birth. It is explained by overstrain of the autonomic nervous system during childbirth and some disruption of the mechanisms of thermoregulation of the mother's body, as well as the entry into the blood after increased muscular work of lactic acid; the increase in temperature on the 3-4th day after birth is explained by the fact that it is by this time that microorganisms penetrate from the vagina into the uterus, in which the processes of regeneration of the mucous membrane are far from completed. In the postpartum period, there may be urinary retention (bladder atony), stool retention, slow reverse development (induction) of the uterus, and engorgement of the mammary glands. Retention of urination and lack of bowel action depend on overexcitation of the sympathetic innervation of the intestine, bladder sphincter, which results in intestinal hypotension and spastic state of the sphincters.
If urination is delayed, you should try to induce it reflexively by placing a heating pad on the suprapubic area. If there is no effect, give oxytocin 1 ml 2 times a day intramuscularly, a single intravenous (drop) injection of ml 25°/’
magnesium sulfate solution. If these measures fail, the bladder is emptied using a catheter.
In the absence of independent stool, on the 3rd day after birth, a cleansing enema is prescribed or a laxative is given orally - magnesium sulfate. Acupuncture is effective.
Slow involution (subinvolution) of the uterus.
- This is a lag in the reverse development of the uterus. Prescribe ice to the lower abdomen, ergot extract inside,
When there is engorgement of the mammary glands, an elevated position is necessary. It is necessary to limit drinking and prescribe a laxative internally. After each feeding, express the remaining milk if the mammary glands are not emptying enough.
Caring for a postpartum mother.
Keeping the external genitalia clean. Lochia causes skin irritation, and this contributes to the penetration of infection into the vagina, uterus and appendages. To avoid this, it is necessary to toilet the postpartum mother at least 3-4 times a day in the first 4 days, and in subsequent days at least 2 times (morning and evening). To do this, wipe the external genitalia, perineum and inner thighs with a disinfectant solution. After using the toilet, the skin is thoroughly dried with sterile material. The linen sheet is changed after each toilet. To wash the external genitalia, various disinfectant solutions are used: potassium permanganate (1: 4000); furatsilin (1:5000); 1% chloramine solution. If there are seams, they must be kept dry and lubricated with alcohol and a 5% alcohol solution of iodine. Normally, sutures are removed 6-7 days after birth.
-•Hygiene rules when feeding a newborn.
1. When the newborn is in the arms of the mother, her hair should be hidden under a headscarf, and her mouth and nose should be covered with a gauze mask.
2. Before each feeding, the postpartum mother should wash her hands with soap and wipe them with a gauze napkin. moistened with an antiseptic solution.
Causes of the pathological condition
Subinvolution of the uterus after childbirth may be due to the following reasons:
p, blockquote 8,0,0,0,0 –>
- C-section;
- multiple pregnancy, accompanied by excessive stretching of muscle fibers;
- retention of parts of the placenta in the uterine cavity after childbirth, these fragments can also become a site of infection and the formation of postpartum endometritis;
- prolonged or rapid labor, depleting myometrial contractility;
- secondary infection – endometritis.
More often than others, the disorder occurs in postpartum women with fibroids, women under 18 or over 40 years of age, in the absence of lactation, especially in the first days after childbirth. Diseases also contribute to the weakening of the body and, as a result, to the slowdown in recovery, such as posthemorrhagic anemia, connective tissue diseases, abnormal development of the uterus, digestive dysfunction with malabsorption syndrome, exhaustion, severe chronic diseases, including tuberculosis.
p, blockquote 9,0,0,0,0 –>
Subinvolution of the uterus after cesarean section is not a pathological, but a physiological process. It is associated with delayed contraction and healing of the cut muscles of the uterine wall. In this case, it is not recommended to use Oxytocin, so antibiotics are mandatory to prevent infectious complications.
p, blockquote 10,0,0,0,0 –>
False subinvolution sometimes occurs if the organ is measured when the bladder is not completely emptied. Therefore, in the postpartum period, you should urinate before a medical examination.
p, blockquote 11,0,0,0,0 –>
Currently, the main theory for the development of uterine subinvolution is considered to be infectious. Normally, it should shrink on its own even in the presence of unfavorable factors. Subinvolution is considered as a risk factor or the first manifestation of endometritis.
Changes in the genitals in the postpartum period
Significant changes in the postpartum period occur in the woman’s reproductive system, especially in the uterus.
Involution of the uterus
In the first hours after the period, a significant tonic contraction of the uterus occurs. Against the background of increased tone, peripheral muscle contractions (contractions) occur, which contribute to a reduction in the size of the uterus. In this case, the walls of the uterus thicken, it takes on a spherical shape, slightly flattened in the front-to-back direction.
The fundus of the uterus at the beginning of the postpartum period is 13-15 cm above the pubic symphysis, the length of its cavity (from the external os of the cervical canal to the fundus) reaches 15-20 cm, the thickness of the walls in the fundus is 4-5 cm. The transverse size of the uterus immediately after birth is 12-13 cm, weight - 1000 g. The anterior and posterior walls of the uterus are adjacent to each other.
The uterus contracts in the direction from the fundus to the cervix. The contractility of the lower section and cervix is much lower, so in the lower section the uterine wall is thinner. The vaginal part of the cervix hangs down into the vagina, its edges are thinned, often have lateral tears and superficial damage (tears). Due to the contraction of the body of the uterus and the circular layer of the myometrium, located around the internal os, the boundary between the upper and lower parts of the uterus is marked. In the first days of the postpartum period, the fundus of the uterus comes into contact with the abdominal wall, and an angle open forward (antlexio uteri) is formed between the body and the cervix. This is facilitated by the relaxation of the ligamentous apparatus and the fact that the woman in labor lies on her back. In the first days after birth, the mobility of the uterus is increased, which is also explained by the stretching and insufficient tone of its ligamentous apparatus. The uterus easily moves upward, especially when the bladder is replaced.
A reduction in the size and weight of the uterus is facilitated by the contraction of its muscles and the morphological changes that occur during this process. Muscles that contract compress the walls of blood and lymph vessels. The lumen of the vessels narrows, many of them close and undergo obliteration. As a result, there is a sharp restriction of nutrition of myometrial cells, their fatty degeneration, decay and resorption.
The state of uterine contraction is judged by the level of its fundus. During the first 10-12 days after birth, the uterine fundus drops daily by approximately 1-1.5 cm. On the first day after birth, the uterine fundus is at the level of the navel (due to increased tone of the pelvic floor muscles), which is higher than immediately after childbirth On each subsequent day, the level of the uterine fundus decreases by one transverse finger. On the second day, the uterine fundus is located above the pubic symphysis by 12-15 cm, on the fourth day by 9-11 cm, on the sixth day by 8-10 cm, on the eighth day by 7-8 cm, on the tenth day by 5-6 cm and on the twelfth-fourteenth day is in the womb. By the end of the 6-8th week after birth, the uterus is the same size as that of a non-pregnant woman (in nursing mothers it may even be smaller). The weight of the uterus by the end of the first week decreases by more than half (by 500-600g), the second week to 350g, the third week to 200g, and at the end of the postpartum period 60-70g.
Involution of the uterus depends on the general condition of the woman’s body, age, number of previous births, and the characteristics of pregnancy and childbirth. In multiple pregnancies, polyhydramnios, large fetuses and labor anomalies, the involution of the uterus is delayed (uterine subinvolution).
In a unique way, healing occurs on the inner surface of the uterus, which, after separation of the placenta and membranes, represents an extensive wound surface, especially in the area of the placental area, since during childbirth the superficial part of the collapsible layer of the mucous membrane is separated. On exposures of the uterine wall, only the basal layer of endometrial epithelial tissue and the remains of the deep glandular layer of the uterine membrane can be found. A large number of small cells that appear among the remains of decidual tissue form a layer of granulation tissue - the granulation shaft. The latter is quickly covered with an epithelial layer, which is formed from the remains of glands. Epithelial proliferation leads to regeneration of the wound surface and its transformation into a typical mucous membrane. The wound surface in the placental area is completely covered with a thin layer of mucosal cells on the tenth day of the postpartum period. The restoration of a full-fledged endometrium is completed only eight weeks after birth.
Lochia
During the healing process of the inner surface of the uterus, postpartum discharge appears. Fragments of decidual tissue, scraps of membranes, blood clots undergo phagocytosis and active proteolysis with the formation of wound secretion - lochia. The nature of lochia changes in accordance with the processes of cleaning and healing of the inner surface of the uterus. In the first 2-3 days after birth, lochia is bloody in nature (lochia rubra), starting from the 3rd day they become bloody-serous with a predominance of leukocytes (lochia rubro-serosa), on days 7-9 after birth - serous (lochia serosa ). The total number of lochia in the first eight days reaches 500-1500g.
Lochia has a neutral or alkaline reaction and a specific musty odor. From ten days after birth, lochia acquires a serous-mucosal character (lochia alba). At 5-6 weeks there is no discharge from the uterus. Sexual activity is permitted no earlier than the eighth week of the postpartum period.
The involution of the cervix lags behind the involution of the uterine body in intensity. Immediately after childbirth, the cervical canal freely allows the hand to pass through. 10-12 hours after birth, the canal becomes cone-shaped, the internal pharynx allows 2-3 fingers through; one day after birth, due to the contraction of the circular muscles surrounding the internal opening of the cervical canal, the internal pharynx allows two fingers through, the cervical canal is funnel-shaped. On the third day, the internal pharynx allows only one finger to pass through. By the tenth day, the cervical canal is formed. The external ocellus closes in the third week of the postpartum period. The cervix takes on a cylindrical shape instead of a conical shape before childbirth, and the external os becomes slit-like in the transverse direction. The ligamentous apparatus, which was in a state of relaxation in the first days after birth, gradually acquires its usual tone and in the third week becomes the same as before pregnancy.
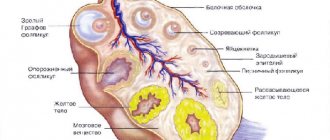
Changes in the ovaries
The ovaries undergo significant changes in the postpartum period. The regression of the corpus luteum ends and the maturation of the follicles begins. In the majority (55-60%) of women who do not breastfeed, menstruation occurs 6-8 weeks after birth. In the majority of breastfeeding mothers (80%), menstruation is delayed for several months or for the entire period of breastfeeding.
The first menstruation after childbirth is often “ANOVULATORY”, i.e. the follicle matures, but ovulation does not occur and the corpus luteum does not form. The follicle undergoes regression, and currently the disintegration and separation of the uterine mucosa begins, in which proliferation processes have arisen (under the influence of estrogen hormones), but secretory transformation of the endometrium does not occur. Over time, the ovulation process, and with it menstrual function, is completely restored.
Diagnostics
p, blockquote 31,0,0,0,0 –>
The risk group includes pregnant women with the following pathologies:
p, blockquote 32,0,0,0,0 –>
- excess of the normal volume of amniotic fluid;
- large or multinodular fibroids;
- large fetus or multiple births;
- history of chronic endometritis, salpingitis, cervicitis, pyelonephritis;
- severe gestosis in the second half of pregnancy, accompanied by increased blood pressure, edema, and the appearance of protein in the urine.
Such patients, in the absence of indications for surgery, can give birth on their own, but after completing the 3rd stage of labor, they require increased attention from doctors. This makes it possible to timely notice a too slow decrease in uterine size and associated infectious complications, as well as begin their early treatment.
p, blockquote 33,0,0,0,0 –>
The following methods are used to diagnose uterine subinvolution:
p, blockquote 34,0,0,0,0 –>
- Collection of complaints, physical examination, determination of the amount and nature of discharge.
- Gynecological examination: a two-handed examination reveals an enlarged uterus that does not correspond to its normal involution, a pear-shaped or spherical shape of the organ.
- Normally, after childbirth, the uterus should be moderately dense. Its softening may be a sign of retention of parts of the placenta in the cavity, which is a source of infection.
- External examination of the cervix using mirrors reveals its swelling, intense hyperemia (redness), the external pharynx is not closed, and blood clots are detected in the cervical canal.
- Ultrasound (through the abdominal wall or through the vagina) allows you to determine the true size of the organ, the thickness of the walls, and identify the remains of the placenta in the cavity.
- MRI of the pelvic organs is an even more informative, non-invasive, safe method.
- Hysteroscopy is one of the most informative diagnostic methods, which at an early stage makes it possible to determine signs of endometritis and retained parts of the placenta.
- There may be no changes in the general blood test, but with the development of inflammation, nonspecific signs appear - an increase in ESR and the number of leukocytes.
- With the development of endometritis, the material of secretions and lochia is inoculated on a nutrient medium. This makes it possible to accurately determine the causative agent of the disease and the most suitable antibiotic to eliminate it.
p, blockquote 35,0,0,0,0 –>
Postpartum involution
In the female body, reverse changes are considered normal and natural, predetermined by nature. All phases of this process follow their own schedule.
With the birth of a child, a woman's reproductive system is rebuilt again. Pregnancy hormones are not produced, and the reproductive tract gradually begins to restore to its prenatal state. It is believed that this period normally passes within three months.
Uterus
It takes about two months for the uterus to fully recover to its previous size.
In the first days after birth, the walls of the organ are thickened; due to peripheral contractions, it has decreased in size, but still has a spherical, flattened shape, and it can be determined by palpation, approximately 12–14 cm above the pubic symphysis. After all, its weight is still about 1 kg with an approximate volume 500 ml. The non-pregnant uterus weighs only 70 g and holds 5 ml. Its return to prenatal size is facilitated by the lysis (dissolution) of proteins, and the number of muscle cells remains the same, and they simply decrease in size. The blood walls and lymphatic vessels shrink, and some of them completely obliterate (close). Additional nerve, muscle and connective tissue cells undergo protein and fatty degeneration and disintegrate. How does the involution of the uterus affect the weight of the organ:
- End of the first week: minus 550–600.
- Second week: minus 300 g.
- Third week: minus 150–200.
By the seventh to tenth day, minor lesions on the cervix, vagina, and perineum are epithelialized. By the end of the second week, the organ is already located only in the small pelvis, and by the sixth week it returns to its normal size, acquiring a cylindrical shape. The isthmus of the cervix is already closed.
Lochia
Postpartum discharge indicates that the healing of the inner walls of the uterus is proceeding normally. Lochia (wound secretion) consists of remaining particles of membranes; blood clots have a neutral or slightly alkaline reaction with a specific predominant odor. If in the first 2–3 days they are profusely bloody, then over time they become bloody-serous in nature due to the large number of leukocytes in their composition. By the end of the first week they become more serous and transparent-watery, and by the sixth week they stop completely. The involution of the uterus is completed. From the eighth week, a woman is already allowed to have sex.
Pathogenesis
p, blockquote 14,0,0,0,0 –>
In the development of postpartum uterine subinvolution and the addition of endometritis, three pathogenesis factors are of primary importance:
p, blockquote 15,0,0,0,0 –>
- Insufficient hormonal and nervous stimulation of uterine muscle fibers
Leads to their overstretching and disruption of contractility (ability to contract). An increase in intercellular spaces between stretched muscle fibers increases the area and depth of penetration of pathogens, which contributes to the development of infection.
p, blockquote 16,0,0,0,0 –>
- Insufficient spasm of the uterine vessels in the first days after childbirth
Causes tissue swelling, inflammation and lack of normal organ contraction. The reason for this is foreign bodies in the uterine cavity (endometrial remnants). For example, this is how subinvolution of the uterus develops after an abortion. Therefore, it is recommended that this procedure be performed by a qualified doctor with careful ultrasound control after it.
p, blockquote 17,0,0,0,0 –>
- Tissue swelling
Promotes disruption of blood supply, which slows down the physiological breakdown of connective tissue fibers located between muscle cells and preventing them from returning to their normal size.
p, blockquote 18,0,0,0,0 –>
p, blockquote 19,0,0,0,0 –>
The division of uterine subinvolution into types is based on infection of the endometrium that occurs after childbirth. Therefore, primary and secondary types are distinguished.
p, blockquote 20,0,0,0,0 –>
The primary type develops in the complete absence of inflammatory changes. It is observed quite rarely and occurs under the influence of such factors:
p, blockquote 21,0,0,0,0 –>
- myogenic, that is, muscle weakness after multiple pregnancy, polyhydramnios, rapid or prolonged labor;
- microcirculatory, that is, disruption of the blood supply to tissues, release of fluid into the intercellular space and swelling during gestosis;
- endocrine, associated with a violation of hormonal stimulation of myometrial contraction; in particular, during subinvolution, one's own oxytocin may not be produced due to lack of breastfeeding.
Endometritis can be caused by viruses and bacteria, including those that normally exist on the surface of the genital organs and in the intestines (opportunistic). The likelihood of this is especially high with retained placenta or urinary tract infection. In such patients, subinvolution of the myometrium after childbirth should raise suspicion of the development of postpartum endometritis.
p, blockquote 22,0,0,0,0 –>
p, blockquote 23,0,0,0,0 –>
Subinvolution
Under the influence of a number of unfavorable factors, reverse changes do not occur or are delayed. The opposite process, in which the uterus is not able to contract to its natural size, subinvolution, is diagnosed by the end of the first week after delivery. There are two types of this pathology:
- Subinvolution of an infectious nature. The reason is inflammatory processes against the background of chronic diseases (pyelonephritis, anemia) or as a result of an infection that has developed due to particles of the placenta or fetal membrane remaining in the uterine cavity.
- True subinvolution occurs from excessive mechanical overstretching of the walls of the organ.
It can be caused by a number of unfavorable factors:
- Difficult pregnancy.
- Multiple births.
- Polyhydramnios.
- Large fruit.
- Anomalies of labor.
- Caesarean section.
- Suppressed immune system.
Bacterial or viral infections and mechanical damage to the internal genital organs can slow down the reverse conversion process. The rate of uterine involution after childbirth can also be affected by age (over 30 years), general condition of the body, and concomitant chronic diseases. The main warning signs of subinvolution:
- Copious brown discharge mixed with blood, unpleasant odor
- Temperature increase.
- Rapid heartbeat, weakness.
- There is no cramping pain in the lower abdomen during feeding.
If a woman is discharged from the maternity hospital, she should consult a doctor as soon as possible with such symptoms.
After examination and ultrasound examination, the specialist determines the type of pathology and prescribes therapy:
- When the cause is an inflammatory process, antibiotics and drugs that improve uterine circulation are indicated. If necessary, vacuum aspiration of blood clots from the organ cavity is performed.
- With true subinvolution, special drugs are prescribed that stimulate the muscle tone of the uterus.
Usually the course of treatment lasts from 10 to 14 days. If a woman seeks medical help in time, the prognosis for recovery is favorable.
In most cases, the woman provokes subinvolution herself. To avoid it after childbirth and caesarean section, you need to walk as much as possible, roll over on your stomach and pay attention to breastfeeding. With good and established lactation, the chance of subinvolution occurring is negligible.
Clinical manifestations
p, blockquote 24,0,0,0,0 –>
The main signs of uterine subinvolution:
p, blockquote 25,0,0,0,0 –>
- slow reduction in organ size after childbirth;
- lochia that persists for more than 3 weeks;
- unpleasant smell of discharge (a sign of infection);
- absence of spasmodic sensations in the lower abdomen when breastfeeding or nipple stimulation;
- nagging pain in the lower abdomen without connection with external causes.
Long-term retention of postpartum discharge in the uterine cavity, or lochiometer, often causes the development of severe endometritis. This acute inflammatory process has characteristic symptoms:
p, blockquote 26,1,0,0,0 –>
- severe fever with chills, sweating, weakness;
- the discharge of lochia is not brown, but yellowish-greenish, purulent in nature, with an unpleasant odor;
- deterioration in general health;
- weakness, headache;
- abdominal pain.
p, blockquote 27,0,0,0,0 –>
Climacteric involution
Against the background of age-related hormone deficiency, the uterus, as the most vulnerable and sensitive organ, is the first to change. During premenopause, it first increases in size, but loses its density. The myometrium begins to degenerate, being replaced by connective tissue. So gradually the uterus loses its contractility. Atrophic processes in the myometrium reduce the organ in volume by approximately half. The cervix becomes short, the lumen of the cervical canal tightens or completely closes.
With the decline of the myometrium, the function of the mucous glands decreases and the amount of vaginal mucus begins to decrease. A jump in such changes is observed in women in the first two years of postmenopause. By this time, the involution of the uterus stops, and 12–15 years after menopause, the organ decreases to the size of the tonsil. The female genital area atrophies and completely fades away.
Principles of therapy
p, blockquote 36,0,0,0,0 –>
The complex of therapy includes medications, instrumental methods, as well as routine measures and gynecological massage.
p, blockquote 37,0,0,0,0 –>
Bed rest, exclusion of physical activity, and regular latching of the newborn to the breast are required. If for some reason (for example, treatment with many antibiotics) the baby cannot be breastfed, the mammary glands, areolas and nipples must be regularly massaged, and the milk must be expressed. There is a pronounced reflex connection between breast stimulation and myometrial contraction.
p, blockquote 38,0,0,0,0 –>
A woman should eat well. Impaired supply of nutrients, for example due to malabsorption syndrome or as a result of starvation, slows down the normal involution process.
p, blockquote 39,0,0,1,0 –>
Hormonal drugs
p, blockquote 40,0,0,0,0 –>
In case of subinvolution of the uterus of various origins (after miscarriage, abortion or childbirth), medications are prescribed that replace physiological female hormones. Oxytocin is usually used for this purpose. This is a hormone synthesized in the posterior lobe of the pituitary gland. It stimulates uterine contractility and increases the tone of the smooth muscles of the myometrium, leading to accelerated involution of the organ. The drug is administered intramuscularly or intravenously. It is contraindicated after cesarean section and with a scar on the uterine wall. In case of increased contraction, accompanied by cramping pain, drugs that relax smooth muscles, for example, No-shpa, are used as an “antidote”.
Classification
Early postpartum period. Its duration is 2–4 hours after the completion of the delivery process. Medical personnel are actively monitoring the woman during this time. The midwife monitors discharge from the genital slit, uterine contractions, measures blood pressure and assesses the general condition of the woman.
If during childbirth there was damage to tissue cells - ruptures, cracks, or the perineum was dissected with a scalpel, then suturing is performed under local anesthesia.
Subsequently, the sutures are regularly treated with a solution of brilliant green and removed on the fifth day. The woman is prohibited from sitting down for another 14 days and during this time it is recommended to feed the baby while lying down.
Consequences and complications
If uterine subinvolution is treated incorrectly, it always leads to endometritis. Even in the case of true damage, when there is no primary infectious factor, the remaining extensive intrauterine wound surface is quickly populated by pathogenic or even opportunistic microorganisms. In the future, this can provoke the development of the following serious diseases:
p, blockquote 28,0,0,0,0 –>
- sepsis, the penetration of microorganisms into the bloodstream and the formation of purulent foci in various organs;
- peritonitis, spread of inflammation to the peritoneum with the formation of an “acute abdomen” and the need for immediate surgical intervention;
- septic shock, rapid decrease in blood pressure, discrepancy between the needs of the brain and the capabilities of the cardiovascular system, impaired consciousness, development of failure of vital organs (kidneys, liver, lungs, heart);
- metrothrombophlebitis, inflammation of the walls of the veins that drain blood from the genital organs, with the formation of blood clots in them and the threat of their spread through the venous system and the right side of the heart into the pulmonary vascular system, which causes a deadly condition - pulmonary embolism;
- embolism of the arteries of the genital organs, causing a sharp restriction of the flow of blood and oxygen to the tissues, which is accompanied by ischemia and death;
- prolonged uterine bleeding, difficult to respond to hemostatic drug therapy;
- hematometra - accumulation of blood in the uterine cavity with subsequent infection.
Thus, at first glance, a harmless slow restoration of the normal size of an organ can become the first sign of extremely serious diseases that threaten a woman’s life.
p, blockquote 29,0,0,0,0 –>
p, blockquote 30,0,0,0,0 –>