Uterine prolapse is a downward displacement of the reproductive organ, which without adequate treatment can lead to complete prolapse of the uterus.
It is a mistake to believe that cervical prolapse can only be observed in older women; according to statistics, 30 out of 100 women of reproductive age also experience this pathology.
Of course, the degrees of uterine prolapse are different, and so are the reasons that provoke this pathology.
One of the most common causes of prolapse of the reproductive organ at a young age is considered to be traumatic childbirth.
The essence of pathology
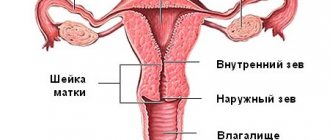
Uterine prolapse develops as a result of weakening of the pelvic muscles, which hold the reproductive organ in its correct and natural position..
The pathological process can affect not only the body of the uterus, but also its cervical region, as well as the fallopian tubes and ovaries.
Pregnancy and childbirth are very stressful for a woman’s body..
If a woman did not prepare for pregnancy - did not exercise, did not take vitamin complexes, and so on, this wonderful and amazing condition - the emergence of a new life - can lead to various pathological changes in the female reproductive system.
All processes that occur in the body of a pregnant woman are associated with hormonal changes, changes in the position of some internal organs, and muscle stretching.
The muscles that support the uterus are most stretched and strained, which can result in weakening or even damage. After childbirth, if the muscles are damaged, the uterus ceases to be supported and, under its weight, moves downward.
TOILET HABITS
This point is closely related to the previous one, since the quality of digestion directly affects how bowel movements occur. Avoid prolonged sitting on the toilet; strive to ensure that the act of bowel movement takes place in one unforced attempt. An important point - DO NOT train the muscles of the perineum and sphincters while going to the toilet, this goes against natural reflexes and “confuses” our body. Analyze pelvic floor training methods, if you use them, and exclude exercises that contain elements of straining.
Causes of prolapse after childbirth
All the reasons that lead to prolapse of the uterus after childbirth are in one way or another related to the woman’s improper behavior during the recovery period.
Doctors must give women recommendations regarding lifestyle and nutrition during the postpartum period.
This is not a whim or empty words, this is a guarantee of a woman’s health and the prevention of dangerous pathologies.
So, what reasons can trigger postpartum prolapse?:
- Muscle injury during childbirth - the use of medical forceps during difficult childbirth.
- Lifting weights - if after childbirth a woman does not take care of herself and regularly lifts weights, this will inevitably lead to prolapse, since the muscles after childbirth have not yet regained their elasticity. Some young mothers who are predisposed to uterine prolapse are prohibited from even holding their own baby in a standing position, and if the doctor has given such a warning, it must be taken with the utmost responsibility
- Poor nutrition. Constipation after childbirth is a sure way to prolapse, which is why it is so important to include in the diet of a young mother foods that improve intestinal motility,
- Hereditary predisposition is the only cause of prolapse, which does not depend in any way on the woman herself or on the midwife who delivered the child. However, if a woman knows about her predisposition and informs the gynecologist about this, the specialist will choose a different pregnancy monitoring program and will use a more gentle birth technique.
Expert opinion
Dmitrieva Elena Yurievna
Gynecologist-endocrinologist, 40 years of experience
Natural childbirth does not always occur without complications. And these complications do not always appear immediately; uterine prolapse is the failure of the uterine muscles to hold the reproductive organ in the correct position. Such a complication may remain unnoticed for some time after childbirth, and then, when the uterus descends significantly, a concomitant clinical picture appears in the woman. Deep vaginal birth tears are very dangerous, so doctors most often use episiotomy to prevent severe stretching of the tissue. Also dangerous is a violation of the integrity of the muscles that raise the anus. Despite the fact that this pathology is not common, it is quite serious; a woman may develop gas and fecal incontinence, as well as fistula formations, all of which requires surgical treatment.
Prevention
Having information that such a pathology can arise as a result of pregnancy and childbirth, it is better to prepare for it in advance. Moreover, it is quite real. If you have this hereditary pathology, then do not forget to tell your doctor about it. The doctor observing the pregnancy will be more attentive, and the obstetrician attending the birth, in case of vaginal ruptures, for example, will use the most gentle suturing method, which will prevent prolapse.
During pregnancy, many people talk about the need for moderate physical activity. This load also applies to the pelvic floor muscles, which are responsible for supporting the uterus.
The same exercises that can be your treatment if you still allow uterine prolapse after childbirth are gymnastics for the prevention of prolapse, both during pregnancy and after childbirth. But after giving birth, before performing these exercises, you should consult your doctor, since not all tension is good after the birth of the baby.
Exercises for the prevention (treatment) of uterine prolapse
Sitting in the office or at home on the couch in front of the TV, standing in line, lying in the bathroom or in bed before bed, you can perform a block of exercises to strengthen the pelvic floor muscles.
The first exercise is to squeeze your vaginal muscles and count to 10, relax. Gradually increase the interval between muscle tension and relaxation. Repeat at least 10 times.
The second exercise is a sharp contraction and relaxation of the muscles without delay in a tense state. This exercise can be completed up to 50 repetitions at a time, starting with about 10 tension-relaxation complexes.
Prolapse of the uterus after childbirth is a serious pathology that will not go away on its own over time, but will only become more serious. Don't be frivolous and visit your doctors regularly just for a routine check-up. Let them tell you at the next examination: “Everything is fine with you. We are waiting for you in a year."
We recommend reading: Another problem that often plagues new mothers is urinary incontinence after childbirth. How it is treated, and what needs to be done to never encounter it.
Author
Editorial staff of the portal Mama66.ru
Share
Symptoms of prolapse
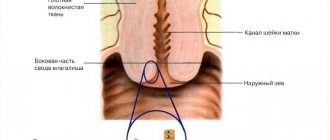
One of the symptoms of postpartum prolapse is a clear definition of a dense tubercle at the entrance to the vagina, which can be easily felt if the woman squats.
This symptom is characterized by a parodic disappearance of the compaction, but after some time it appears again.
In addition, other symptoms may occur:
- pain in the lower abdomen, as well as in the lower back and sacral region;
- problems with urination. Possible incontinence or stagnation of urine, which provokes cystitis, pyelonephritis and other inflammatory processes;
- problems with bowel movements. Most often this is constipation, especially if a woman has a tendency to it;
- in some cases, the cervix can be felt by palpating the genital fissure, however, such a symptom indicates an advanced form of prolapse;
- blood impurities in natural secretions.
NOTE!
If such symptoms are observed in the first two months after birth, it is too early to talk about prolapse.
It takes time to restore muscle tone, even if the muscle injuries during childbirth were minor. But if signs of prolapse persist for 5 months or more after childbirth, pathology can be suspected.
What is the danger of uterine prolapse during pregnancy?
The following symptoms indicate cervical prolapse during pregnancy:
- pain in the lower abdomen and lumbar region;
- shooting pain in the pubic area;
- painful intercourse;
- feeling of fullness in the vagina;
- colorless or bloody discharge;
- disturbance of urine outflow;
- involuntary urination;
- difficulty in bowel movement.
If the uterus is below the required position during pregnancy, this condition can lead to dangerous complications. In the early stages, the risk of spontaneous abortion increases 10 times, so the woman is recommended to go to the gynecological department for preservation.
Attention! Against the background of uterine prolapse, there is a risk of premature birth.
In the third trimester of pregnancy, a woman with uterine prolapse is advised to be hospitalized; such a recommendation from gynecologists is associated with the risk of a rapid onset of labor. You need to understand that prolapse in the first trimester is much more dangerous than in the later stages.
The descent of the uterine fundus immediately before childbirth is a natural process that ensures spontaneous delivery. If this process began after 30 weeks of pregnancy, there is nothing to worry about. In case of premature birth, the child and mother will be able to provide the necessary assistance. Premature children do not differ from those born at term, but in the first year of life they lag behind in development.
Degrees of the disease
1st degree prolapse is a slight prolapse of the external os of the uterus .
At the same time, the pathology does not spread beyond the genital opening. A woman may experience mild pain in the lower abdomen, which is usually attributed to cystitis, painful periods, inflammation, and so on.
2nd degree prolapse
looks like partial loss of the genital organ .
In this case, the prolapsed area can be injured when walking, which is fraught with inflammation and infection. Problems arise during intimate contacts. 3rd degree and 4th degree - partial and complete loss of the reproductive organ from the genital slit .
The degrees of pathology are presented in the photo.
Special physical education
Exercises for prolapsed internal organs often help avoid surgery. Their main task is to strengthen the muscles of the abdominal wall, pelvic floor, lumbar region, normalize the functional state of the digestive organs, increase the motor functions of the intestinal tract, and activate redox processes. It is recommended to perform the following groups of exercises:
- Lying on the couch with the head end raised 10-12 cm, on your back, perform breathing exercises (full breathing, diaphragmatic breathing). The movements are performed rhythmically, full amplitude, at an average pace.
- Exercises for legs - with tension and free.
- Lying on the right side - movements of the limbs. Diaphragmatic breathing. Repeat the same on the left side.
- Lying on your stomach, exercises are performed to strengthen the spinal muscles (movement of the legs and lower torso).
- Knee-elbow, knee-wrist position - exercises for the muscles of the trunk and limbs.
- Lying on your back - exercises for all muscles of the legs and torso. Without increasing pressure on the abdominal cavity, the transition from a supine position to a sitting position is also excluded.
All exercises for prolapse of internal organs are performed for 15 - 20 minutes. At the final stage, gymnastics for the medium and small muscles of the limbs and breathing exercises are recommended.
Starting from 6-8 weeks after achieving a positive result (improved appetite, subjective state, performance, sleep, normalization of stool), exercises for posture are introduced into the therapeutic complex of physical activity, with the exception of bending the body forward. In the course of treatment for prolapse of internal organs, it is advisable to use no more than 3 sets of exercises, selected individually.
When approaching the natural position, classes can be carried out somewhat less frequently than in the first stages. It is recommended to lift objects from the floor after sitting down. When getting out of bed, the patient must first turn on his side, lower his legs and only then raise his torso.
During the first year of treatment, jumping, bending the body forward, and running are not recommended. To activate the motor functions of the digestive tract, massage of the sacral and lumbar region, self-massage of the abdomen, and colon massage are indicated. Gymnastics for prolapse of internal organs should be performed regularly.
Do I need treatment?
Uterine prolapse must be treated, and therapy must begin as early as possible .
If the uterus descends so much that it falls out of the genital slit, quite often it has to be removed.
In addition, the displaced reproductive organ puts pressure on both the bladder and intestines, disrupting their functionality and leading to various complications.
Patient diagnosis
Initially, prolapse is diagnosed when examining the patient in a gynecological chair, after which the woman is prescribed additional studies:
- colposcopy;
- transvaginal or transabdominal ultrasound;
- analysis of a vaginal smear for pathogenic odds;
- cytology;
- general and bacterial urine analysis.
Is it possible to independently detect uterine prolapse? Read here.
Treatment regimen
To choose the optimal treatment regimen, the doctor must consider the following factors::
- patient's age;
- degree of prolapse;
- presence of background pathologies;
- the ability to preserve reproductive function;
- possibility of complications after surgery.
Conservative methods are effective only in the early stages of the disease, however, in most cases, the pathology involves surgical intervention.
Conservative methods
Drug therapy is based on the use of the following drugs:
- anti-inflammatory drugs - Voltaren, Flamax, Terizhinan, Diclofenac;
- non-steroidal drugs - Nurofen, Celecosib, Meloxicam, Piroxicam;
- antimicrobial agents - Pennicillin, Biomycin, Streptomycin;
- hormonal drugs - drugs in the form of tablets, suppositories and ointments that contain estrogen; Ovestin vaginal suppositories are most often prescribed.
Drug therapy gives a positive effect only in the initial stages of prolapse.
In some cases, a woman is offered to wear a special uterine ring - a pessary, which will hold the reproductive organ in the correct position.
Sometimes a pessary is needed temporarily while conservative treatment of the pathology is carried out, in other cases wearing the device becomes lifelong - provided that the woman recovers from surgical intervention.
As for traditional methods of treating prolapse, they can be effective in combination with drug therapy and gymnastic exercises.
The most commonly used medicinal plants are::
- plantain;
- Dill seeds;
- Melissa;
- pine nuts;
- dope;
- smoker;
- quince;
- astragalus.
Some of these plants are indicated for oral administration; decoctions of others can be douched or taken in sitz baths.
Surgical intervention
Surgery for prolapse is advisable in advanced stages of the disease, when conservative methods are powerless.
Postpartum prolapse is eliminated in one of the following ways :
- vaginoplasty;
- shortening of the ligaments that support the uterus;
- attachment of the uterus to the pelvic floor ligaments;
- plastic surgery of the ligamentous apparatus;
- suturing of the vaginal lumen;
- complete removal of the uterus - practiced in women who have passed reproductive age.
In some cases, when the prolapse is complicated, it is possible to use combined surgical techniques - several types of pathology elimination are used at once.
Kegel exercises
Most often, women diagnosed with prolapse are prescribed Kegel exercises, the purpose of which is to strengthen the muscle fibers of the pelvic floor and normalize the tone of the reproductive organ.
You must understand that each exercise has its own characteristics and recommendations for implementation . Therefore, it is advisable that the doctor clearly explain to the woman exactly how she needs to perform the exercises, and which ones will be preferable.
IMPORTANT!
The undoubted advantage of Kegel gymnastics is that the exercises can be performed without interrupting your daily routine; they can be done while washing dishes, standing at a bus stop, while walking or before bed.
Performing Kegel exercises will be difficult at first, but after a woman gets used to this technique, the exercises will not seem difficult.
In addition to Kegel exercises, there are other methods , for example, physical therapy according to Atabekov, according to Yunusov, yoga and others .
POSTURE AND POSTURE CONTROL
In yoga classes in many schools, they teach you to carefully and consciously build tadasana - a mountain pose, in which you stand on both legs and align the whole body, trying to optimally coordinate the work of the muscles of the feet, legs, body and shoulder girdle. I recommend doing the same (with reasonable care) in everyday life - when you work, stand at a bus stop, in public transport, in line - anywhere. Level up - try to eliminate excessive pelvic tilt, when the lower back and stomach “fall” forward, engage your feet and thigh muscles, straighten your shoulders and breathe freely. This is not as simple as it seems at first glance, and requires skill. But this skill is incredibly useful and necessary in life, so take the time and master it.