Retention cysts of the cervix (Nabothian cysts, ovuli Nabothi) are benign cavity formations containing mucus. They are formed as a result of blockage of the ducts of the cervical glands and the accumulation of their mucous secretion. They are asymptomatic, in most cases do not require treatment, and do not become malignant. They are detected on the vaginal part of the cervix by a gynecologist during a visual examination, in the cervical canal - during an ultrasound examination with a vaginal sensor.
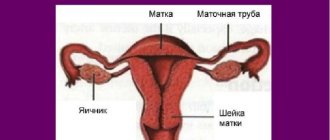
Retention cysts usually form in the transition zone of the cervix
Classification
Cysts on the cervix occur as formations of two types:
- A retention (or Nabothian) cyst of the cervix occurs inside the cervical canal in the process of clogging the gland duct with mucous secretion and epithelial cells. The accumulation of excess mucus leads to the development of a bulging cystic nodule. Such a formation can be single, but often multiple brushes form on the cervix.
- An endometrioid cyst of the uterus is a cavity node filled with bloody secretion. The lesion can be single or in the form of several separate growths.
The formation develops due to the ingrowth of endometrial cells (the inner layer of the organ) into the tissue of its cervical part.
Normally, over the course of the monthly cycle, the endometrium thickens in preparation for implantation of the egg. If fertilization does not occur, the endometrial cells are rejected and excreted in the menstrual blood. During the pathological process, endometrial cells migrate and attach to other organs and tissues, including the cervical canal. During the menstrual cycle, the endometrioid node begins to bleed, blood fills small cavities, and a cyst appears on the cervix, which is detected along with endometrioid cysts on the ovary and other organs.
Formations on the cervix also differ in place of development:
- an endocervical cyst occurs inside the cervix (in the canal where the glands secrete mucous contents);
- a cyst on the uterus, localized on the outer part of the cervix, extending to the vaginal vault, is called paracervical.
What does a mass on the cervix look like?
Visually, upon examination, a single uterine cyst looks like an elongated or rounded tubercle; multiple nodes look like brushes on the cervix or inside the cervical canal.
Large single cysts and extensive growths of small nodes cause noticeable discomfort and complications. Their growth in women is referred to as a pathological condition - uterine cystosis.
The nodes that appear on the ducts of the nabothian glands have a whitish-yellow color, endometrioid formations acquire a reddish-bluish or chocolate color.
Preventive measures
The main preventive measures for the prevention of non-bothian cervical cysts can be called:
- systematic visits to the gynecologist for control diagnostics;
- timely detection and treatment of infectious and inflammatory diseases that can cause cyst formation;
- To prevent relapses of the disease, physiotherapeutic procedures and the use of homeopathic and hormonal medications are prescribed.
It is important to note that it is better to prevent any disease than to quickly deal with its negative consequences.
Despite the fact that in most cases the non-Botian cyst has a benign development, its treatment should not be neglected. Any medical forum says that many diseases are curable, but only if they are diagnosed in a timely manner.
Video: Removal of nabothian cysts of the cervix
Cervical Nabothian cysts. Removal of nabothian cysts
Causes of uterine cyst formation
The reasons for the appearance of neoplasms in the uterus have not been fully established. It is believed that a combination of provoking factors forms the conditions under which such growths develop.
In gynecology, the basic causes of cysts on the cervix of any type are identified:
- Cervical erosions.
- Tissue damage during childbirth.
- Unprofessional termination of pregnancy (abortions often result in severe cervical injuries)
- Therapeutic procedures, including excision of polyps of the internal canal of the cervix, coagulation (cauterization) of erosions using laser, radio waves, chemicals, diagnostic curettage.
Erosion that occurs during these processes injures not only the mouths of the excretory ducts of the glands. Endometriotic cysts of the cervix are also associated with tissue damage when endometrial particles penetrate and implant into the damaged surface.
The reliability of the above reasons is confirmed by the fact that cervical cysts more often occur in patients of childbearing age who have experienced childbirth or abortion.
The mechanism of formation of a retention cyst in the uterine cavity is directly related to the fact that the outlet ducts of the nabothian glands located inside the cervical canal become clogged with mucus and exfoliated cells. When the lumen of the gland is blocked, the outflow of secretion is suspended, it accumulates in the outlet channel, transforming into a nodule.
The immediate causes of a cyst on the cervix due to blockage of the excretory glandular ducts are considered to be:
- Age-related changes in which the cells of the squamous epithelium of the vagina shift inside the cervical canal, blocking the outflow of mucus from the outlets;
- Inflammation of the cervical canal (endocervicitis), leading to swelling of the walls of the glandular ducts and narrowing of their lumen. Cervicitis is caused by pathogens such as trichomoniasis, mycoplasmosis, gonorrhea, ureaplasmosis, herpes virus and papilloma.
- Hormonal imbalance, which can also cause the development of cysts on the uterus, leading to thickening and increased viscosity of the mucus of the endocervical glands.
In addition to them, experts point to several reasons that also contribute to the occurrence of cervical cysts:
- installation of an intrauterine device, hysteroscopy (examination of the uterine cavity using a hysteroscope);
- inflammatory processes in the appendages and diseases of the uterus;
- disorders of the metabolism of fatty compounds.
Symptoms
The severity of symptoms during the development of a cyst in the uterus largely determines the method of treating this pathology.
Single and small cystic formations of the uterus usually do not cause symptoms and are detected during examination by a gynecologist.
The first symptoms of a cyst on the cervix begin to appear:
- if the node has become large (more than 10 mm) to cause discomfort;
- with multiple growths of brushes on the cervix;
- against the background of infection and suppuration of the formation.
The basic signs of a cystic tumor in the uterus are not the same, which is due to:
- node size;
- localization - in the vaginal area of the uterus or inside the cervical canal;
- coverage area - in the form of a single formation or multiple brushes on the cervix and inside the cervical canal;
- type of formation - Nabothian cysts or endometrioid lesions;
- presence of infection.
The main manifestations during the development of nabothian nodes:
- Dyspareunia is discomfort and pain during intimacy, which is associated with erosion, a decrease in the volume of mucus produced by the endocervical glands and increased dryness of the mucosa.
- Increased secretion of mucus, which occurs with significant ectopia - the growth of endocervical epithelial cells from the cervical canal onto the flat epithelium lining the outside of the cervix.
- The appearance of yellowish, purulent discharge with a specific odor, which indicates the development of infection in the area of the cystic node.
- Painful periods. This phenomenon occurs when there is a significant growth of small nodes inside the cervical canal, which decreases, preventing the normal outflow of menstrual blood from the uterus. Bloody clots accumulate and stretch the lower segment of the uterus, causing pain.
Why are uterine cysts dangerous?
Is it dangerous when a cyst forms in the uterus? And is it necessary to have surgery to remove such a formation?
As long as the nodes are painless and small, they do not affect the woman’s condition. But there are conditions under which such a pseudotumor can cause negative consequences.
In what cases can it be dangerous?
If the node and surrounding tissues become infected with microbes and viruses, inflammation begins. If this process is often repeated, chronic diseases of the reproductive organs occur: cervicitis in the cervix, colpitis in the vagina, salpingitis, adnexitis, oophoritis in the fallopian tubes and ovaries. In addition to the fact that these diseases themselves are dangerous for the female body, many of them can cause inability to conceive.
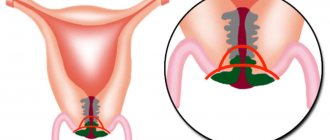
Often small nodules cover a significant part of the cervical canal or grow over the entire internal surface. If the entire internal lumen of the cervix becomes overgrown with such nodes, it will close, which can complicate conception and gestation. Large nodes also narrow the internal canal, being a mechanical factor in menstrual dysfunction, menstrual pain and infertility. This is why it is necessary to treat cervical cysts.
Can a uterine cyst burst?
Such cases in gynecology are recorded very rarely. But rupture can occur if a large node (more than 20 mm) with a thin wall is damaged during rough intimate contact. Sometimes this happens during childbirth if the tumor is located in the area of a cervical rupture or an artificial incision made surgically to facilitate the baby's exit from the uterus.
Possible pathologies
If recommendations for the treatment of cystic tumors are not followed, there is a risk of secondary formation.
Possible pathologies:
- Deformation of the pelvic organs. Cervix, kidneys, intestines.
- Since the bulge is a capsule with liquid contents, the growth of the tumor and an increase in the amount of liquid causes suppuration. The liquid may contain microbes and bacteria that cause a number of pathologies. Inflammatory processes are possible. An increase in body temperature and pain in the lower abdomen indicate this.
- When a capsule containing liquid ruptures, an inflammatory process is also possible.
Women are advised to carefully monitor their own health. Visit gynecologists regularly. Take smears to check the condition of the vaginal microflora and other laboratory tests.
Diagnosis
When diagnosing a cyst of the uterus and cervix, it is important to differentiate (distinguish) it from other pathological formations, including malignant ones, and also to identify the factors that provoked its appearance.
The following diagnostic research methods are used:
- Examination of the cervix using gynecological speculum. The method allows you to see retention and convex yellowish nodes or endometriotic dark red lesions that bleed upon contact with a medical instrument.
- Cytological examination to exclude oncology. This is a microscopic examination of cells scraped (smear) from the cervix and its internal canal, in which any damage and changes in the structure are visible. The accuracy of detecting malignant changes is 80%.
Colposcopy. A procedure for examining the outer mucous membrane of the cervix and vagina, in which tissue is examined in detail using a colposcope with an optical head. The LED illumination of the device allows you to examine hard-to-see areas. The device repeatedly (up to 40 times) magnifies the image of the affected area, down to the cellular level.
- To detect pathological changes during colposcopy, the cervix is lubricated with a weak solution of iodine or vinegar, which can cause a slight burning sensation. Normal tissue is stained brown, cells with pathology do not react to solutions. Today, during colposcopy, it is possible to save photo and video data.
- Biopsy and histology.
The most accurate method for distinguishing a benign node from a cancerous one is a targeted biopsy under the control of a colposcope followed by histological analysis.
Biopsy means the process of removing a tiny (no more than 5 mm) piece of mucosa containing abnormal cells for histological examination. The main task is the early detection of the first symptoms of cancerous changes in the cells of the cervix with an accuracy of up to 99%.
Unlike cytology, histological examination examines sections of problem areas. If it is suspected that a neoplasm in the uterus has appeared due to epithelial proliferation, then histology will rule out the cancerous nature of the growth.
Tissue sampling during biopsy is carried out: with a thin needle (targeted method), wire loop (radio wave), excision with a scalpel (wedge-shaped).
If a biopsy of tissue from the cervix is performed, the procedure does not cause pain because there are no nerve endings in this area. Sometimes mild spasmodic pain occurs.
After the procedure you may experience:
- slight nagging pain (1 – 2 days);
- slight bleeding (usually with low blood viscosity) for up to 5 days.
Not recommended for 7 – 10 days:
- intimacy, increased stress, including sports, lifting heavy bags;
- using tampons, douching.
Contraindications to biopsy:
- menstrual bleeding at the time of the procedure;
- abnormally low blood clotting;
- inflammation of the reproductive organs in the acute stage.
- Transvaginal ultrasound (ultrasound examination)
The main procedure that is always prescribed when diagnosing a formation on the cervix, combined with other methods. Helps detect changes in size, tissue structure, blood supply, and development of pathologies.
Since the organ is being examined from the inside, a vaginal sensor is used for the most reliable information, since viewing through the abdominal wall will not give a complete clinical picture in this case. There are no unpleasant sensations.
- Laboratory research:
- A general blood and urine test (number of leukocytes, ESR, protein level, bacteria) will indicate the degree of likelihood of developing inflammation;
- blood test: for the presence of sexually transmitted diseases and other sexually transmitted infections;
- on the level of thyroid hormones, progesterone, estradiol, prolactin, tumor marker proteins, which indicate the likelihood of a malignant process;
After using diagnostic methods, the doctor determines the cause of the formation of cystic nodes on the uterine cervix, the question of the need for their surgical removal or treatment of the causative disease, prescribing anti-inflammatory drugs and hormones is considered.
Diagnostic methods
Ultrasound photo of the endocervix
The initial diagnosis of the disease is made by a doctor during examination using a mirror. In the future, the following methods are used to confirm the correct diagnosis:
- An ultrasound examination will reveal cyst formations, their location and size. Ultrasound can also give a clear definition if there is a controversial diagnosis. For example, uterine fibroids occur with similar cyst-like pathologies, which are very similar in appearance to the enocervix, but the fibroid cyst has a more dense structure.
- Colposcopy is a method of examining the cervix using a colposcope. This method allows you to identify the smallest foci of formations on the mucous membrane.
- PAP smear and oncocytology determine pre-cancerous formations. As described above, an endocervical cyst is benign, but it may be similar in appearance to a malignant formation.
- Tests to determine urogenital infections are carried out to exclude or confirm the presence of sexual diseases.
- Differential examination is required when the uterine lining is heterogeneous. Diagnosis will rule out adenomyosis.
After operation
After surgical removal of nodes on the cervix, the following is considered a natural phenomenon:
- yellowish and brown discharge for 7 – 10 days;
- mild nagging pain in the abdomen (2–4 days).
Most gynecologists recommend for 20 days after cryodestruction, surgitron, laser and for 45 days after the diathermocoagulation procedure to avoid infection and bleeding:
- exclude intimate contacts completely;
- do not lift weights, reduce any physical activity;
- do not use hot communal baths, foot baths, refuse to visit baths, steam rooms, saunas;
- exclude swimming in the pool, river, sea;
- observe hygienic cleanliness, but avoid douching and the introduction of any suppositories until 8–10 days have passed after the procedure.
Treatment after surgery from 8 to 10 days (not earlier) involves the use of anti-inflammatory disinfecting suppositories. Before this, epithelization occurs - the primary healing of the wound at the site of the removed formation.
Only a gynecologist prescribes suppositories, taking into account all the features of the patient’s treatment and illness. Used: Depantol, Hexicon, Kolposeptin, Betadine, Osarbon, Vokadin, Povidone-Iodine, Venro-kit.