What is colposcopy
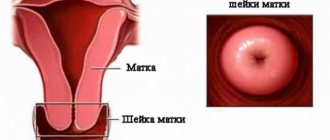
Colposcopy is a research method that allows you to identify cancerous and precancerous changes that appear on the surface of the cervix and vagina. The procedure is performed using a special instrument called a colposcope. This device allows the doctor to examine the cervix and vagina under a magnifying glass.
Extended colposcopy is an in-depth study of the mucous membrane of the cervix. The method allows you to identify changes that are invisible during the usual procedure. To conduct an extended colposcopy, the gynecologist pre-treats the cervix with a weak solution of acetic acid, and then applies iodine. These substances provoke a reaction during which the surface of the mucous membrane changes. Based on the manifestation of changes, one can assume the presence of undesirable processes. It is worth noting that the accuracy of colposcopy does not allow a definitively correct diagnosis to be established, therefore a number of additional manipulations are performed to confirm the data.
Why is colposcopy performed?
Colposcopy is an important diagnostic procedure that allows you to identify dangerous gynecological diseases in the early stages of development. The technique allows you to detect cervical erosion, leukoplakia, dysplasia and even cancer. Colposcopy is used when poor smear cytology or Pap test results are obtained.
The doctor may prescribe such an examination if any pathologies of the cervix are detected. To clarify the diagnosis, a biopsy is performed simultaneously with colposcopy. A biopsy is a procedure that requires the collection of tissue samples.
When is an examination necessary?
Indications for colposcopy include the following conditions:
- Suspicious cells were found in the smear for atypia;
- a woman is bothered by spotting after a gynecological examination or sexual intercourse;
- during the examination, the gynecologist revealed changes in the cervix;
- the woman has cervicitis or polyps;
- genital warts were found.
How to prepare for colposcopy
For the results of colposcopy to be informative, the patient should abstain from sexual intercourse 1-2 days before the procedure. It is also not recommended to use tampons and douching.
Colposcopy can be done on any day of the menstrual cycle except days of bleeding. During menstruation, manipulation is not carried out, because the natural process complicates diagnosis. Particles of blood and rejected mucous membranes do not allow the doctor to examine the changes, so the results will be less informative.
Attention! Many women are interested in the question: is it possible to perform colposcopy during pregnancy? Gynecologists say that, if necessary, the study is possible, it does not affect the process of gestation, and does not increase the risk of premature termination of pregnancy.
How is the examination carried out?
The procedure is performed in the gynecologist's office. The woman is positioned in the gynecological chair in the same way as during the examination. To see the cervix, the gynecologist places a special speculum in the vagina and opens it. Afterwards, the doctor installs the colposcope a few centimeters from the entrance to the vagina. Light comes from the optical device, which illuminates the genitals and allows you to examine the mucous membrane.
After clearing the cervix of mucus, the doctor applies a solution of acetic acid to its surface and then covers it with an iodine solution (pictured). If abnormal staining is detected, a biopsy of individual areas is performed. The whole process takes no more than 25 minutes. During the procedure, the woman does not feel acute pain, but slight discomfort is possible. During application of the reagents, a burning sensation appears, which disappears after a few seconds. After the diagnostic procedure, a woman may experience slight bleeding that goes away within a few days.
Causes
Acetowhite epithelium requires further examination of patients, passing the necessary tests and conducting additional examinations, since this sign may indicate the presence of focal cervicitis (inflammation), and it is also often considered a manifestation of a viral infection of the cervix, dysplasia and other pathologies.
The reaction spreads to the vessels, the structure of which has undergone some disturbances, so they spasm, become white and are called acetowhite epithelium.
Acetowhite epithelium itself is not a disease, but always acts as a harbinger of developing pathologies. Gynecologists are interested in prompt diagnosis after identifying such a sign.
Decoding the results
Only a gynecologist can fully decipher the results of colposcopy. You should not look at them yourself and try to interpret the conclusion. Some terms can frighten a woman, despite the fact that pathological changes do not always indicate dangerous diseases. To identify dangerous diseases, the result of colposcopy is not enough, there is a diagnostic error, so there is no need to worry in vain, it is better to immediately seek advice from a doctor.
Attention! If colposcopy reveals an iodine-negative zone, the woman is advised to undergo additional examinations.
Norms
In the absence of structural anomalies, the length of the cervix in a healthy woman is about 3 cm. The external os and the cervical canal have different shapes. If the patient has given birth, the canal takes on a slit-like appearance and may have scar changes due to ruptures. A nulliparous woman is characterized by a pinpoint external os. Such data must be indicated in the colposcopy transcript.
Flat epithelium
Stratified squamous epithelium (the original squamous epithelium of the cervix) is the surface of the outer part. It can be not only normal, but also changed. The healthy appearance of the tissue is described on examination as pale pink with a smooth surface.
Normal squamous epithelium does not turn white when tested with acetic acid, but acquires a dark brown tint when iodine is applied. If the epithelium of the outer part is changed, during a colposcopic examination the boundaries and nature of the pathology will be noted. Similar data is indicated in the diagnostic transcript. During menopause, the stratified squamous epithelium changes and is described by gynecologists as atrophic. Such deformations appear against the background of a decrease in the production of female sex hormones.
Columnar epithelium
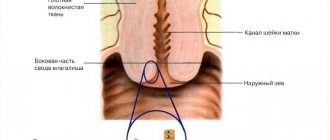
Columnar epithelium lines the inside of the cervical canal. This type of tissue ensures the production of mucus and the formation of a protective plug, which prevents infection from entering the uterine cavity. Normally, columnar epithelium should only be inside the canal. During colposcopy, its location is specified in the transcript.
If an abnormal localization is observed: on the surface of the cervix or in the vagina, then upon examination this area is identified as an area of redness. The glandular tissue is velvety, consists of villi, and a blood vessel is visible in the center of each. During the examination, the doctor identifies a finely lumpy surface when the cylindrical tissue is located on the cervix. When treated with vinegar, a faint white color can be seen; when touched with a tool, the hearth may bleed.
Metaplasia and transition zone
An important marker of colposcopic examination is the determination of the transition zone. This concept refers to the boundaries of two types of epithelium. Gynecologists also call this area the transformation zone, since it is here that the squamous and columnar epithelium meets.
Experts identify several transformation zones:
- When a transformation of the first type is detected, the identified zone is completely located on the cervix. Normally, such a shift is diagnosed in pregnant women and girls.
- In the second type of pathology, the zone is located in the cervical canal and is barely visible during the examination. Normally observed in an adult woman after childbirth.
- In the third type, the transformation zone cannot be detected during colposcopic examination. This change is normal for women during menopause.
Metaplasia is also a type of deformity; this diagnosis is often received by young women or girls, pregnant patients, and women using combined oral contraceptives. Metaplasia is the result of replacement of columnar epithelium with flat epithelium. The doctor must distinguish this condition from pathological changes. In the transcript of colposcopy you can find the following marks:
- the surface of the cervix is even and smooth, small vessels can be traced in the area of the external pharynx;
- pronounced white color when treated with vinegar;
- iodine-negative areas are partially positive.
Confirming the diagnosis of metaplasia is quite difficult and requires a biopsy. The reason for the appearance of such a change is the active production of estrogen hormones by the female body. Normally, an excess of these substances is present in the blood of young girls during puberty, but sometimes an excess indicates the development of endometriosis.
Pathologies
As a result of the influence of external and internal environmental factors, the surface of the cervix may change.
Most often, pathological changes are provoked by the following reasons:
- hormonal disorders;
- sexually transmitted infections;
- human papillomavirus activity;
- serious injuries to the genital organs;
- effect of drugs.
Attention! If you suspect the development of pathology, you should not hesitate to consult a doctor. Early diagnosis is the key to successful treatment.
Iodine-negative areas
After treating the cervix with Lugol's solution (contains iodine), a qualitative reaction of the active substance with starchy compounds occurs. Glycogen contained in epithelial cells reacts upon contact with iodine and produces a dark brown color.
If certain areas of the cervix are not stained with iodine, a note is made in the transcript confirming the presence of iodine-negative lesions. Such changes appear in dysplasia, leukoplakia, metaplasia and ectopia. Also, such a manifestation indicates the development of erythroplakia or epithelial atrophy.
Acetowhite epithelium when treated with vinegar
Treating the cervix with vinegar is not only a preparation step before the Schiller Test, but also a diagnostic operation. An acetic acid solution allows you to evaluate the reaction of blood vessels.
Sharp spasms, accompanied by significant blanching of the surface, manifests itself in the following diseases:
- dysplasia;
- condylomas;
- flat papillomas;
- endocervicitis;
- cervicitis;
- cervical cancer;
- erythroplakia.
Attention! The listed pathologies in the early stages can be treated without surgery; in the later stages of progress, a woman may lose her reproductive ability, so treatment must be provided in a timely manner.
Mosaic or punctuation
Such phenomena are described as coarse or fine punctuation and mosaic. They indicate an abnormality of the cervical vessels, which manifests itself against the background of various pathologies. Gentle puncture is allowed in small areas of the cervix and is manifested in metaplasia. This condition is diagnosed during pregnancy and in girls taking combined oral contraceptives. An accurate result can only be obtained after a histological examination. Rough mosaic and punctuation may indicate the development of cancer, dysplasia and cervicitis.
GRC
The abbreviation CRG refers to cystic enlargement of the glands. The reaction of squamous epithelium after treatment with acetic acid is white. The boundaries of the epithelial junction are not visualized. After treatment with Lugol's solution, leukoplakia is determined; areas rise above the squamous epithelium.
Open and closed glands
In the transcript, colposcopy is defined as coolant and gastric cancer on the cervix. The external opening closes, and mucous contents accumulate inside the so-called nabothian glands. As a result, vasodilation occurs and an inflammatory process develops. The formation of a closed gland or nabothian cyst is ensured. When treated with a vinegar solution, the area turns white.
Acetowhite epithelium
Acetowhite epithelium appears in response to treatment of the cervix with a solution of acetic acid; this sign is considered important when conducting research. Experts warn that it should not be compared with leukoplakia, which has a completely different nature of occurrence.
There are distinct contours on the surface of the acetowhite epithelium; it can be flat or papillary. Doctors associate the intensity of lightening with the severity of the permissible pathological process. The more persistent the color, the more pronounced the pathology of the mucosal vessels. When applying vinegar, pathological signs such as mosaic and punctuation are determined.
Consequences
If iodine-negative areas are detected, the doctor will order a full examination of the patient, because such deformation often indicates the presence of pathology or an increased risk of its development. Depending on the changes detected, the severity of the likely consequences in the absence of treatment changes.
IDD is a marker of dangerous cancerous and precancerous conditions, so the complexity of the situation cannot be underestimated. The woman is indicated for a biopsy to exclude the risk of developing cervical cancer.
Congenital transformation zone (CTZ)
Colposcopic signs of VZT are varied.
In patients undergoing CS, there are no signs of an abnormal formation; only with the Schiller test does a mild iodine negative appear, sometimes extending to the vaginal vaults. In another part of women, this area may be slightly acetowhite. Sometimes the VZT contains a delicate mosaic or finely calibrated vessels over the entire surface.
A biopsy is required. The histological conclusion in most cases is parakeratosis, acanthosis. The malignancy potential of VTD is considered low and no treatment is required. Although other authors cite cases of combination of VZT with CIN. This sign, in our opinion, is more appropriately attributed to anomalous pictures.
Articles
EPIDEMIOLOGY OF CERVICAL CANCER
Lifestyle, bad habits
The first studies on the epidemiology of cervical cancer appeared in the nineteenth century. Rigoni-Stern in 1842 published data based on a study of the death register in Verona from 1760 to 1830. He noticed that cervical cancer was significantly more likely to cause death in married women and widows and was not found in virgins and nuns. This circumstance allowed the scientist to put forward a hypothesis about cervical cancer as an infectious disease. In a study of 13,000 case histories of nuns in Montreal and Quebec, F. Gagnon (1950) noted that cervical cancer was never detected. The author associated these results with the low incidence of inflammatory diseases of the cervix in nuns.
The results of epidemiological studies concerning the role of early onset of sexual activity, early first pregnancy, frequent change of sexual partners, as well as sexually transmitted infectious diseases in the occurrence of cervical cancer have been published. There is now convincing evidence of an increased risk of developing cervical cancer in women who smoke. Some authors (Hellberg, Greenberg, Winkelstein, Brinton) note the relationship of smoking with early onset of sexual activity and frequent changes of sexual partners, others (Hoffman, Sasson) point to the carcinogenic role of nicotine and cotinine contained in tobacco smoke.
Urogenital infections
The role of trauma associated with childbirth and abortion is still being debated. For quite a long time, the statement of R. Meyer (1910) about trauma as an etiological moment of metaplastic processes in the epithelium of the cervix of the uterus dominated. However, it was subsequently found that “local infection, or rather, a combination of these two conditions, is no less important than mechanical trauma in the pathogenesis of cervical cancer” (A.I. Serebrov). For many years, the possibility of a connection between dysplasia and cervical cancer has been discussed, and a higher frequency of detection of nonspecific microflora, including Trichomonas infections and gardnerellosis, has been noted. Examples of such influence have been discussed in relation to Treponema palliddum, Neisseria gonorrhoeae, Chlamydia trachomatis, herpes simplex virus type 2, cytomegalovirus, human papillomavirus. Epidemiological studies have convincingly shown that an indisputable risk factor for the occurrence of precancerous changes and cervical cancer is genital papillomavirus infection.
The concept of the viral nature of cervical cancer has a long history and is inextricably linked with studies of condylomas of various locations. Genital condylomas are described in works on ancient medicine. For many years, it was believed that vulgar, juvenile, and genital warts were caused by the same type of human papillomavirus, with differences in clinical course due to differences in location. Views on the pathology of cervical condylomas were radically revised after Meiisseis, Fortin (1976), Purola, Savia (1976) described genital flat and inverted (endophytic) condylomas, determining their fundamental difference from condylomas of other localizations, and postulated cytomorphological signs of papillomavirus infections: koilocytosis or ballooning of cells, characterized by enlarged, hyperchromatic nuclei surrounded by a clear zone of clear cytoplasm. Later, using electron microscopic, immunohistochemical and DNA hybridization studies, their papillomavirus etiology was confirmed.
Human papillomavirus infection
Currently, more than 100 types of human papillomaviruses (HPV) have been identified. More than 70 types are described in detail. It is a well established fact that certain types of HPV can infect a strictly defined type of epithelium and cause characteristic changes. Thanks to the identification of the multivariance of HPV genotypes, the identification of specific types of HPV, the accumulation of data on the malignant transformation of genital warts and the oncogenic potential of various types of HPV, it became possible to consider papillomavirus as an etiological factor in the development of cervical cancer. Papilloma viruses infect the basal layers of the epithelium. The most “vulnerable” area is the zone of transition of stratified squamous epithelium into columnar epithelium.
Of all the identified types of papilloma viruses, 34 are associated with lesions of the anogenital area. The oncogenic potential of papillomaviruses varies significantly. Based on their ability to initiate dysplastic (precancerous) changes and cancer, papillomaviruses are conventionally divided into groups of “high” and “low” risk of tumor transformation of the infected epithelium. HPV types 6, 11, 42, 43, 44 were classified as low risk types for cancer, types 16, 18, 31, 33, 48, 56 - high risk. Thus, HPV types 6/11 are the cause of genital warts, are often identified in mild and moderate dysplasias and are rarely associated with cervical tumors. In cervical cancer, HPV types 16 and 18 are most often detected (67-93% of cases). Type 18 virus is detected approximately 2 times less frequently than type 16 virus. Papillomavirus type 18 is more often detected in adenocarcinomas and poorly differentiated squamous cell carcinoma of the cervix, has a higher oncogenic potential, and is associated with a rapid rate of tumor progression, a low level of differentiation of the infected epithelium and an unfavorable prognosis compared to other oncogenic types of HPV. However, most authors point out that infection with the papilloma virus alone is not enough to induce tumor growth, and point to the role of cofactors in HPV-dependent carcinogenesis.
The immune system plays a significant role in the pathogenesis of cervical diseases. The pronounced connection of immunological reactions with atypical proliferation of the ectocervix epithelium indicates the influence of cellular and humoral immunity, on the processes that support the existence of background and precancerous diseases, as well as those that provoke their relapses.
Cervical examination
An oncocytological study is a study of scarified smears from the vaginal portion of the cervix and cervical canal. Diagnosis is based on dividing smears into 5 classes (Papanicolaou) or issuing a conclusion according to the international Bethesda system. Papanicolaou classification:
- Absence of atypical cells.
- Cells with signs of atypia are in small quantities.
- Cells with pronounced signs of atypia.
- Suspicion of a malignant process.
- Convincing signs of malignancy.
The main goal of a cytological study is to identify the morphological features of cells that characterize a specific process. There are up to 80 signs of an atypical cell, with about 10 of them being the most constant.