Dermatovenerologist
Khasanova
Alina Rashidovna
8 years of experience
Make an appointment
Hyperkeratosis is a general name for a group of pathologies, the main symptom of which is excessive keratinization of the skin. Cells of the outer, stratum corneum, under the influence of a certain factor, activate the process of division, while the desquamation of dead cells slows down. As a result, the skin is covered with a stratum corneum, the thickness of which varies from fractions of a millimeter to several centimeters. Any part of the body can undergo keratinization, depending on the causes of the pathology.
Classification of cervical hyperkeratosis
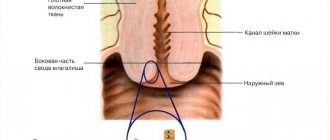
Hyperkeratosis of squamous epithelium of the cervix
Photo.
Leukoplakia (hyperkeratosis) This is keratinization of epithelial cells. White film, clear boundaries, which cannot be removed mechanically. With hyperkeratosis of the MPE (stratified squamous epithelium) of the cervix, all layers are affected: the basal, parabasal, intermediate, and superficial layers. Both part of the mucosa and the entire epithelial layer of the cervix are susceptible to tissue destruction.
Focal hyperkeratosis of the cervix
This is a serious deficiency of female hormones. It looks like clearly defined white spots with a matte sheen on the cervix. This condition is also called pseudo-erosion.
Parakeratosis of the cervix
One of the pathological processes is parakeratosis. This is a change in the mucous layer, a violation of keratinization of the lining of the organ. It is much less common than hyperkeratosis of squamous epithelium. It occurs as a result of injury to the internal genital organs of a woman during rough sex, as well as during medical procedures: installation of a spiral, cleaning, abortion. With parakeratosis, a tissue cell ceases to produce keratohyalin, which is responsible for the elasticity of the epithelial layer, so the mucous membrane is more susceptible to damage and injury.
Cervical dyskeratosis
It differs from other species in that the cells divide chaotically at a high speed, the neoplasms grow and become similar in appearance to cauliflower, which grows on the epithelial layer. Since exfoliation of keratinized cells does not occur, scale by scale they form layers - the size of the neoplasms becomes impressive. Dyskeratosis is dangerous because uncontrolled growth of tumor cells can occur in a short period of time. Human papillomavirus (HPV) and HIV infections are important; they increase the risk of cells degenerating from benign to malignant.
Diagnostics
Often visiting a doctor with cervical hyperkeratosis, a woman hears a result such as a cytogram corresponding to hyperkeratosis of the squamous epithelium. This indicates the presence of the disease and the appearance of one or more white spots on the epithelium of the cervix, indicating layering of the epithelium.
Also, against the background of the disease, the presence of a benign tumor (dermatofibroma) is often detected. In such cases, patients are interested in the question of what dermatofibroma with hyperkeratosis of squamous epithelium means. When diagnosing the disease, the identification of benign formations is not uncommon.
Diagnosis of the disease is carried out using the following methods:
- examination of the patient;
- taking anamnesis;
- ultrasound appointment;
- analysis of the patient’s microflora;
- study of hormone levels in the blood;
- biopsy of samples of the epithelium of the affected areas.
As a result of the research, single accumulations of scales or multiple formations are detected on the surface of the mucous membrane of the cervix. After making a diagnosis and identifying the provoking causes, it is necessary to begin treatment. In such cases, the pathology will have a positive prognosis.
Important! Timely detection of the disease and proper treatment will help avoid complications of the pathology in the future. Often patients, faced with cervical hyperkeratosis, wonder how the pathology is treated
With mild hyperkeratosis, patients are prescribed medications that help restore the natural functions of the epithelium. These may be medications from the following groups:
Often patients, faced with cervical hyperkeratosis, wonder how the pathology is treated. With mild hyperkeratosis, patients are prescribed medications that help restore the natural functions of the epithelium. These may be medications from the following groups:
- probiotics;
- vitamins A and C;
- folic acid.
For more serious forms of the disease, treatment may involve the use of a method such as chemical coagulation. In simple terms, this is cauterization of the affected tissue. This method is used for mild to moderate damage to the epithelium.
In severe forms, surgical intervention is indicated. These could be the following methods:
- Electroconization involves the removal of affected areas of the epithelium using a special surgical loop through which current is passed.
- Cryotherapy - cold is used to get rid of the problem.
- Laser treatment is a method based on the use of laser equipment.
- Ultrasound - irradiation.
- Knife conization – involves the removal of damaged uterine tissue.
- Complete amputation.
Important! Drug treatment is selected by the attending physician based on the examination of the patient and the characteristics of the course of the pathology. Indications for surgery may include severe forms of the disease and precancerous conditions.
https://youtube.com/watch?v=pd4cxZNIMQk
Traditional methods of treatment
Treatment with folk remedies for hyperkeratosis can be used in the form of auxiliary methods of therapy. Popular recipes include the following:
Douching
When the epithelium of the cervix is damaged, various decoctions against the background of medicinal herbs work well. It can be chamomile, calendula, yarrow, celandine. Brew the herb at the rate of one tablespoon per 500 ml. water. Douching is carried out with a warm decoction.
Use of oils
Vegetable oils have a beneficial effect on human mucous membranes. For these purposes, sea buckthorn, olive, and sunflower oil are used. Treatment is carried out using tampons soaked in oil.
Treatment with suppositories
Candles are used based on cocoa butter. To do this, the product in an amount of 150 g is placed in a water bath. After purchasing the oil in liquid form, add a few drops of tea tree oil, 10 drops of calendula tincture, 5 drops of vitamin A (can be bought at the pharmacy). Afterwards, the resulting mixture is poured into specially prepared foil molds to make candles. Candles are placed daily at night. The course is 10 days.
Important! Using folk remedies, you must carefully monitor the condition of your body. With this type of therapy, allergies to one or another component of the drug often occur.
Timely diagnosis of pathology and its proper treatment will help to avoid complications and preserve women’s health for many years.
The danger of cervical hyperkeratosis
The disease poses a threat to the health and life of women . If focal keratosis is not detected during the procedure, the consequence is cervical atrophy. The estrogen hormone is reduced, the epithelium is suppressed, the tissue is smoothed out. Atrophic vaginitis is a common phenomenon. Postmenopause is one of the reasons. Often occurs against the background of cancer pathologies. The most recognizable symptoms are intermittent bleeding, as well as vaginal dryness, and a constant urge to urinate.
Cervical atrophy causes infertility and cervicitis, which is characterized by purulent discharge, pain during intercourse and urination. The uterine pharynx and vagina have an inflammatory process that is often neglected. If a couple wants to have a child, then first it is necessary to cure cervicitis, otherwise the child may be born with developmental disabilities.
But the most dangerous is dyskeratosis. Over a short period of time, uncontrolled growth of tumor cells can occur. Human papillomavirus (HPV) and HIV infections are important; they increase the risk of cells degenerating from benign to malignant.
Leukoplakia of the vulva
During the postmenopausal period, you should not refuse scheduled visits to the gynecologist, since the onset of menopause does not mean that you will never have problems with the female part again. There are diseases that are specific to older women, for example, vulvar leukoplakia. However, it also occurs in young people, although much less frequently.
If a woman feels itching, burning and pain in the external genital area, which intensifies after urination, sexual intercourse and when walking, then it is necessary to consult a doctor. But a specific sign - thin films that can be easily removed with a tampon, or whitish plaques on the skin or mucous membrane of the vulva, cervix or vagina - can only be seen by a gynecologist during an examination.
Description
Leukoplakia of the vulva is a precancerous condition, a dystrophic change in the stratified squamous epithelium. With this disease, the horny and granular layers that are normally absent from the epithelium appear, and para- and hyperkeratosis develops.
Vulvar leukoplakia usually develops during menopause, but recently leukoplakia is increasingly being diagnosed in young women. The danger of this disease is that there is a risk of leukoplakia degenerating into vulvar cancer.
Doctors believe that leukoplakia is a protective reaction of the body to the action of various damaging factors; it is expressed in the too rapid growth of squamous epithelium. Leukoplakia of the vulva occurs against the background of inflammation of the mucous membrane, with endocrine, immune and metabolic changes.
Risk factors for vulvar leukoplakia:
- age over 40 years;
- the presence of chronic inflammatory diseases of the genital organs, HPV and genital herpes;
- cervical dysplasia;
- genital injuries;
- metabolic disorders, diabetes, obesity;
- neglect of personal hygiene;
- vitamin A deficiency.
Leukoplakia of the vulva is divided into three forms according to the severity of hyperkeratosis:
- flat – smooth whitish spots appear on the surface of the vulva, easily removed with a swab, but then appear again. There are no signs of inflammation. This stage does not cause any discomfort to the woman and is detected only during a routine examination.
- hypertrophic - dry grayish convex plaques are visible on the surface of the vulva. Plaques can merge with each other and cannot be removed with a tampon.
- warty - the lesions grow and resemble warts in appearance. This form of leukoplakia is complicated by the presence of erosions, cracks, inflammation and is considered a precancerous condition.
Diagnostics
To diagnose vulvar leukoplakia, visual examination and colposcopy are used. A Schiller test is required. It consists of uniform staining of the mucous membrane with Lugol's solution. Areas of leukoplakia do not stain and become clearly visible to the naked eye. In doubtful cases, a biopsy is performed followed by histological examination.
Treatment
If you are diagnosed with this condition, aim for long-term treatment - leukoplakia is quite difficult to cure. Treatment is complex and includes drug therapy, physiotherapy, diet, and, if necessary, surgery and the help of a psychotherapist.
Leukoplakia sufferers should follow these guidelines to relieve symptoms:
- systematic hygiene procedures without soap, with warm boiled water, preferably using decoctions and infusions of decoctions of calendula chamomile;
- refusal of synthetic underwear - it increases the itching of the genitals and does not allow the body to breathe normally;
- light blanket;
- physical exercise and walks before bedtime;
- diet therapy - refusal of spicy, fatty, fried, smoked, strong tea and coffee, alcohol.
Inflammation and itching are treated with hormones and antiseptics in the form of ointments, creams, and vaginal suppositories. Be sure to prescribe multivitamins.
If there is no effect from conservative treatment, foci of leukoplakia are excised with a scalpel or radio knife (sometimes with a laser or cryodestruction method). If the disease is advanced, then vulva extirpation is performed.
All patients with this disease are monitored by an oncologist in parallel with the gynecologist.
Prevention
Prevention of leukoplakia consists of preventing hormonal imbalances or, if they occur, their timely elimination, treatment of metabolic disorders, infectious and inflammatory diseases of the pelvic organs. It is necessary to undergo an examination by a gynecologist every six months, since in the early stages, when the disease does not yet manifest itself, leukoplakia is easier to cure.
Doctor Peter
Signs of cervical hyperkeratosis and diagnosis
The anomaly as a whole occurs without any symptoms, almost without manifesting itself. The woman’s condition is satisfactory, so diagnosis of keratosis occurs during a visit to the doctor for a routine medical examination. But still, some signs of leukoplakia exist. If an infectious disease of the reproductive system provokes hyperkeratosis, then the following may occur:
- vaginal itching, burning;
- discharge with an unpleasant odor;
- discomfort and pain during or after sexual intercourse.
During the examination, the female doctor discovers damage to the cervical mucosa in the form of white plaques. A whitish coating is localized in the vaginal part, in the vulva area. Gynecology identifies several forms of this disease:
- flat or simple;
- verrucous or verrucous.
If flat leukoplakia is not treated promptly, the pathology degenerates into a warty form and looks like a lumpy lesion of the white mucosa.
Diagnosis
To determine the type of leukoplakia, a number of examinations are carried out. A biopsy, ultrasound, smear for oncocytology and smear examination for histology will most fully reflect the clinical picture. Elements of hyperkeratosis are atypical cells that can develop progressively and turn into cancer. The treatment strategy directly depends on the identified form.
Prevention
To prevent the re-development of hyperkeratosis, it is necessary to care for the skin, ensure its nutrition and hygiene. The following will help prevent relapses of the disease:
- normalization of nutrition, provision of a varied, balanced diet;
- avoidance of prolonged exposure to the sun or hypothermia of the skin;
- hygiene, skin care;
- use of protective equipment when working with chemical reagents.
Some forms of the disease are extremely difficult to treat and remain with a person throughout his life. In this case, it is especially important to pay attention to preventive measures that reduce the risk of relapse.
Causes of cervical hyperkeratosis
Statistical tables show that the popularity of vaginal keratosis among women is growing. Factors of pathological mutations are:
- severe and chronic forms of sexually transmitted diseases;
- long-term course of candidiasis in the vagina;
- contraceptives;
- a large number of abortions or births;
- failure to comply with personal hygiene rules;
- promiscuity;.
- erosion;
- inflammatory diseases, for example, colpitis or vaginitis;
- weak immunity;
- viral diseases.
Treatment of cervical hyperkeratosis
Therapy for keratosis is prescribed individually and depends on the degree of damage to the mucous membrane, localization, and cytology results.
Medication method
Taking medications restores the epithelium and these drugs include:
- pre- and probiotics;
- hormones;
- immunostimulating;
- anti-inflammatory drugs;
- macro- and microelements, vitamins;
- antibacterial agents;
- antiviral drugs.
Surgical method
But in most cases, the problem is solved by surgical intervention:
- diathermocoagulation – thermal cauterization with electric current;
- chemical coagulation - cauterization with acids: “solkovagin” and “vagotil”;
- electroconization – removal using an electric loop;
- laser therapy – the therapeutic use of laser light;
- radio wave therapy is the most highly effective and minimally painful method, in which removal occurs using an electrode with high-frequency waves;
- knife conization - removal of fragments with a scalpel;
- cryodestruction – exposure of the lesion to extremely low temperatures;
- amputation - an organ is removed.
To avoid scars, young women undergo:
- radiosurgical treatment;
- laser vaporization;
- cryo destruction.
It is very important to eat right during treatment. The rate of vitamin A intake is one of the important conditions: pork and beef liver, cheese, cottage cheese, cream, egg yolk, cod or halibut fish oil, also medical. Beta-keratin is found in carrots, pumpkin, apricots, greens and black currants, and the body independently synthesizes retinol from it. It is necessary to remove hot, spicy, salty foods from the diet. To strengthen the immune system, vitamins contained in vegetables and fruits are necessary. Additionally, sexual rest, abstinence from alcohol and smoking, proper rest, and proper hygienic care are prescribed for 4–8 weeks.
Symptoms
It is extremely difficult to independently determine the pathology, so often the patient learns about the diagnosis only at the next preventive appointment with the gynecologist. Among the symptoms, in rare cases, vaginal discharge, which is uncharacteristic for a healthy woman, is noted. As a rule, there are no other manifestations of the pathology.
If we talk about a medical examination, the doctor identifies the disease by white plaques formed on the mucous membranes. In the absence of obvious lesions, but if a disease is suspected, the gynecologist prescribes additional diagnostic measures.
Pregnancy and vaginal hyperkeratosis
A mild degree of leukoplakia does not affect the ability to get pregnant. If the disease has reached a severe stage, then the decision on treatment is made by the doctor individually after examination.
In the case of leukoplakia discovered during pregnancy, there is no need to panic. First of all, you need to take the recommended tests: blood, a smear, a section of the cervix for histology, circicometry, and the abdominal cavity is examined using an ultrasound machine. Keratosis of the cervix is not a reason to terminate a pregnancy. An indication for abortion may be rapidly progressing cancer, and even in this case the week of pregnancy plays a role. Basically, experts insist on continuing the pregnancy. The fetus is regularly monitored for the disease.
Drug treatment is selected depending on the trimester; if therapy is unsuccessful, then surgery occurs after childbirth. If the focus of whitish spots is small, then they can disappear without any drugs or medical procedures, on their own. Women often get scared when they hear a diagnosis, so they immediately want to read information on the Internet about who had it and how they managed to overcome the disease. A forum where the female sex often finds communication can persistently advise folk remedies.
IMPORTANT! Since leukoplakia is considered a precancerous condition, any experiments can be harmful. Before resorting to traditional medicine, you should definitely consult a doctor. Doctors warn that douching with decoctions of medicinal herbs will not only not bring any improvement, but will also worsen the situation and activate the biotransformation of cells. Not so long ago, when treating hyperkeratosis using folk methods, tampons with sea buckthorn, olive or sunflower oil, and douching with decoctions of various herbs were often used. To date, scientists have proven that such manipulations do not bring improvement, but only aggravate the situation and transform cells from benign to malignant.
Hyperkeratosis is no joke. The disease is very serious. To avoid leukoplakia, you need to treat even minor diseases in time, do not expose the internal genital organs to injury (coils, abortions), maintain proper hygiene and do not forget to check with a gynecologist every six months.
Video: What is cervical leukoplakia? (hyperkeratosis)
What is “Cervical Leukoplakia”?
Reasons for the development of pathology
All causes of keratosis development can be divided into two groups. The first includes external influences - tight shoes or clothing that rubs certain areas of the skin, intense physical labor, constant contact with chemicals or other substances that negatively affect the skin, failure to comply with hygiene rules, etc.
The second group includes diseases and pathological conditions that lead to excessive formation of the stratum corneum:
- systemic disorders, congenital or acquired - ichthyosis, diabetes mellitus, psoriasis, keratoderma, etc.;
- circulatory disorders, most often occurring in the lower extremities - varicose veins, obliterating atherosclerosis;
- lack of vitamins;
- fungal diseases of the skin (lichen) and feet;
- gastrointestinal diseases;
- stress;
- excess weight, foot pathologies, lameness.
Under the influence of certain factors in the upper layer of the skin, capillary blood supply is disrupted and innervation worsens. Because of this, the process of cell division in the stratum corneum is activated, with a simultaneous slowdown in their desquamation and the formation of thickened keratinized areas.