Radical treatment of cervical and uterine cancer
Wertheim's operation fully complies with the above requirements. Its essence is to remove the uterus with appendages (fallopian tubes and ovaries), the upper third of the vagina, as well as the ligaments supporting the uterus and the surrounding fatty tissue with lymph nodes.
Indications for surgery are cancer of the cervix and uterine body. But in some cases surgery is not recommended:
- in the presence of distant metastases;
- in the case of a huge size of the tumor, with germination of blood vessels and nearby organs, and sometimes the walls of the pelvis;
- with severe concomitant pathologies;
- in old age.
Preparation and indications for surgery
Surgery can be used as a stand-alone therapy or as part of a combination treatment. If the patient is diagnosed with well-differentiated squamous cell carcinoma at stage T1bN0M0, then Wertheim's operation allows eliminating the pathology without additional chemotherapy or radiation therapy.
Radical hysterectomy is indicated for patients in the following cases:
- Development of a malignant tumor in the uterus;
- Myoma, the size of which exceeds 12 weeks of pregnancy;
- The occurrence of symptomatic uterine fibroids;
- Rapid increase in tumor size;
- Cervical cancer;
- Necrotic changes in the uterine fibroid node;
- Development of uterine bleeding against the background of anemia;
- A history of grade 3-4 adenomyosis;
- Development of submucosal fibroids;
- Gender change;
- The occurrence of chronic pain syndrome in the pelvic area;
- Vaginal and uterine prolapse;
- Ineffectiveness of conservative therapy or therapeutic curettage for endometrial pathologies.
Before surgery, it is important to undergo a comprehensive diagnosis. This will reduce the risk of complications during surgical treatment and in the postoperative period. The examination includes the following manipulations:
- Clinical examination of blood and urine;
- Coagulogram - determination of blood clotting;
- Biochemical blood test. It is necessary to determine the following indicators: total protein, ALT, AST, cholesterol, creatinine, glucose;
- ECG;
- Smears from the vagina, cervix and urethra to determine the microflora and the presence of inflammation;
- Determination of sexually transmitted infections (ureaplasmosis, chlamydia, herpes virus, HPV) using PCR;
- Cytological examination of the cervix;
- Determination of blood type and Rh factor in order to prepare at least 1 liter of blood of the desired type before surgery;
- Colposcopy in the presence of cervical pathologies;
- Diagnostic curettage followed by endometrial histology;
- X-ray of the lungs or fluorography;
- Ultrasound of the pelvic organs;
- Blood test for HIV and syphilis.
If the patient is diagnosed with large uterine fibroids or severe endometriosis, then hormonal therapy is indicated for 3-6 months before surgery. It is aimed at stabilizing the growth of nodes and the progression of pathology.
Important! Before surgery, it is necessary to undergo an examination by a therapist or dentist, and carry out sanitation of carious teeth if necessary.
In the presence of varicose veins of the lower extremities, it is necessary to prescribe appropriate therapy 2-3 months before surgery to remove the uterus and appendages. However, antiplatelet medications should be stopped 10-14 days before surgery.
1 day before the operation, you should switch to table No. 1, which involves eating liquid and pureed food. In the evening and in the morning it is necessary to carry out a cleansing enema. On the day of surgery it is forbidden to drink or eat.
Wertheim's operation for cervical cancer
If we talk about the treatment of this pathology, it should be noted that this operation can be used either independently or as part of combination therapy.
In the case of diagnosing well-differentiated squamous cell cancer (stage T1bN0M0), this operation can radically solve the problem without the use of methods such as chemotherapy and radiation therapy. However, most often the Wertheim operation is a component of a combination treatment.
For uterine cancer (even in stage IB), other methods of therapy are always prescribed, in addition to surgery.
Operation Wertheim: progress of the operation
Surgical intervention for radical removal of the uterus and appendages includes several stages. These include:
- Access.
- Transection of the uterine ligaments.
- Mobilization of fallopian tubes and ovaries.
- Mobilization of the bladder.
- Ligation and intersection of the main supply vessels.
- Removal of tissue from the anterior surface of the cervix.
- Crossing the ligaments that fix the uterus from behind (uterosacral).
- Crossing the cervical ligaments.
- Resection of the cervix.
- Hemostasis of the vaginal stump.
- Peritonization.
Surgical approach
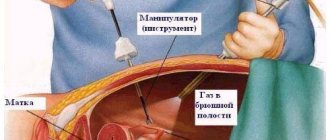
Wertheim's operation is an extensive intervention that requires good visualization of the surgical field and the ability to manipulate without difficulties or restrictions. Therefore, the incision must be adequate. Mini-approaches and endoscopic surgery are not suitable in this case. When it comes to treating cancer, the cosmetic result comes last in importance.
Typically, a median longitudinal laparotomy is performed (dissection of the anterior abdominal wall along the linea alba, bypassing the navel) or the Cherny approach (transverse laparotomy with dissection of the rectus abdominis muscles).
Indications
Removal of the uterus is a major operation, which requires certain indications:
- oncological diseases of the pelvic organs;
- massive uterine bleeding that cannot be stopped;
- loss and prolapse of an organ;
- multiple adhesions after the inflammatory process;
- extensive growth of the endometrium;
- purulent-inflammatory processes that are not amenable to drug treatment;
- long-term erosive changes.
Mobilization of the uterus
For this purpose, the round ligament of the uterus, the proper and suspensory ligaments of the ovary, as well as the uterine end of the tube are intersected. All of these formations should be crossed, if possible, in places devoid of blood vessels. This will reduce blood loss. The uterus itself is taken on clamps and moved to the side.
After cutting the suspensory ligament of the ovary, removal of the uterine appendages becomes possible. The main thing when mobilizing them is not to damage the ureter. To do this, palpation of the broad ligament of the uterus is required during the operation. The ureteral fold is usually easily located on its posterior sheet. This manipulation allows for mobilization of the uterus and appendages without damaging the ureters.
After opening the vesicouterine fold, the bladder is separated from the anterior wall of the cervix with a tuffer. This should be done without deviating from the center line to reduce the risk of injury to the choroid plexus.
If the bladder is fused to the uterus by adhesions, its separation may be difficult. In this case, manipulation begins from the round ligaments and goes to the neck along the areas with the greatest mobility, separating the bladder with scissors.
Next, Wertheim's operation involves ligation of blood vessels. The main vascular bundle of the uterus is the uterine artery and accompanying veins running along the rib of the uterus. Their dressing is carried out at the level of the internal pharynx.
For additional mobilization of the uterus, the prevesical fascia is dissected and tissue is bluntly displaced from the anterior surface of the cervix downwards. Next, ligaments that were previously inaccessible for manipulation are intersected: the sacrouterine and cervical ligaments. After this, the hysterectomy enters its final stage.
Hysterectomy itself, hemostasis and peritonization
The vaginal vault is opened, the cervix is taken with clamps and is gradually cut off from the vagina. After this, hemostasis and peritonization are performed. The vaginal stump cannot be sutured tightly; it can serve as a natural drainage in the event of any pathological processes in the pelvic cavity and accumulation of pus or blood there.
The vaginal tube is treated in a special way. The vaginal walls are sutured with the vesicouterine and rectal uterine folds, as well as with the uterosacral ligaments, thereby achieving hemostasis and peritonization.
Complications arising in the early postoperative period
The postoperative period can be complicated by:
- Infection of sutures (not only skin, but also internal).
- Peritonitis and sepsis.
- Bleeding from the suture area, including internal bleeding.
- Hematomas of the suture area.
- Dysuria.
- PE (pulmonary embolism).
Even the strictest adherence to sterility does not always avoid purulent complications. This is due to the fact that the operation is performed on patients whose bodies are already weakened by the fight against a malignant tumor and whose immunity is reduced. Therefore, inflammation of their sutures is a possible situation. In order to prevent this condition in the postoperative period, a course of antibiotics is required.
Bleeding and the appearance of hematomas indicate insufficient hemostasis. Prescribing hemostatic drugs is not always enough; sometimes repeated surgical intervention is required - revision of the wound and suturing of bleeding vessels.
Dysuria is frequent and painful urination. The appearance of this symptom is possible when the mucous membrane of the urethra is damaged by a catheter and traumatic urethritis occurs.
PE can occur as a complication of thrombosis of the veins of the lower extremities. That is why, in the postoperative period, anticoagulants (Heparin) are prescribed and the wearing of compression stockings or elastic bandages is recommended.
Recovery period
The duration and severity of the postoperative period depends on many factors: the individual characteristics of the body, the severity of the disease, preparatory measures and the type of operation.
Rehabilitation measures aimed at eliminating complications and accelerating the body’s recovery processes are as follows:
- the first days after surgery are accompanied by severe pain, to relieve which analgesics are used;
- wearing compression garments and taking anticoagulants help avoid thromboembolic complications;
- to restore blood volume, infusion therapy is prescribed;
- treatment of postoperative wounds and timely dressing are the main methods in the fight against infection;
- abstinence from sexual intercourse must last for at least 6 weeks.
Nutrition plays an important role for a woman in the period after hysterectomy. The work of the gastrointestinal tract in a stressful situation for the body is suppressed. Therefore, it is important to adhere to the principles of proper nutrition for a positive effect on the gastrointestinal tract.
Doctors also recommend rational physical activity. Starting from the second day after surgery, the patient is advised to walk daily. Light exercise and breathing exercises are effective ways to adapt the body. However, it is important to remember not to overexert yourself or do exercises that require effort.
Consequences of the late period
There are also certain complications after Wertheim’s operation that develop in the long term:
- Emotional problems: fear of possible changes in appearance and loss of sexual desire (after all, the ovaries have been removed, which means the level of sex hormones has been changed), worries about the inability to get pregnant, an unsightly scar on the anterior abdominal wall.
- Adhesive process of the abdominal cavity.
- Climax.
- Vaginal prolapse.
- Formation of retroperitoneal lymphocysts.
A woman’s worries about the consequences of a hysterectomy are understandable. Therefore, in the postoperative period, the support and understanding of loved ones is very important.
You just have to come to terms with some complications (postoperative scar, inability to have children). Other fears can and should be fought, as they are often unfounded. Removal of the ovaries does not entail any drastic changes in appearance or sexuality. However, discomfort may occur during sexual intercourse if the vaginal stump is too short after hysterectomy.
Adhesions after Wertheim's operation are formed in the same way as after any abdominal surgery. This is due to trauma to the peritoneum during surgery, which leads to the formation of connective tissue cords between its sheets and internal organs.
The adhesive process in the abdominal cavity can cause abdominal pain, problems with urination and defecation, and in some cases even lead to intestinal obstruction. To prevent the formation of adhesions in the postoperative period, early activation of the patient and physical therapy on the first day after surgery are important.
Menopause after hysterectomy occurs due to the removal of the ovaries. Postoperative menopause is naturally more difficult to bear, because in this case hormonal changes occur abruptly. Hormone replacement therapy is used to reduce discomfort.
And vaginal prolapse after Wertheim's operation becomes possible due to damage to the ligamentous apparatus (a necessary condition for performing a hysterectomy) and displacement of the pelvic organs to the place of the missing uterus. To prevent such a complication, the patient is recommended to perform special gymnastics, wear a bandage, and limit physical activity for at least 2 months after surgery.
Often, a lymphocyst forms in the retroperitoneal space after Wertheim's operation. Its treatment is surgical. However, it is much more effective to prevent the occurrence of this complication at the stage of surgery than to treat it. For this purpose, various methods of drainage of the retroperitoneal space are used.
When is Wertheim's operation prescribed for cervical cancer?
Article last updated 12/07/2019
Methods of surgical treatment of cervical cancer (CC) became widespread and scientifically justified at the beginning of the twentieth century. Ernest Wertheim made a significant contribution to the treatment of oncological pathologies of the reproductive system. Today, most operations for cervical cancer are performed using his method. Surgery for cervical cancer is independent or used in complex treatment.
Diagnostic methods
When carrying out preparatory measures for Wertheim’s operation, the doctor must know with a high degree of accuracy the prevalence of oncogenesis (localization, area, depth), the morphofunctional state of the adjacent structures, and predict the compensatory capabilities of the patient’s body. To solve these problems, the following studies are carried out:
- examination using gynecological speculum;
- bimanual rectovaginal;
- Ultrasound of the urogenital and lymphatic drainage systems;
- radiography;
- cysto-, hystero- and colposcopy;
- examination of the rectum and lower parts of the sigmoid colon using a sigmoidoscope.
If necessary, an extensive examination of the kidneys, bladder, colon and other organs of the peritoneum and pelvis may be prescribed.
Data obtained from CT, MRI, PET, laparoscopy help increase the information content of research methods, but their result is not a basis for revising the stage of cervical cancer.
The stage is determined based on the results of the initial examination of the patient and cannot subsequently be changed.
Preparing for surgery
Oncology can be provoked or occur against the background of an infectious process of acute or chronic form. An important stage of preoperative preparation is the sanitation of detected lesions.
To ensure unhindered access to the surgical field and prevent complications in the postoperative period, the gastrointestinal tract is cleaned.
If there is a risk of thrombosis, preventive treatment using antiplatelet drugs is prescribed.
Brief description of the method
The operation, in essence, is an extended extirpation (total hystrectomy) of the uterus with (or without) appendages, part of the vagina, periuterine tissue and adjacent lymph nodes. At the stage of preparation for surgical intervention, a gauze swab is installed in the patient’s vagina, and catheterization is performed to drain urine.
The operation is performed under general anesthesia, epidural anesthesia, or a combination of these methods. The patient is positioned on the operating table set at an angle of 30-45° with the pelvis elevated and the head end lowered (Trendelenburg position). Transperitoneal access is provided by a midline laparotomy or transverse (if the patient is obese) incision.
The doctor inspects (examines) organs, structures, systems of the peritoneal and retroperitoneal space. Depending on the condition of the organ, the presence and location of metastases, the surgeon:
- places clamps on the ligaments of the fixing apparatus of the uterus and ovaries, stretching them, and dissects them;
- slightly releases and displaces the bladder;
- removes uterine common and external lymph nodes with surrounding adipose tissue. In the presence of secondary foci of carcinogenesis, all pelvic lymph nodes are excised;
- separates and bypasses the superior cystic artery;
- uterine vessels are dissected and alloyed (ligated);
- releases and displaces the rectum;
- the uterus is separated, dissected and the cardiac ligaments are ligated;
- the mat, after these stages of the operation, is fixed exclusively with the genital tube;
- performs partial (at any level) or total resection of the vagina. The upper third of the reproductive tube must be removed;
- after removing the internal reproductive organs, suturing the stumps and draining the surgical field;
- the remaining part of the mesosalpinx leaf is fixed with sutures to the back wall of the vagina, and the peritoneum covering the bladder is fixed to the front wall;
- drains the cavity;
- the wound hole in the abdominal wall is completely sutured.
The disease is not a death sentence - in case of uterine cancer, Wertheim's operation gives a high rate of patient survival - in stage IB without the formation of secondary foci in regional (located nearby) lymph nodes it is 85-90%, and in the presence of metastases (IV-IIA) - 50%.
Cancer patients with complicated cervical cancer and lymphogenous metastatic process in the pelvic lymph glands, deep penetration (penetration) of tumors into the stoma and tissue are subject to radiotherapy or chemoradiotherapy during the rehabilitation period. This increases their survival rate by up to 60%.
Method modifications
Modern modifications of surgical therapy for microinvasive cervical cancer suggest:
- surgery with preservation of the appendages, since with squamous cell cancer they are involved in the carcinogenic process in less than 1% of patients;
- preservation of part of the vagina, since in patients amenable to surgical treatment, the middle part of the reproductive tube is rarely involved in the malignant process, and it is sufficient to remove its upper third;
- total resection of regional lymph nodes and adjacent tissue, while removal of parietal lymph nodes of the lumbar region is carried out only when indicated;
- if appropriate, leave the lateral third of the cardiac ligaments and the surrounding part of the paravaginal tissue.
These methods make the operation less traumatic while maintaining its effectiveness.
Complications
Surgery during such a complex, extensive and invasive operation requires the surgeon to have knowledge in related specialties - phlebology, urology, proctology, so that he can eliminate any complications that arise during the intervention. Common perioperative complications are injuries to organs (bladder and ureters, colon and small intestine), and great vessels, which the specialist eliminates during the work.
At an early stage of postoperative recovery, the following may occur:
- hemorrhage;
- blockage of the pulmonary artery by an embolus;
- blockage of the intestinal lumen as a result of adhesions.
Long-term consequences of surgery are:
- formation of fistulas – urethro-vaginal and vesico-vaginal;
- hypotension and atony of the detrusor and ducts, leading to the development of an ascending infectious process;
- the occurrence of lymphocele in the retroperitoneal space.
Among postoperative complications, infections of both the surgical field (wound) and urological tracts predominate. The use of modern methods of antibacterial therapy can reduce the risk of this type of complications from 77% to 15%.
Adhesions after surgery occur due to the formation of an extensive wound surface, injury to organs, insufficient blood supply, tissue hypoxia, and fluid accumulation. They are diagnosed in 60-90% of cases and occur within 3 days after surgery. In 40% of cases, adhesions after surgery are the cause of chronic pelvic pain.
What they say about Wertheim's operation
To radically get rid of cervical or uterine cancer, Wertheim's operation is used. Reviews about it vary.
Doctors and patients note positive aspects after surgery:
- Increased life expectancy.
- Guaranteed absence of uterine diseases, including cancer.
- Contraception that prevents even a small chance of unwanted pregnancy.
- The operation does not reduce performance, and it is possible to return to a full life.
- Inability to have children.
- An unsightly scar on the anterior abdominal wall.
- Possibility of complications, both early and late (discussed above).
Removal of the uterus using Wertheim's procedure
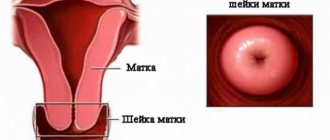
Wertheim's operation is an intervention that is performed in case of cervical cancer. This disease is characterized by the fact that the mucous membrane of the cervix is affected in the place where the cervical epithelium passes into the vaginal epithelium. The operation involves getting rid of not only the pathology itself, but also healthy organs of the female reproductive system, which include:
- the fallopian tubes;
- ovaries;
- the uterus itself;
- ligaments and lymph nodes;
- upper third of the vagina.