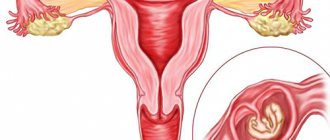
How does a normal pregnancy occur? The egg and sperm meet to form an embryo. The fertilized egg is implanted into the wall of the uterus, where it develops over the next 9 months of pregnancy.
Cost of services in our clinic
| Appointment with a gynecologist with the highest category | 1000 rub. |
| Consultative appointment with a doctor based on test results and ultrasound results | 500 rub. |
| Extended colposcopy | 1500 rub. |
| Amino test for bacterial vaginosis | 300 rub. |
| Medical abortion (all inclusive) | 4500 |
| Make an appointment by phone: 8-800-707-15-60 (toll-free) |
| *The clinic is licensed to remove tumors |
However, in some cases, successful fertilization does not lead to the desired result. This occurs when the embryo attaches to the walls of any organ other than the uterus. This condition in gynecology is called ectopic pregnancy and is considered the most dangerous pathology.
Previously, treatment for ectopic pregnancy required removal of the organ where the embryo began to grow, which often led to loss of reproductive function.
Modern methods of early diagnosis and treatment of ectopic pregnancy make it possible to preserve the patient’s internal organs and avoid dangerous health consequences. If treatment is delayed, you can lose not only the fallopian tube, but also your life.
What is an ectopic pregnancy and what happens?
A pregnancy is called ectopic if the embryo does not implant in the uterus. Usually the egg is implanted in the fallopian tube. Tubal pregnancy accounts for more than 98-99% of all types of VB. There are right-sided and left-sided ectopic. Rarely, pregnancy can develop in the ovary, in the abdominal cavity, and even in the cervix. There is also a classification based on the place of attachment of the fertilized egg in the tube.
Depending on the timing of the discovery of the pathology during the operation, doctors can save the tube, remove it partially or entirely, there is a possibility of removing the tube along with the ovary. Sometimes an ovarian resection is performed. This is when not the whole, but only part of the ovary is removed.
All organs can be saved only if the pipe has not burst, before surgery. If a fallopian tube ruptures, it is unrealistic to save the fallopian tube for further conception.
Predisposition to ectopic pregnancy
Who is more likely to have an ectopic? The list helped to compile both my own experience and my neighbors in the hospital bed. After all, everyone has their own history and background. The attending gynecologist also contributed to the creation of the article. You have a predisposition to an ectopic pregnancy if at least one item from the list below is in your biography.
- Previous operations in the abdominal cavity (adhesions).
- Sexually transmitted infections.
- Any inflammation of the female genital organs.
- Tubal ligation (there is still a gap).
- Chlamydia (impaired movement of the egg to the uterine cavity).
- There is already a history of ectopic.
- Tumors, polyps.
- Congenital anomalies of the female reproductive organs.
- Tubal plastic surgery (any operation related to the tubes).
- Pertubation (blowing of the fallopian tubes).
- Hysterosalpingography (X-ray contrast agent is injected).
- Hormonal disbalance.
- Endometriosis.
- Endocrine disorders.
- Women over 35 years old.
There are many risk factors. Don't be alarmed, not all of the above are high risk.
Symptoms of ectopic pregnancy
- Lower abdominal pain.
- Loss of consciousness.
- Dark bloody discharge (brown spotting).
- Heavy bleeding (cervical pregnancy).
- Decrease in blood pressure after a painful attack.
- Cold sticky sweat.
- When the pain stops, a revolution in the intestines begins (irritable bowel syndrome).
- Positive pregnancy test.
The pain can be dagger-like or moderate intensity. I didn't have very bad pain. There was a brown daub. I lost consciousness for a few minutes on the second day after the painful symptom. Then I felt almost normal throughout the day. Girls, don't believe the relief. This is the calm before the storm. You need to run to the doctor as soon as possible, or better yet call an ambulance right away.
I was admitted to the hospital only on the third day. The rupture occurred on the second day after the pain syndrome. On the same day, pain and bloating began all over my stomach. Life was saved only by the fact that the blood loss was small - the pipe was twisted. Everyone's blood loss is different. You can go into shock and die from blood loss. So under no circumstances should you delay.
Children from ectopic pregnancy: about random exceptions
Despite all the “buts” and risks of history, there are known cases of ectopic pregnancy, which turned out to be possible to save. Women diagnosed with ectopic pregnancy became mothers. The women not only remained alive and healthy, but also miraculously gave birth to babies. Examples are rare and are more likely the result of a happy coincidence than an achievement of doctors. So far, several such cases have been recorded in the world over the past few decades.
In Russia this happened by absolute accident. A woman in labor was admitted to the hospital at 36 weeks with suspected appendicitis with acute abdominal pain and nausea. Doctors decided to operate on the patient to remove appendicitis. There was no limit to surprise when, instead of an appendix, they found a child in the abdominal cavity. An obstetrician-gynecologist was involved in the operation. The doctor recorded that the baby was alive and ready to be born.
The boy's height was 51 cm, weight 2750 g. The operation lasted several hours, the child turned out to be weak, but viable. Today he is growing and developing on par with his peers.
The happy mother of the baby said that during pregnancy she was seen at the antenatal clinic and had several ultrasound examinations, but the doctors did not see any pathology. This fact can be explained by the difficulty of diagnosing the diagnosis with the unusual position of the fetus and placenta in the abdominal cavity. If the doctors saw a problem during the examination, the pregnancy would be terminated. The doctors' misconception helped the child to be born, although not without risk to the mother's health.
Another unique case occurred almost 20 years ago in London. The baby was born as a result of an ectopic tubal pregnancy. The boy developed in the tube, in parallel with two sisters who were placed in the uterine cavity. The pathology was discovered only at 18 weeks, which is already a phenomenal period of “life” for such a pregnancy. The doctors decided to continue the pregnancy until the required term. The birth was successful at the scheduled time by caesarean section. The girls were born first, followed by a boy who formed a fertilized place in the fallopian tube.
Another variant of the successful outcome of a tubal ectopic pregnancy, although this time without childbirth, was recorded in the USA. The expectant mother was given a terrible diagnosis at 27 weeks. Doctors discovered that the fetus grows and develops in the intestinal omentum. They decided to remove the child for subsequent development in artificial conditions. The chance of survival was only 2%, but that was enough for the baby. He coped, survived and grew up to be a healthy, full-fledged person.
The operation was carried out by more than three dozen doctors, considering the case extraordinary. It is possible that the expectant mother’s faith in miracles played an important role here, because the successful outcome was the exception to all the rules.
HCG for early ectopic pregnancy
Human chorionic gonadotropin, hCG, is a hormone produced by the baby's placenta, the placenta, throughout the entire period of gestation. In addition to nascent life, human chorionic gonadotropin is synthesized by tumor cells, ovarian germ cells and the pituitary gland during menopause.
Some resources write about the production of the hormone from the first hours of fertilization, which is not true. In order for the hormone to begin to be produced, the fertilized cell must attach and the placenta must begin to form. It is she who produces human chorionic gonadotropin. Within a few hours the placenta does not form. So I don’t recommend running to the laboratory 2 days after sex.
The hCG level helps the doctor distinguish between normal ectopic pregnancy in the early stages and pathology in the later stages.
Few women know, but the analysis is divided into several: β-hCG total and β-hCG free. At up to 4 weeks of pregnancy, you can donate blood for total β-hCG. It is determined from the sixth day of conception. A general analysis is also performed after an abortion. There is also a quantitative urine test for hCG.
The European laboratory Sinevo notes hCG analysis for the diagnosis of ectopic pregnancy (5-18 weeks of pregnancy).
The indicator is only relevant until the fallopian tube ruptures. Otherwise, any value of the analysis is no longer meaningful. Fallopian tube rupture occurs between 4 and 6 weeks in most cases.
Only a doctor deciphers the meaning of hCG, and not a friend or a website from the Internet.
Moreover, to diagnose an ectopic pregnancy in the early stages, you need not just one hCG analysis, but several over time. Dynamic tests should be taken in the same laboratory, since analyzers and test systems may be different. The hCG level should double in two days if the fetus is developing correctly and in its place. If the growth is less than expected, there is a suspicion of VB.
Contraindications
There are a number of contraindications for surgical intervention:
- comatose state of the patient;
- cardiovascular diseases;
- respiratory diseases;
- hernia of the anterior abdominal wall.
In rare cases, laparoscopy is performed for symptoms such as:
- large blood loss into the abdominal cavity - more than 1 liter of blood;
- adhesions on internal organs;
- scars and cicatrices from previous operations;
- obesity.
In this case, laparoscopy can be replaced by laparotomy. In the presence of peritonitis or various infectious diseases, laparoscopy is also contraindicated due to the high risk of possible consequences. Laparoscopy cannot be performed if the fetus is large or if there are malignant neoplasms. Then a laparotomy is performed.
If a woman has a cervical ectopic pregnancy, a circular suture is placed around the cervix, then curettage is performed to preserve the uterus. Curettage can be used for diagnostic purposes if symptoms of pregnancy are present and the fertilized egg is not detected during an ultrasound examination.
What does a low hCG level mean?
- Pregnancy does not develop.
- Placental insufficiency.
- Threat of spontaneous miscarriage.
- Post-maturity (in later stages).
- The child died (in the later stages).
- Patau syndrome.
- Edwards syndrome.
- Anencephaly.
- Ectopic pregnancy.
- Early toxicosis.
As you can see, a doctor may suspect a lot of things. Additional examinations are required for differentiation. Low hCG levels and spotting do not always mean an ectopic pregnancy. Perhaps there is a threat of spontaneous miscarriage and you need to go to the hospital for conservation.
When the discharge is not associated with a pathological pregnancy
Discharges of a pathological nature can be observed not only when the embryo is located incorrectly. Something similar happens with cervical erosion, diseases of the female genital area (inflammatory), and endometritis. It is important to identify in time the absence or presence of an ectopic pregnancy, as it is life-threatening.
In addition to the presence of pathological secretion, there are other signs (toxicosis, pain in the lower abdomen, the appearance of discharge that does not fit into the cycle).
Nature arranges it in such a way that discharge serves as a warning to a woman about the appearance of problems in the reproductive system. You cannot ignore them, since in the case of ectopic pregnancy there is a high risk of not only losing the chance to subsequently give birth to a baby, but also death. Therefore, contacting a specialist for any ailments is the key to health.
Will the test and hCG show an ectopic pregnancy?
It is generally accepted that the test will show a faint second line if it is ectopic. Many people write this, but I went through all this and I’m willing to bet. The test showed two clear lines on the 7th day of the delay, and a week later I was lying on the operating table. A pregnancy test shows the presence of a fetus, but not its location.
Most tests show the total hCG molecule rather than the β subunit. Therefore, there are also false positive tests.
It doesn’t matter what time of day you do the test and what the concentration of urine is. This fact does not affect the presence of human chorionic gonadotropin.
The hCG blood test is more accurate, but there are features and difficulties in making a diagnosis in the early stages. The level of hCG during an ectopic pregnancy differs from its natural course.
Treatment of pathology
“Treatment” of pathological pregnancy, regardless of its characteristics and duration, is carried out in a medical institution. Only doctors, having assessed the nuances of the situation, all the symptoms, based on tests and examination, will decide which method should be used. If an ectopic placement of the fetus is detected, several standard methods of eliminating the situation are used.
- If an ectopic pregnancy is detected early, the elimination methods are gentle, and in the case when the fetus (and not its remains) is still inside, laparoscopy is used, which is performed through a mini-puncture of the abdominal wall to insert an instrument. The essence of the procedure is to gently suction the embryo without damaging the tubes (which is important for subsequent conceptions). Equipment with a system that displays all actions on a monitor.
- Some situations require surgery. If the fallopian tube ruptures, a salpingectomy (removal) is performed, which allows saving the woman’s life. Sometimes it is left and stitched after removing the affected part, which does not eliminate the likelihood of a recurrence.
- If an ectopic embryo is detected at an early stage, medical termination with Methotrexate is used. It causes a forced abortion, when the fetus is expelled along with the bleeding.
We can say that in each specific case of pathological conception an individual approach is taken. This condition is dangerous due to complications leading to death due to inflammation or bleeding. Because of it, there is a high risk of secondary ectopic pregnancy, infertility, adhesions, inflammatory diseases of not only the reproductive, but also the excretory system, as well as the abdominal cavity.
Even with high-quality treatment, in some women subsequent conception may also be abnormal. Therefore, in case of a tendency to abnormal localization of the fetal egg, it is reasonable to undergo a comprehensive examination, which will identify its specific causes. For example, inflammatory diseases, if the fallopian tubes are affected, then the next pregnancy may also be pathological.
After removal of an ectopic pregnancy, compliance with medical recommendations is mandatory. Rehabilitation after a pathological conception is quite long; restorative therapy and elimination of the causes of the pathology will not hurt.
After removal of an ectopic pregnancy, high-quality OC is important, and it is better to refuse the IUD, since it often provokes pathological attachment of the embryo. In case of repeated conception, the second tube may be damaged, which threatens definite infertility (but IVF is a possible option). According to statistics, more than half of women affected by ectopic pregnancy subsequently have a successful history of conception. The next pregnancy is permissible no earlier than after a six-month period. Minimum relapses with medication interruption.
HCG table by week and ultrasound for ectopic pregnancy
Different laboratories use different research methods and the numbers may vary significantly.
HCG table
| Weeks after conception | Tolerant value |
| 1-2 | 16-156 |
| 2-3 | 101-4870 |
| 3-4 | 1110-31500 |
| 4-5 | 25000-820000 |
| 5-6 | 23100-151000 |
| 6-7 | 27300-233000 |
| 7-11 | 209000-291000 |
| 11-16 | 61000-103000 |
The range in one week is significant. There are women who compare their own analysis with the reference value of the table, with the norm. You should not compare your results with the results of the tables, even if the units of measurement are the same. The equipment is different in laboratories and the indicators are designed for a specific research method. Units in analysis are not indicators. If you see units of mIU/ml, it is not a fact that you were tested with a similar test system.
Ultrasound is an additional diagnostic method, puncture
Laboratory findings do not constitute a diagnosis. For accuracy, an ultrasound is prescribed. Ultrasound examination is more informative if Doppler is used. A transvaginal ultrasound will show pregnancy at 3 weeks from the date of conception. At the slightest suspicion of VD, an ultrasound should be performed immediately. The presence of a fertilized egg in the uterine cavity will reassure the expectant mother. If the embryo is not in the uterus, the attachment site in the fallopian tube can be seen on the monitor. True, for this you must have a good apparatus and an intelligent specialist.
If VD is suspected, a puncture is performed through the posterior vaginal fornix. The presence of blood that does not clot provides a diagnosis.
During my life I had to experience the puncture on myself twice: once under anesthesia and the second without anesthesia. The pain is terrible without pain relief. Tears flowed naturally, although I consider myself to be a patient category of people. It's good that I didn't have to feel the pain for long. The procedure is done with a tool that resembles a knitting needle.
How does hCG increase during an ectopic pregnancy? HCG for IVF
Gynecologist Viktor Evseevich Radzinsky writes in his book that hCG during an ectopic pregnancy grows less than normal. The hormone increases 1.5 times in 48 hours with VB. If everything goes well, it grows 2 times.
The number of children in the womb matters. If there are twins, then the hCG will be higher and will increase in proportion to the twins. Triplets will give an increase in hCG dynamics three times more, unlike a singleton pregnancy.
If you took an hCG test in the fourth week, then after 48 hours it must be repeated in the same laboratory. Having 2 results in hand, we can talk about a possible VB.
With IVF, ectopic pregnancy can occur. The growth of hCG during IVF will differ from conventional fertilization, since the patient receives injections of a hormonal drug for implantation of the embryo.
Conclusions after the experience gained. Save the fallopian tube yourself
If I had had this knowledge many years ago, I would not have had to lose my fallopian tube and part of my ovary. It is clear that getting pregnant and giving birth with one tube is more difficult.
It is possible to save a tube during an ectopic pregnancy!
It is indeed possible to save all organs if the diagnosis is made in time. Treatment for VB is always surgery, but not everything is always removed. When VD is diagnosed early, laparoscopy is performed. Through three small holes in the abdomen, the embryo is removed from the tube, and the fallopian tube is sutured. If the embryo has implanted in the part of the fallopian tube next to the ovary, then it is possible to extract it without cutting the fallopian tube. You won't lose organs if you take steps and prepare for motherhood before you get pregnant.
- Do hCG over time every 48 hours to 5 weeks. Radzinsky says that at 4-6 weeks the pipe most often ruptures, then it can no longer be saved. Less commonly, tube rupture occurs at 8 weeks. I broke in the fifth week.
- Ultrasound at 3-4 weeks.
- Examination by a gynecologist as soon as you find out about pregnancy.
- Stop smoking.
- Use protection during sexual intercourse before planning a baby.
- Agree to laparoscopy if the ultrasound shows no fetus in the uterus and the test is positive.