- Indications
- Preparing for surgery
- Carrying out
- What happens after surgery?
- Complications
- Postoperative follow-up
- Pregnancy after trachelectomy
All over the world, standard treatment for cervical cancer consists of removal of the uterus, chemotherapy and radiation therapy.
However, for young women who want to maintain the ability to bear children, an alternative operation has been developed - trachelectomy, or removal of the cervix. What is trachelectomy and is it possible to get pregnant after it?
To ensure that the outcome of cervical removal is favorable, the selection of patients for this procedure is critical. During the operation, the cervix, upper 2 cm of the vagina and adjacent tissue are removed. The body and vault of the uterus remain intact. The intervention can be performed through the abdominal cavity, laparoscopically, or using robot-assisted surgery. It is possible to remove the cervix through the vagina.
The first successful operation was performed in 1994. Over the past time, at least 1000 such interventions have been carried out, after which at least 250 women were able to become pregnant.
There are two types of operations:
- Simple with removal of part of the cervix and vagina.
- Radical with additional excision of lymph nodes in the pelvis, where cancer cells may be located, as well as the parametrium (tissue around the uterus).
The treatment method is accompanied by a low risk of complications. The tumor recurrence rate does not exceed 5%.
Indications
Surgery is indicated not only for cervical cancer. It is performed in the following pathological conditions:
- recurrent cervical cysts and polyps, chronic endocervicitis;
- cervical endometriosis;
- a small node of fibroids in the cervix;
- cervical deformation and ectropion caused by the unfavorable course of previous births;
- prolapse or prolapse of the uterus, causing thickening and deformation of the cervix;
- severe leukoplakia or pseudoerosion that cannot be treated by other means.
The cervix is often removed in cases of grade 2 and 3 dysplasia - precancerous processes of the cervix. Conservative methods at this stage are usually no longer effective, and there is no need for complex surgical intervention.
In 1998, the following indications for removal of the cervix were formulated:
- the patient’s desire to maintain the opportunity to have a child;
- tumor less than 2 cm in size;
- FIGO stage 1A1, 1A2 and 1B1;
- uninvolved upper part of the cervical canal, as proven by MRI;
- absence of metastases in the lymph nodes.
If at least one of these conditions is not met, partial removal of the cervix while preserving the organ is impossible.
Tumors larger than 2 cm are usually accompanied by involvement of lymphatic vessels and nodes, as well as the cervical canal. This increases the frequency of tumor relapse and the likelihood of metastases.
The operation is not performed on patients with the following histological forms of cervical tumors:
- neuroendocrine tumors;
- papillary-serous formations;
- sarcomas.
Before performing neck removal, it is important to exclude metastatic disease of the lymph nodes. To do this, before the main operation, lymph nodes are removed laparoscopically, through small incisions in the abdominal wall. If cancer cells are found, the entire uterus is removed.
Which method of hysterectomy is better?
It is impossible to say unequivocally which method of extirpation is worse and which is better. Each of them has its own advantages and disadvantages. For example, laparoscopic and vaginal hysterectomy are easier to tolerate by patients, since they do not involve layer-by-layer dissection of the abdominal wall. However, in oncological practice, open intervention is often required, since a thorough examination of the pelvic organs, and in some cases the abdominal cavity, is necessary to search for cancer metastases and radical removal of all interested tissues.
The extent of the operation is determined by the diagnosis and stage of the disease. The most extensive interventions are performed for ovarian cancer, since it is prone to early contact metastasis through the peritoneum. Therefore, during the operation, not only extensive extirpation of the uterus and appendages is performed, but also excision of the greater omentum and peritoneum.
Preparing for surgery
A blood test, its biochemical composition and the state of the coagulation system are examined. An X-ray of the lungs is performed. To evaluate metastases in the lymph nodes, CT, MRI or positron emission tomography is performed. When diagnosing inflammatory diseases, the infection is treated until complete recovery.
Before removing part of the cervix, doctors determine whether the patient is suitable for such an operation. She is then explained in detail that during the operation, damage to blood vessels, ureters and other organs may occur, which may require immediate laparotomy.
Alternative treatment methods are discussed: cervical conization, hysterectomy, chemoradiotherapy.
In some patients, right during the intervention, it is necessary to expand its volume and remove the uterus if metastases to the lymph nodes are detected.
The woman is hospitalized on the day of the operation or the day before it. She should not eat or drink 6 hours before the intervention. Some medications may be administered as prescribed by the doctor.
The patient signs a consent form for the operation, which contains information about possible complications.
Relapse
Conization is not a panacea for a complete cure. If a woman has concomitant diseases, especially human papillomavirus, dysplasia may develop again. According to medical statistics, 70% of patients diagnosed with human papillomavirus experience a relapse after some time. As a rule, when it occurs again, it is more difficult and develops more rapidly.
The most unfavorable outcome is the presence of cancer cells in the test soft tissue sample taken from the cervix during conization. In this case, drug therapy is carried out aimed at stopping the further development of the pathological process.
If this process is started and left without treatment, complications will begin. Subsequently, it will be necessary to resort to extensive surgery, during which the woman’s reproductive organs affected by cancer cells are removed.
Carrying out
Before surgery, antibiotics are recommended to prevent infection. Sometimes an enema is performed or the patient takes a substance that cleanses the intestines in advance. This depends on the type of intervention contemplated.
A woman should take a hygienic shower. Sometimes pubic hair removal is required. Jewelry, glasses, contact lenses, and piercings are removed.
The patient is placed on a surgical gynecological chair. General or local anesthesia is used. Epidural anesthesia is often performed.
Trachelectomy is performed in one of three ways:
- Removing part of the neck in the form of a cone.
- Wedge resection.
- Amputation with vaginal vault transplantation.
To perform the operation, various instruments can be used: scalpel, laser, electric current, cryodestructor or radio knife. The choice is made by the doctor depending on the capabilities of the clinic and the characteristics of the patient.
How long does cervical removal surgery take?
Depending on the type of intervention – from 30 minutes to 4 hours.
Vaginal removal
First, several pelvic lymph nodes are removed using laparoscopy. They are examined for the presence of malignant cells. If there are no metastases, the cervix is removed. The probability of detecting malignant cells in the lymph nodes at an early stage is 6%.
Radical vaginal trachelectomy is performed most often and consists of 5 stages. First, a local anesthetic drug with a vasoconstrictor effect is injected under the mucosa and a circular incision is made 2 cm below the neck. The anterior and posterior edges of the mucosa are clamped.
The space between the uterus and rectum is then opened and treated. After this, the tissue between the uterus and bladder is opened.
Radical trachelectomy
The ureters and uterine vessels are isolated, and the periuterine tissue is removed. With a simple trachelectomy, the parametrium is not excised. They try to preserve the blood supply to the uterus as much as possible. The arteries leading to the cervix are ligated. The cervix is incised at a level of 1 cm below the internal os.
The removed area of the cervix is urgently examined under a microscope. If cancer cells are found at a distance closer than 5 mm from its edge, the operation is considered ineffective, its volume is expanded and the uterus is removed.
Removal of part of the cervix
At the final stage, they try to restore the cervix as much as possible using non-absorbable materials. Subsequently, such a stitch, partially covering the cervical canal, helps to maintain and carry out pregnancy. A rubber catheter is left in the cervical canal, which is subsequently removed. The edges of the vaginal mucosa are sewn to the cervix.
Cavity removal
Abdominal surgery to remove the cervix is performed with a low horizontal or vertical incision in the abdominal wall.
The opened abdominal cavity is carefully examined in search of metastases. All pelvic lymph nodes on both sides are removed. They are immediately assessed using the frozen section method. If malignant cells are found in them, extensive surgery is necessary.
The ligaments of the uterus and ureters are distinguished. The vaginal part is opened through the posterior surface of the uterus and the outer surface of the cervix is removed. Stitches are applied.
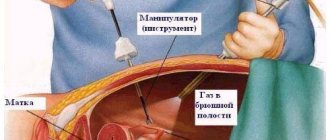
Laparoscopic surgery
Thin instruments in the form of tubes and optical devices are used. The surgeon makes short incisions in the abdominal wall. The laparoscope is inserted through these small holes and the cervix and adjacent tissue are removed under video control. This operation is the least traumatic for the patient. After it, a quick recovery is dismissed.
Types of surgery
Conization of the uterine cervix can be carried out in the following ways:
- radio wave method using an electric knife;
- laser;
- cauterization with liquid nitrogen – cryoconization method;
- operation with an ordinary surgical scalpel.
The attending physician decides which method of surgery to choose. The method is selected depending on the stage of dysplasia and whether the patient has concomitant pathologies that must be simultaneously removed. An important role is played by the patient’s age and the number of births, since some techniques are more or less traumatic.
Knife method
The method, when the cervix is partially excised with a simple surgical scalpel, is performed extremely rarely today. The reason is the high risks of complications:
- formation of scars on soft tissues;
- opening of uterine bleeding;
- long period of tissue healing after surgery.
It is also possible that a woman will develop infertility due to injury to the soft structures of the cervix. But this method also has an undeniable advantage, unlike many other methods. During surgical conization, high-quality biological material can be obtained, which after the operation is sent to the laboratory for research.
If a woman has a history of childbirth, she no longer wants to have children, and dysplasia develops rapidly, surgical conization can be performed.
Laser method
Laser dysplasia is treated by burning out pathological tissues of the cervix by directing a laser beam at them. The advantage of this method is that it is bloodless, painful and uncomfortable sensations are reduced to a minimum. After the operation, the patient recovers faster and easier.
Disadvantages of the procedure: the likelihood of severe burns to adjacent soft tissues; the operation is performed using general anesthesia, since it is necessary to completely immobilize the woman so as not to disturb the laser beam. Another disadvantage of the procedure is its high price.
Radio wave technology
Radio wave conization of the cervix involves burning out pathological tissues by influencing them with high-frequency current. The radiosurgical conization method is carried out using a special instrument, which is a loop of an electrode.
The advantage of the method is the ability to use local anesthesia; the patient will experience a slight feeling of discomfort. There is no risk of burns to adjacent soft tissues. The risks of complications are reduced to a minimum.
Nitrogen use
This technique involves freezing tissue with liquid nitrogen, which leads to natural destruction. The method is absolutely safe, there are no risks of complications, as with other methods.
Despite its low cost, this technique is rarely used. The reason is that it is not possible to take samples of biological material for further laboratory study, which is extremely important in cases where dysplasia is rapidly developing and there is a likelihood of serious complications developing.
What happens after surgery?
The patient is in the recovery room for several hours or overnight, then she is transferred to the department. She can get up, walk, eat food and drink water the same day after the doctor's permission. Protein and dairy products are especially useful.
If for some reason the patient must constantly lie down, she needs to do breathing exercises and raise her legs to improve venous blood flow and prevent the formation of blood clots.
The urinary catheter is usually removed soon. If bladder function is not restored after this, the catheter may be left in place for several days. Through it, urine enters a special plastic bag - a urinal.
If non-absorbable suture materials were used, the sutures are removed 5-10 days after the intervention.
A woman may experience constipation and bloating, sore throat, and bleeding from the vagina. This is not dangerous. It is advisable to do a light foot massage and breathing exercises, as well as use compression stockings. Hospitalization lasts approximately 7 days. At this time, antibiotics, painkillers and anti-inflammatory drugs are prescribed.
If conventional painkillers are ineffective in the first days, 2 options can be used:
- Epidural anesthesia.
- Controlled anesthesia, when the patient himself, by pressing a button on a special pump, regulates the flow of anesthetic into the vein.
All tissues and lymph nodes removed during surgery are examined in the laboratory within 2 weeks. If metastatic foci are found in them, additional consultation with a doctor will be required. It will decide on radiation therapy or surgery to remove the uterus.
After discharge, the woman is bothered by fatigue and should get more rest. She is encouraged to walk, but jogging and swimming are prohibited. Domestic activities such as washing dishes and preparing simple meals are allowed in the first month after surgery. You can drive a car one and a half months after the operation. Around this time, you can return to normal work and a normal sex life.
If abdominal rather than vaginal surgery was performed, the recovery period is extended to 3 months until the sutures are completely healed.
Main restrictions after conization
In order for the cervix to heal quickly, without negative consequences and complications, a woman must follow the following medical recommendations:
- sex is prohibited for a month. This is due to the fact that vaginal sex will damage the tissue of the cervix and cause bleeding;
- taking a bath, visiting saunas and steam baths, solariums, and performing any procedures that involve exposure to heat on the body are excluded;
- It is prohibited to engage in sports and other vigorous physical activities, or lift heavy objects;
- do not take medications from the group of anticoagulants that thin the blood, for example, Aspirin, so as not to provoke bleeding;
- Vaginal douching and the use of tampons are strictly prohibited.
If there is bleeding after surgery, you can only use pads that need to be changed regularly. It is prohibited to visit public pools and swim in natural bodies of water. Only a doctor can tell you when sex will be allowed, after a routine examination a month after the conization.
The normal duration of discharge after conization is 2 to 3 weeks. After a week and a half, the volume of blood released may increase significantly; this is normal. This is explained by the fact that a scab comes off from the cervix. Increased discharge should not have an unpleasant odor. When you start menstruating again after conization depends on the presence of complications. If there are no complications, menstruation will occur as usual, at the woman’s usual time. A slight deviation in the cycle for a few days is allowed.
Immediate complications
The postoperative period and the first weeks after removal of the cervix may be accompanied by complications:
- inability to completely empty the bladder due to decreased tone;
- pain during sexual intercourse;
- vaginal discharge;
- bleeding;
- deep vein thrombosis, pulmonary embolism;
- infectious complications and inflammation of sutures;
- decreased skin sensitivity on the thighs;
- painful or irregular periods;
- swelling of the external genitalia, including the labia, clitoris and vaginal opening;
- vaginal candidiasis;
- prolonged absence of menstruation.
Prevention of these complications:
- Sexual activity is permitted after 6 weeks, when a follow-up medical examination has been performed and the first menstruation after the intervention has passed.
- During the same period, douching, vaginal tampons, hot baths, swimming, and lifting weights of more than 3 kg are prohibited.
- In the first six months you need to protect yourself from pregnancy.
To alleviate her condition after discharge, it is better for a woman to take care of a supply of food in advance and discuss household chores with loved ones.
If, after removal of the cervix, the lower abdomen hurts, discharge with an unpleasant odor appears, your health worsens, or your temperature rises, you should immediately consult a doctor. Normally, the discharge can last 6 weeks; it is spotty, brown in color, and painless. If bright red discharge or clots appear, you should consult a gynecologist.
Pain during and after surgery
Conization of the uterine cervix itself is a painless procedure. But as soon as the local anesthesia wears off after the intervention, the patient will regain her previous sensitivity, and she may experience minor pain in the lower abdomen that is nagging in nature.
After 1-2 weeks, as the soft tissues heal, the uterus will begin to contract intensively, which will be accompanied by cramping pain. The pain is of medium intensity and is easily tolerated by most women. As a rule, patients do not need to take painkillers. If the pain is intense, the doctor prescribes painkillers and antispasmodics.
Postoperative follow-up
The first doctor's examination is scheduled after 2 weeks. In this case, a vaginal examination is not performed. The woman is informed of the results of a biopsy of the removed tissue. A plan for further observation and treatment is discussed.
Pap tests and colposcopy are performed every 3-4 months for the first 3 years after the intervention. Then control examinations are performed once every six months for 2 years.
The doctor pays attention to the appearance of long-term side effects of the operation, which may appear even several years after the intervention:
- accumulation of lymph in the vessels of the extremities (lymphostasis) or in the abdominal cavity (lymphocele) due to removal of the pelvic lymph nodes (this complication is especially typical for situations where trachelectomy was combined with radiation);
- stress urinary incontinence due to activities that increase intra-abdominal pressure, such as sneezing;
- problems with conception and a high risk of pregnancy complications.
Why is it better to perform high cervical amputation at the Swiss University Hospital?
- Our clinic actively uses gentle techniques to preserve a woman’s reproductive function; treatment tactics are selected strictly individually for each patient.
- At the Center for Operative Gynecology, more than 1,500 unique operations are performed annually, some of them were developed by our specialists and are performed only in a few clinics in the country, including ours.
- The clinic has a team of highly qualified professionals who regularly conduct master classes in leading clinics not only in Russia, but also in Europe. Our surgeons also serve as experts in professional associations and societies.
- SHUK has accounted for more than 600 children born after organ-preserving gynecological operations and treatment of chronic infertility.
- An important component of any operation is the use of modern anti-adhesion barriers, which are included in the mandatory surgical protocol. Therefore, the risk of adhesions is minimized; patients, even after complex operations, retain the ability to conceive and bear children.
- In patients with several pathologies, it is possible to perform simultaneous operations - simultaneous surgical treatment of several pathologies at once.
Pregnancy after trachelectomy
For women who have undergone cervical removal, pregnancy is recommended no earlier than 6-12 months later. Approximately 15% of patients experience difficulties associated with narrowing of the lower part of the cervical canal. In this case, they are shown assisted reproductive technologies, for example, in vitro fertilization.
During pregnancy, the risk of miscarriage does not increase. However, the incidence of preterm birth increases as a result of a shorter cervix or the development of chorioamnionitis. This leads to premature rupture of the membranes. 4% of women give birth before 32 weeks of pregnancy, and 55% give birth after 37 weeks. To avoid premature termination of pregnancy, additional stitches are placed on the cervix or special holding devices - pessaries - are used.
There is no vaginal birth; the baby is born by caesarean section.
Despite the fact that many centers around the world successfully use trachelectomy in young women, there is still no evidence of its effectiveness. Therefore, such an intervention does not belong to standard treatment and is performed by highly qualified gynecological oncologists only if the patient persistently desires to give birth to a child in the future, if she meets all other criteria for suitability for such an organ-conserving operation.
Doctor's comment
Are you scheduled for surgery for high cervical amputation or are you just undergoing examination? You are probably interested in what this type of operation is, whether reproductive function will be preserved and many other questions. In our clinic, we always strive, if possible, to perform organ-preserving and gentle operations. Modern equipment, the use of the world's best consumables and, of course, an individual approach to treatment are our advantages. We practice complete pain relief using modern drugs, and you can also count on a short recovery period. All our efforts are aimed at not only stopping the pathological process, but also preserving reproductive function. This is possible if the disease is detected at an early stage. In advanced cases, the likelihood of childbearing is significantly lower. That is why you should not delay the start of treatment. Make an appointment and together we will consider all possible treatment methods in your case and discuss in detail every detail of the upcoming treatment.
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov