Uterine fibroids are a pathology of a tumor nature, dependent on the hormonal regulation of the menstrual cycle, which is expressed in the formation of a uterine myometrial node. Fibroids are the most common gynecological ailment in women of reproductive age.
Like any other disease, uterine fibroids have their own code according to the international classification of diseases. The international classification of diseases is abbreviated as ICD.
Currently, the ICD 10 code for uterine fibroids is D25. However, this is a general code that characterizes fibroids as one of the diseases according to the international classification.
Uterine fibroids are a little-studied disease, despite numerous ongoing studies and existing hypotheses of its occurrence and progression. Its ICD code has been revised several times.
Classification
Uterine fibroids occur due to hypertrophy of muscle and connective tissue elements.
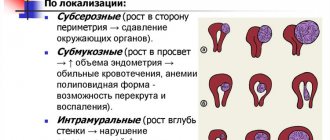
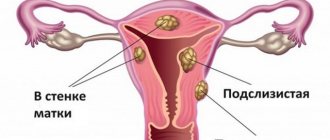
Myomatous nodes can be multiple or single, from a few millimeters to tens of centimeters. Based on their location relative to the parts of the uterus, they are distinguished:
- intramural - located directly in the thickness of the uterine wall, in the muscle layer (myometrium);
- submucous - under the mucous membrane, increasing towards the inner surface of the uterus;
- subserous - protrude above the outer surface of the uterus, increasing in the direction of the abdominal cavity;
- intraligamentous – between the broad ligaments of the uterus.
ICD 10 uterine fibroids, unspecified – Uterine fibroids
Classification of uterine fibroids is the determination of the type of formation by the number of nodes and by location in the uterus.
Please note that this text was prepared without the support of our Expert Council.
Fibroids classification by number of formations:
- Single node.
- Multiple nodes.
- Neoplasms located under the mucous layer, closer to the organ cavity - submucosal nodes.
- Localized in the muscle layer - intermuscular, intramural, interstitial nodes.
- A subserous formation forms under the outer serous layer of the organ.
- A neoplasm between the broad ligaments of the uterus is an intraligamentary node.
- Formation in the tissues of the cervix of an organ is a cervical node.
Consultation by e-mail will help you get more information on the classification of benign cervical tumors and uterine fibroids, ICD10 and treatment methods.
Classification of uterine fibroids according to ICD 10 in adult women is an international classification of diseases in which medical diagnoses are coded. Uterine fibroids in ICD 10 are coded D25.
You can find codes in the ICD for fibroids of the uterine body and cervix of the reproductive organ using a sequential search:
- Class - neoplasms - neoplasms C00-D48 will open.
- The disease belongs to benign neoplasms – D10-D36.
- Uterine fibroids ICD code – D25
Uterine fibroids code according to ICD 10
When the first signs of the disease appear, a woman needs to make an appointment and undergo a full examination. It is very rare, but there are cases of the formation of a benign leiosarcoma node, a malignant neoplasm, inside the tissues.
When treating fibroids, the ICD 10 code is indicated in the patient’s card; the code contains all the data about the type of fibroids. ICD 10 is revised periodically (every 10 years) under the guidance of the World Health Organization.
The ICD fibroid code is an alphanumeric code system that includes all types of disease and has replaced the old digital system. Diagnosis and treatment are provided by fibroid treatment clinics.
The main activity of the clinics is the prevention and diagnosis of the disease; the efforts of doctors are aimed at preserving the reproductive function of women. Organ-preserving techniques are used as treatment: UAE, laparoscopic and hysteroscopic myomectomy.
UAE is a minimally invasive method, does not require general anesthesia, no incisions or punctures are made on the anterior abdominal wall, and after the procedure there is a quick recovery process. EMA gives women a chance to have a child.
Sources used: www.mioma.ru
Coding of uterine fibroids according to ICD 10
Uterine fibroids are a benign neoplasm that is localized in various parts of the organ and affects the myometrium.
The standard ICD 10 code for uterine fibroids consists of the following characters: D25 . This combination encrypts several variants of nosology:
- submucosal location of disease (Supplementary Figure 1);
- intramural, that is, passing through all layers (number 2 after the dot);
- subserous pathology (Supplementary Figure 3);
- unspecified type of disease (number 9 after the dot).
In the International Classification of Diseases, 10th revision, a benign tumor of the uterus is called leiomyoma or fibromyoma.
The pathology code allows you to highlight the standards of diagnostic measures, patient management protocols, preventive measures and other features.
This classification allows us to improve the provision of medical care throughout the world, since the code for uterine fibroids in all countries will be the same.
Features of the course of the disease
A benign neoplasm is a plexus of smooth muscle fibers that intertwine with each other, forming a specific knot.
The size of the tumor is not limited, so the nodes can grow up to several kilograms of weight and compress the surrounding tissues in the body of women, negatively affecting the blood supply and the functioning of the pelvic organs.
The disease predominantly affects women after the age of 30, during active fertility.
Myoma of the uterine body develops in the vast majority of cases. Less commonly, the tumor is localized in the cervix. The node can be single, but multiple forms of pathology occur.
The clinical picture does not always appear, so the disease is often detected during annual preventive examinations by a gynecologist.
The most characteristic manifestations of pathology:
- heavy bleeding outside of menstruation;
- increased intensity of hemorrhages during menstruation;
- anemic syndrome due to blood loss;
- pain in the lower abdomen (cramping during menstruation, but sometimes constant);
- a feeling of squeezing or bursting in the pelvis (typical for large sizes of the node);
- dysfunction of the bladder or rectum (if diagnosed untimely).
In some cases, the disease is complicated by torsion of the pedicle of the fibromatous node, which is accompanied by a sharp attack of pain and requires immediate surgical intervention.
Treatment protocols
In ICD 10, uterine fibroids have additional coding, like all neoplasms, based on histological examination data. The obtained biopsy results, the localization of the tumor and the severity of bleeding allow us to determine treatment tactics.
In 80% of cases, the gynecologist chooses a wait-and-see approach, during which any changes in the progression of the tumor process are monitored.
Rapid growth of the node and other signs of deterioration of the process (worsening of the clinical picture or its appearance) provide grounds for starting conservative therapy with hormonal drugs, for example, oral contraceptives.
Severe blood loss, a nascent fibromatous node, and lack of improvement from medications are indications for surgical treatment. During the operation, a node or multiple formations are removed.
In rare cases, when the process is advanced to life and there is profuse bleeding, hysterectomy is performed.
Save the link, or share useful information on social media. networks
Sources used: mkbkody.ru
Codes for uterine fibroids and other neoplasms according to ICD 10
The main way to organize all types of diseases and health problems is the classification accepted throughout the world, which is abbreviated as ICD.
It helps the doctor, regardless of the country in which he practices, to find the same approach and indicate an understanding of the nature of the disease. It is thanks to such a system that experience is exchanged and medical science is improved.
The table shows the classification regarding uterine fibroids in the ICD, tenth revision. It also presents other benign neoplasms localized in the genital area of a woman. Coding of fibroids, as well as other ailments, is based on the data obtained from histological studies.
Uterine leiomyoma or fibroma (this also includes neoplasms M 889 and the nature of the formation code /0)
A benign disease with damage to the uterine smooth muscle and fibrous layer.
It is located directly under the layer of the mucous membrane and protrudes into the lumen of the uterus, most often leading to infertility
Localized in the thickness of muscle fibers, it accounts for 90% of all diagnosed formations
Located on the outer surface and can press on other abdominal organs
Sources used: cistitus.ru
Types of submucous fibroids
About a third of cases are fibroids with submucosal localization.
Important! Submucous fibroids are considered the most unfavorable type of benign tumors. Due to sufficient blood supply, they can reach significant sizes in a short period of time. The danger of this type of benign neoplasm is the increased incidence of infertility. They account for about 35% of all diagnosed cases. When pregnancy occurs, the risk of miscarriage, spontaneous abortion, premature birth, malposition of the fetus, and complications during childbirth increases. Therefore, it is important to diagnose the disease in a timely manner and carry out the necessary treatment.
The classification of submucosal formations is based on the volume they occupy in relation to the myometrium, which helps in choosing treatment tactics. Highlight:
- Type 0 – nodes are located entirely in the body of the uterus;
- type 1 – 50% is located in the thickness of the myometrium, and the remaining part is in the cavity;
- Type 2 – more than 50% is located in the thickness, and a smaller part is in the cavity;
- Type 3 – there is no myometrial layer between the endometrium and the tissues of the tumor node.
Consequently, type 2 submucous uterine fibroids are a benign neoplasm of the female genital organs, localized in the submucous membrane, mostly located in the thickness of the myometrium.
Additional facts
Necrosis of the myomatous node is characterized by necrosis of tumor tissues due to torsion of the fibroid stalk or disruption of its vascularization.
Necrotic changes can occur in nodes of any location - submucosal, subserous, intramural. The incidence of necrosis of the myomatous node in gynecology occurs in 7% of all cases of uterine fibroids. Signs of cystic degeneration or necrosis are found in 60% of plannedly removed myomatous nodes. In necrotic tissues, swelling, hemorrhages, degeneration, and aseptic inflammation develop. Further progression of necrosis of the myomatous node can lead to peritonitis.
Types of necrosis of myomatous node.
Based on morphological characteristics, in gynecology it is customary to distinguish between wet, dry and red necrosis of the myomatous node. Wet necrosis is characterized by softening and wet necrosis of tissue in which cystic cavities form. Dry necrosis of a myomatous node is characterized by shrinkage of necrotic areas of the tumor with the formation of cavernous cavities in these areas with remnants of dead tissue. Red necrosis usually affects intramural myomatous nodes in pregnant and recently given birth women. Macroscopically, with red necrosis, the myomatous node is colored reddish-brown, has a soft consistency, dilated veins with thrombosis. Against the background of aseptic necrosis of the myomatous node, infectious inflammation usually develops due to lymphogenous or hematogenous introduction of microbial pathogens (staphylococcus, Escherichia coli, streptococcus). Infection of necrotic nodes is associated with the risk of developing peritonitis or a generalized form of infection - sepsis.
Necrosis of myomatous node
Reasons for education
The causes and pathogenesis of submucous fibroids of the second type, like other types, have not yet been precisely studied. There are several hypotheses about what factors can trigger the development of the disease. It is known that an excess of female sex hormones - estrogens - in the body, in most identified cases predisposes to the appearance of this type of formation.
Frequent abortions, complications during childbirth, inflammatory diseases of the female genital organs, hereditary predisposition, absence of pregnancies and childbirth in women under 30 years of age, late onset of menstruation, endocrine disorders (diabetes mellitus, thyroid disorders), excess body weight, frequent stress and long-term use of hormonal contraceptives can also lead to the development of the disease.
In each individual case, the patient’s heredity, lifestyle, and health should be studied. Knowing the possible causes will help prevent relapse in the future.
Short description
Uterine fibroid (UF) is a limited benign tumor consisting of smooth muscle and fibrous connective tissue elements. The tumor can be single, but more often multiple nodes are detected (sometimes up to 10 or more); hormonal dependent. Statistical data . Found in 4–11% of all women, 20% of women over 30 years of age and 40% of women over 50 years of age.
Code according to the international classification of diseases ICD-10:
- D25 Leiomyoma of the uterus
Symptoms
Important! The disease can be asymptomatic for a long time. The clinical picture is most pronounced when the nodes reach significant sizes. Regular visits to the gynecologist (at least once a year) and following the recommendations will help identify the disease at earlier stages.
Patients with type 2 submucous fibroids mainly present the following complaints:
- for menstrual irregularities;
- prolonged and heavy menstrual bleeding with short intervals between them (hyperpolymenorrhea);
- the appearance of clots during menstruation (menorrhagia);
- painful menstruation (algomenorrhea);
- the appearance of intermenstrual bleeding (metrorrhagia);
- weakness and general malaise due to iron deficiency anemia due to prolonged menstruation;
- cramping pain in the lower abdomen. The node is foreign, so the uterus tries to get rid of it - hence the cramping pain. Sometimes it can come out on its own, which is always accompanied by severe pain and heavy bleeding. This is especially true for large nodes of types 0 and 1;
- enlargement of the abdomen due to the rapid growth of the myomatous node.
In the case when the submucous formation reaches a very large size, the cyclicity of menstruation is disrupted, and subsequently menstruation may not stop at all.
If the nutrition of the tumor is disrupted, if it is bent or the leg is torsed, an acute condition occurs that requires immediate medical attention.
Submucous fibroids in most cases lead to infertility, so it is very important for everyone to know the manifestations of the disease. The earliest diagnosis in women of reproductive age allows preserving the opportunity to become pregnant.
Diagnostics
The doctor can suspect the presence of a pathology already at the stage of a gynecological examination, by asking the patient about existing complaints and directly during the examination on the chair. By palpation, you can directly feel the node itself; if it is large enough, the uterus will be enlarged. Pressing directly on the area where the lesion is located may cause pain.
Non-invasive instrumental methods are used for diagnosis:
- Ultrasound (ultrasound diagnostics). Using a transabdominal or transvaginal sensor, the neoplasm is clearly visualized, how and where it is located, and its size and features are determined. This is a completely painless and quite informative diagnostic method.
- Ultrasound with Dopplerometry allows you to determine the characteristics of blood flow in the formation and the surrounding area;
- Hydrosonography. Based on the use of ultrasound with a contrast agent. Allows you to differentiate a myomatous node from a uterine polyp.
- CT (computed tomography). The use of computed tomography makes it possible to detect the disease at the earliest stages. This method is often used to evaluate large tumors.
- MRI (magnetic resonance imaging). Allows you to obtain a three-dimensional image in three projections. The most sensitive diagnostic method, however, is one of the most expensive. Using MRI, you can obtain the most accurate and reliable information about the tumor.
- Hysterography (X-ray). This method is used less and less in modern medicine. On X-ray, the tumor appears as a defect with clear contours. The disadvantage of the method is the difficulty of differentiating a submucosal node from a polyp, a nodular form of adenomyosis and uterine cancer.
Diagnostic hysteroscopy is used as an invasive method. By introducing an endoscopic device into the uterine cavity, the location of the myomatous node, the nature of the surface, the width of the base, and consistency are determined.
Treatment
Thanks to the advent of laparoscopic and endoscopic myomectomy, it has become possible to remove the myomatous node without removing the uterus, therefore it is possible to preserve reproductive function.
The laparoscopic method is an access to the abdominal cavity, when instruments and a laparoscope (an optical system that allows the surgeon to display images of internal organs on a screen) are inserted through small incisions (up to 10 mm). Surgery using a laparoscope is low-traumatic, postoperative complications are rarely observed, patients recover faster, and the cosmetic defect is so small that it is practically invisible.
Important! Surgical removal of submucosal fibroids is the most effective treatment strategy. If you refuse surgical treatment in the early stages of tumor growth, then in the future the likelihood of undergoing radical surgery to remove the tumor along with the uterus increases.
In the treatment of type 2 submucous fibroids, two-stage conservative myemectomy is used. It is based on the use of the laparoscopic method in combination with electrosurgical and laser hysteroresectoscopy. Hysteroresectoscopy involves the introduction of a special electrocoagulator (or laser) device through the vagina and cervical canal. During the operation, the tumor is removed layer by layer, minimally affecting healthy tissue. An important point in preparing for surgery is the use of hormonal therapy, which will stop menstrual function and, by reducing the endometrium, the size of the node itself will decrease.
Radical surgery involves removing the uterus with the cervix (total hysterectomy) or without the cervix (subtotal hysterectomy).
The prognosis after surgical treatment is favorable.
Uterine fibroids: diagnosis and treatment methods
Uterine fibroids
30.11.2017
3.3 thousand
2.2 thousand
7 min.
Uterine fibroids (ICD-10 code: D25) are especially susceptible to women aged 40-50 years. Recently, the disease is increasingly being diagnosed in young patients, adolescents and even children.
There are submucosal, intramural, subserous leiomyomas. Myoma nodes are localized inside or outside the uterine cavity. Accompanied by pain, bleeding and discomfort in the pelvic organs.
Treatment is prescribed in the form of medications or surgery.
Uterine fibroids
Uterine fibroids are a benign formation that appears in the muscular layer of the uterus - the myometrium. Its other name is fibroid, leiomyoma or fibromyoma. Depending on the location of the formation and size, it manifests itself with severe pain or bleeding. Currently, the disease has become younger and begins to occur in women 20-30 years of age.
The size of the formation can be from a pea to 7 cm in diameter. In rare cases, it reaches the size of a five-month fetus. Localization is possible in different parts of the uterus. Myoma is not an oncological formation; it does not transform into a cancerous tumor. Cells are equivalent to healthy cells in the body. The formation consists of muscle and fibrous tissue.
But it often requires treatment.
According to ICD-10, this diagnosis is characterized as D25 (leiomyoma) and has subcategories. After examination, medical workers diagnose patients with:
Diagnosis Code according to ICD-10
| Submucosal leiomyoma of the uterus | D25. 0 |
| Intramural leiomyoma of the uterus | D25. 1 |
| Subserous leiomyoma of the uterus | D25. 2 |
| Leiomyoma of the uterus, unspecified | D25. 9 |
Submucosal leiomyoma appears deep in the uterus, under a thin layer of mucous that lines the organ cavity. The nodes are formed in the form of cysts, on a stalk. Sumbucosis is removed using hysteroscopy.
It is this form of fibroids that most often causes prolonged and severe symptoms in the form of long, painful menstruation with clots. Perforated bleeding between cycles is possible.
Sometimes they are so abundant that a woman develops anemia, weakness, headaches, shortness of breath, and an increased pulse rate.
Intramural is the most common form. It develops in the middle muscle layer and is capable of enlarging the uterus lengthwise and across. Symptoms include menstrual irregularities, a feeling of heaviness and pain in the lower abdomen.
Subserous - develops in the subperitoneum. A foreign body grows from the outside of the uterus into the pelvic cavity. Usually the menstrual cycle is not disrupted, but discomfort is felt as it puts pressure on surrounding tissues.
In most cases, the development of leiomyoma occurs due to hormonal disorders, which subsequently lead to the growth of endometrial nodes. There is evidence in medical research that leiomyoma nodes begin to form after surgery.
Adult women who several years ago had an abortion, curettage, or cesarean section during childbirth seek help from a doctor. The size of fibroids is calculated in weeks, the same as the age of the pregnant woman's fetus.
Ultrasound diagnostics helps to identify nodes at an early stage.
Women who have suffered from inflammatory diseases of the pelvic organs at least once in their lives are at risk of developing fibroids. Sexual infections also provoke their occurrence. But the main cause of fibroids is the consequences of mechanical damage to the uterus, including low-quality intrauterine devices.
One of the factors is the lack of harmony in intimate life, as well as orgasm during sexual intercourse, when the rush of blood after arousal does not disappear, but stagnates in the pelvis, causing vascular tension and venous stagnation (one of the causes of pain during sexual intercourse). If a woman does not experience satisfaction from sex for a long time, this can provoke hormonal imbalance and the development of fibroids.
Rarely, fibroids occur in girls during adolescence, during puberty. The nodes at this time are mostly single, ranging in size from 2 to 4.5 cm.
The majority had inflammatory processes in the female genital organs before the disease. With the development of fibroids in this age group, dysmenorrhea (severe pain during menstruation) begins.
Surgical laparoscopic intervention is used for treatment.
It has been noticed that fibroids often recur in women from generation to generation. If the grandmother and mother had the disease, most likely the girl from this family is also susceptible to it.
Symptoms of leiomyoma vary from woman to woman. This depends on the size and location of the myomatous node. More often than not, several signs of fibroids occur at once. Due to the pressure of the tumor on neighboring organs, painful sensations appear. Aching pain radiates to the lower back, perineum, and groin area.
Sometimes during menstruation they become unbearable. During sexual intercourse, a woman feels discomfort. With sumbucous leiomyoma, when the nodes are located deep in the uterus, they are cramping and long-lasting.
When the nodes are located deep in the walls of the uterus, as with intramural fibroids, the pain is prolonged and aching in nature, especially during menstruation.
The most common symptom of this disease is bleeding. Basically, these are long, heavy periods, which often lead to anemia.
Pallor appears on the face, even with minor physical exertion - shortness of breath and dizziness. Bleeding may begin during the intermenstrual period.
Postmenopausal women may also experience bleeding after exercise. Sometimes it's just spotting.
With prolonged pressure from fibroids on neighboring internal organs: the rectum, bladder, women begin to suffer from constipation, bloating, and frequent urination. There is a high risk of bacteria entering the bladder and causing infection.
The main goal of diagnosing and treating uterine leiomyoma is to detect it at the first stage. In this case, it can be cured without surgery.
This is especially true for women of childbearing age.
When a disease is detected, it must be differentiated from an ovarian tumor and uterine cancer.
An experienced gynecologist will identify fibroids during an examination. In 90% of cases the diagnosis is made accurately. Myoma can be felt by palpation, one or more dense nodes are clearly identified.
Additional methods are used in diagnosing the disease:
- 1. Ultrasound of the pelvic organs. It clearly shows the size and location of the nodes. Deformation of the uterine cavity, if present, is visible. An ultrasound also determines the thickness of the endometrium (often fibroids occur along with existing polyps or endometriosis).
- 2. Hysteroscopy. A special device - a hysteroscope - examines the cervical canal. The method has proven itself in determining the submucosal or intramural form of leiomyoma.
- 3. Laparoscopy. For advanced fibroids, it is used to detect secondary changes, such as hemorrhage and tissue necrosis.
- 4. Curettage of the uterus for diagnostic purposes. It is done for any form of myoma to establish the exact pathology of the endometrium and exclude diseases such as uterine cancer.
The therapy is carried out by a gynecologist. After diagnosis, conservative or surgical treatment is prescribed.
The choice of treatment method depends on the stage of the disease, the size of the fibroids, and the age of the patient. They also take into account whether the disease is progressing, the presence of chronic pathologies and the possibility of preserving reproductive function.
The underlying cause of fibroids is hormonal imbalance. Therefore, patients are prescribed medications containing hormones.
One of the groups is drugs that suppress the production of pituitary hormones of the gonadotropic group. COCs, antiprostagens and GnRH agonists, antigonadotropins, gestagens are prescribed, for example:
- Marvelon;
- Novinet;
- Mercilon;
- Regenidon;
- Ovidone;
- Lindinet;
- Logest.
Prescribing these medications reduces the risk of uterine bleeding and pain in the lower abdomen. Reduction of nodes when treated with drugs of this group can be achieved in the early stages of the disease, when they do not exceed 15 mm in size. Therefore, this group of medications is not a priority in the treatment of fibroids.
The second group is agonists. They provoke inhibition of gonadotropic hormones, which causes menopause:
- Decapeptyl;
- Diferelin;
- Decapeptyl - depot;
- Zoladex;
- Sinarel;
- Buserelin;
- Lucrin - depot.
For large growths, medications help reduce the size of the nodes. Subsequently, this facilitates surgical treatment, allowing the operation to be performed while preserving the reproductive organ.
The third group is antiprogestogens. For example, Mifepristone. The use of this drug in myomatous processes provokes short-term regression of the tumor and relieves pain symptoms. Antiprogestogen therapy is used only before surgery.
The next group is hormonal drugs containing estrogens and gestagens. Basically, these drugs are prescribed to women for fibroids. Treatment stops the growth of tumors and helps them shrink. But it lasts six months, sometimes several years. Prescribed:
These drugs are used for subserous and intramural myomatous formations, which are most amenable to the therapeutic effects of drugs.
Surgical treatment is indicated when the size of the fibroid approaches 12 weeks of pregnancy, the tumor begins to interfere with the normal functioning of other abdominal organs, or is accompanied by endometriosis or an ovarian tumor.
Surgery is also performed if pain syndromes prevent a woman from living a full life, bleeding threatens anemia, fibroids quickly increase in size and tissue necrosis begins.
There are two types of operations for this disease:
- 1. Laparoscopy. It is carried out in cases where there are small pedunculated myomatous nodes, subserous, intramural or mixed formations no larger than 20 cm. A camera and surgical instruments are inserted into the abdominal cavity through small punctures, the growths are cleaned out and sutures are applied. The recovery period lasts about 3 days, there is no noticeable seam, and no adhesions form in the pelvis after the operation. Contraindications to this type of surgery will be the presence of more than three leiomyoma nodes.
- 2. Hysteroscopy. It is prescribed when a woman has submucosal nodes. The procedure is performed vaginally and does not injure healthy tissues and organs, like other surgical methods. It is not performed if infectious diseases of the genital organs are diagnosed, or there are suspicions of endometrial hyperplasia and adenocarcinoma.
With proper and timely treatment, the prognosis of the disease is favorable. With constant monitoring by a gynecologist, the fibroids can be controlled, and when menopause occurs, the nodes regress on their own.
Source: https://klimakspms.net/uterus-and-appendages/hysteromyoma/mioma-matki-kod-po-mkb-10
Complications
After treatment, complications such as:
- Relapse of the disease. After removal of the formation, observation and avoidance of possible causes that led to the disease are necessary. The presence of harmful factors can lead to re-growth of the tumor. Women during menopause are especially at risk. The hormonal changes that occur during this period can again start the process of tumor growth.
- Scars on the uterus during surgical removal of multiple formations can cause uterine rupture during pregnancy. When planning a pregnancy, it is better to wait about six months after the operation. In some cases, doctors may prescribe a cesarean section to reduce the risk of this complication.
Prevention consists of maintaining a healthy lifestyle, reasonable protection from unwanted pregnancy, timely consultation with specialists in case of hormonal disorders, diseases of the female reproductive system, following all recommendations, and an annual examination.
Video: sumbucous uterine fibroids - treatment
Submucous uterine fibroids - treatment