Nodular uterine fibroids are fairly common gynecological diseases that are more common in women after the age of 30. The onset of menopause is characterized by a hormonal imbalance, which can provoke the appearance of fibroids in the uterus or the growth of fibroids that formed earlier.
With timely treatment, the woman will be able to recover completely, preserving the uterus. The advanced form of the disease is fraught with dangerous complications and consequences.
What it is
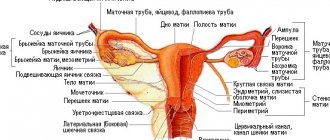
Nodular fibroids are benign neoplasms that develop in the myometrium, the muscular layer of the uterus. It is formed from fibers of muscle and connective tissues and ligaments, forming a dense, smooth knot with a rounded shape.
Myoma can be single, when only one tumor is formed, or multinodular, when several nodes develop at once. In most cases, fibroids develop in the body of the uterus, but can appear on the cervix.
Existing types
Myomatous nodes are divided into varieties according to several criteria. Depending on the location of the formation and the direction of its growth, the following forms of the disease are distinguished:
- Intramural - the tumor grows exclusively in the depths of the myometrium.
- Subserous - develops in the myometrium under the serous membrane and grows towards the abdominal cavity.
- Submucosal - appears in the myometrium under the internal mucous membrane, and its growth is directed into the uterine cavity.
Uterine fibroids of the subserous and submucous nodular form can grow either on a wide base or on a thin stalk.
The development of the disease is determined by the size of the node. Moreover, on ultrasound the size of myomatous tumors is determined in millimeters or centimeters by measuring in diameter, and in practical gynecology the size is indicated in obstetric weeks. The gynecologist compares the size of the uterus with a developed node with the size of the uterus that is normal at a certain stage of pregnancy.
The following sizes of fibroids are distinguished:
- Small or small - the node does not exceed 2 cm in diameter or 4 weeks of pregnancy.
- Medium - the size of the neoplasm in diameter is from 2 to 6 cm or up to 10-11 obstetric weeks.
- Large – the tumor is larger in diameter than 6 cm or 12 weeks.
The choice of treatment method depends on the size of the tumor.
Depending on the degree of growth of the node and the intensity of formation of new blood vessels within it, the following courses of the disease are distinguished:
- Simple - the node consists of unevenly distributed muscle and connective tissue cells. Cells have a low ability to divide and due to this the tumor grows slowly
- Proliferating - externally the formation has a clear contour, but it contains a large number of vessels and cavities. The tumor tends to grow rapidly due to the high rate of cell division.
The simpler form of myomatous nodes is more common.
Causes
Doctors identify two main theories for the development of uterine fibroids, as well as a number of factors that increase the risk of pathology. According to the first theory, each myomatous tumor begins to grow from a separate defective cell of the uterus, which is formed during the prenatal development of a girl, under the influence of various factors.
With the arrival of the first menstruation, changes in hormonal levels provoke the division of defective uterine cells and the growth of myomatous nodes.
According to the second theory, the cell from which the tumor begins to grow appears in the absence of pregnancies. Normally, the smooth muscle cells of the uterus begin to divide in the second half of the menstrual cycle, preparing the organ for pregnancy.
If conception does not occur, the newly formed cells die and are excreted from the uterus with menstrual blood. In some cases, some cells may not die. They will continue to divide in subsequent cycles. Some of them die, while others begin to grow a nodule, and thus fibroids develop.
During pregnancy and lactation, the uterus does not menstruate and has the opportunity to rest. The fewer pregnancies a woman had, and the shorter the lactation period, the less rest the uterus had.
In the absence of pregnancies, the uterus did not have the opportunity to rest. Monthly menstruation depletes it, and increases the likelihood of developing nodular type uterine fibroids.
The appearance of myomatous nodes can be provoked by the following factors:
- Hormonal imbalance, regardless of the cause. Frequent stress can lead to it.
- Inflammatory and infectious diseases of the genital organs.
- Injuries to the uterus received during difficult childbirth, gynecological curettage and abortion.
- Operations performed on the uterus.
- The development of endometriosis is a disease in which the cells of the inner layer of the uterus grow outside their layer.
- Excess weight leads to estrogen dominance. After all, adipose tissue tends to deposit estrogen.
- Pathologies in the functioning of the endocrine system organs lead to hormonal imbalance.
- Irregular sex life or its complete absence, as well as the constant lack of orgasm, lead to stagnation of blood in the pelvic organs.
- Sedentary lifestyle.
An important place among the factors provoking the disease is occupied by genetic predisposition. Approximately 60% of women diagnosed with uterine fibroids had the same disease in their mother, sister, grandmother, or other close relative.
Sonographic picture
Echosigns of uterine fibroids and the structure of a benign neoplasm are largely determined by what tissue it consists of and where it is localized. Fibroids are usually hyperechoic, and leiomyomas, due to the predominance of low-grade smooth muscle fibers, give a more homogeneous picture.
The node, located in the thickness of the wall of the reproductive organ, most often does not deform the contour of the cavity and wall of the organ. The size of the nodes can reach 15-70 mm.
A submucosal node can be diagnosed as an iso- or hypoechoic oval-shaped object against the background of the endometrium or fluid in the cavity of the reproductive organ.
The subserous node creates a tuberous contour of the genital organ, and can change its localization relative to the median axis of the small pelvis. Often, such a myomatous node is quite problematic to measure, so they resort to Doppler. With its help, it is possible to examine all the vessels and accurately determine the size of the tumor.
Fibroids have certain signs that can be observed during ultrasound examination. The benign neoplasm has a round shape with a heterogeneous structure, and the edges of the fibroids are quite uneven.
In addition, experts identify the following echo signs that may indicate the presence of fibroids in the uterine cavity:
- the size of the reproductive organ is larger than normal;
- the outlines of the organ are deformed;
- heterogeneous organ density;
Doppler shows unusual blood flows. Determining the size of the reproductive organ with myomatous nodes is carried out in the usual way, if only one formation is visualized. In the event that a multiple process is observed in the cavity of the reproductive organ, then a description is made taking into account the largest node.
What is the danger of the disease
For women of reproductive age, the development of myomatous nodes is dangerous due to the development of infertility. Depending on the location of the tumor, a woman will not be able to get pregnant or carry a child to term - there will be miscarriages.
Nodular uterine fibroids provoke various disorders of the menstrual cycle, an increase in the number of critical days and the abundance of menstrual flow, which leads to the development of iron deficiency anemia.
With a certain localization of the nodes, hematometra can develop - menstrual flow does not flow out, but remains in the uterus. When the uterus is filled with menstrual blood, urgent surgery is required.
Myomatous nodes can become inflamed, which leads to the development of peritonitis or sepsis. Torsion of the leg of the node leads to necrosis of myomatous cells, and in case of untimely medical care, to the development of peritonitis.
Submucous, internal and subserous fibroids.
If the myomatous node grows towards the bladder, then a frequent urge to go to the toilet begins, and then problems with urination. When a fibroid nodule grows towards the rectum, problems with defecation begin, frequent constipation appears and, as a result, hemorrhoids may develop. Myomatous nodes can degenerate into a malignant tumor.
To avoid the dangerous and irreversible consequences of the development of myomatous nodes, it is necessary to regularly undergo a preventive examination by a gynecologist every six months and promptly treat gynecological diseases, adhering to all the doctor’s recommendations.
Reasons for the appearance of the tumor
The main cause of fibroids is considered to be a hormonal imbalance in the body. This neoplasm is estrogen-dependent, that is, its development and occurrence are caused by an excess of estrogen in the body.
The causes of hormonal imbalance can be endocrine pathologies, taking hormonal drugs to eliminate cycle disorders that appear during menopause, as well as infertility treatment. Contraceptive drugs with a high amount of estrogen, which activates ovulation, also provoke the development of fibroids.
Hormonal imbalance also occurs in infectious and inflammatory diseases of the genital organs. The presence of polyps, ovarian cysts, and endometriosis also leads to an imbalance in the synthesis of sex hormones.
Other factors that contribute to the development of a nodular tumor are:
- injuries to the uterus that were received during gynecological medical procedures, during abortion or childbirth;
- heredity;
- depression;
- sedentary lifestyle.
Symptoms: how to recognize pathology
At the initial stage of development, nodular fibroids develop asymptomatically, and therefore can only be detected during a gynecological examination. As the tumor grows in size, the following symptoms may appear:
- The number of critical days increases, and menstrual flow becomes heavier than before.
- Painful sensations appear before and during menstruation. More often, women complain of pain in the lower abdomen, but it can radiate to the lumbar region.
- Bloody discharge during the menstrual cycle.
- Iron deficiency anemia begins to develop due to monthly heavy menstrual flow. She has the following symptoms: general weakness of the body, frequent headaches and dizziness, poor skin, and fatigue.
- There may be discomfort and pain during sexual intercourse.
Large fibroids begin to put pressure on the bladder or intestines in the rectal area, which leads to various pathologies in these organs - problems with urination and defecation. A woman’s belly begins to grow, but her body weight may not change significantly.
Submucosal fibroid
Submucosal fibroids are also called submucosal fibroids due to the fact that they appear under the inner mucous membrane of the uterus and grow towards the uterine cavity. Nodes of this type can grow either on a stalk or on a broad base. Submucosal nodes more often develop in the body of the uterus than on the cervix. This type of fibroids has the highest growth rate.
A distinctive symptom of submucosal nodes is heavy menstruation with clots, which may be accompanied by cramping pain. The duration of critical days increases to a week or more, with daily blood loss exceeding 100 ml.
Another symptom of this type of nodes is bloody discharge during the cycle. Due to the direction of growth of nodes into the uterine cavity, a woman cannot become pregnant or has miscarriages.
First aid for the birth of a node
The birth of a node is a complication that occurs only with the development of submucous fibroids on a thin stalk. The mobile node is expelled from the uterine cavity through the cervical canal into the vagina.
When fibroids are born, the following symptoms appear:
- cramping pain in the lower abdomen;
- intense bleeding begins;
- there is a feeling of heaviness and distension of the vagina;
- cold sweat appears;
- heart rate increases;
- blood pressure drops;
- the skin turns pale;
- possible dizziness;
- General weakness of the body appears, which has an increasing tendency.
If the birth of a node has already begun, then only surgical treatment is indicated. With heavy bleeding, there is a high risk of infections and the development of life-threatening complications. Therefore, the woman needs to be operated on as quickly as possible. It is important to call an ambulance immediately, and the woman needs to lie down until she arrives.
At the stage of preoperative preparation, the woman is given infusion therapy to compensate for blood loss, and antibiotics and other medications are administered to stabilize her condition.
During the operation, the submucosal node is removed, sometimes along with the uterus and appendages. After surgery, antibiotic therapy is administered to avoid the development of infectious complications.
Subserous node
Subserous or abdominal myomatous nodes form on the outside of the myometrium under the serous layer of the uterus and grow towards the abdominal cavity. They can grow on a wide base or a thin stalk. In the second case, the tumor will protrude beyond the uterus. While fibroids are small in size, they develop asymptomatically.
Symptoms begin to appear when the nodes grow to medium to large sizes. Pedicled nodes are not characterized by menstrual irregularities.
If the tumor grows on a broad base, then as its size increases, the contractile activity of the myometrium may be disrupted, which is manifested by long and heavy menstruation. In this case, the woman develops iron deficiency anemia.
If the nodes have grown to a large size, then lower back pain appears, which intensifies during menstruation. There are also signs of pressure on neighboring internal organs.
When the node puts pressure on the bladder, the urge to urinate becomes more frequent, and there is a feeling of incomplete emptying of the bladder. Compression of the rectum is indicated by frequent constipation, increased urge to defecate, and the appearance of hemorrhoids.
Abdominal nodes have less impact on reproductive function than other types of fibroids. A woman will not be able to get pregnant only if the growth of a subserous node on a wide base has led to significant deformation of the uterine cavity or the formation of its bend.
Intermuscular transmural nodes
Intramural myomatous nodes are also called transmural or intermuscular. They grow exclusively in the myometrium - the muscular layer of the uterus. Often, not one node develops, but several at once, with different localization in the uterus and growth rate. At the initial stage, the disease develops asymptomatically. When the node enlarges, the following symptoms appear:
- Uncomfortable and painful sensations in the lower abdomen;
- Heavy periods, which may contain clots.
- Bleeding appears after menstruation.
Against the background of intense bleeding, iron deficiency anemia develops.
With the growth of multiple nodes, the uterus increases in size and puts pressure on neighboring organs, causing problems with urination and defecation, and nerve endings are also pinched.
If a woman has a single small intermuscular fibroid, she will be able to become pregnant and carry a child, provided that the fertilized egg does not attach next to the node. Enlarged nodes deform the uterine cavity, and problems with pregnancy arise.
Tumor size for surgery
Surgical removal of myomatous nodes is indicated in the following cases:
- large tumor - more than 6 cm in diameter or 12 obstetric weeks.
- the node grows rapidly - more than 4 weeks of pregnancy in 1 year.
In some cases, the size of the node is not a decisive factor when deciding to treat it surgically. The operation is indicated in the following cases:
- a nodule has formed on the cervix or submucous fibroids have grown in its body;
- a woman has long and heavy periods, which led to the development of anemia;
- the growth of the node is accompanied by severe pain that is not relieved by painkillers;
- The uterus with overgrown tumors puts pressure on nearby internal organs, which leads to disruption of their functionality.
A woman undergoes urgent surgery if there is torsion of the leg of the node or, due to malnutrition of the tumor, necrosis of its tissues begins.
Types of fibroids, reasons for their appearance
There are several types of fibroids. The submucosa appears inside the uterine cavity, under its lining. It causes severe pain and cramps. Subserosal fibroids develop on the outer lining of the uterus. Interstitial forms on the walls of the uterus and quickly increases in size. Interligamentous fibroids are localized in the environment of the ligaments that support the uterus in the abdominal cavity. The stalked form develops from the subserosal form when it grows a stalk. Such formations can twist and cause severe pain. Making a diagnosis when the uterus is enlarged in size does not cause difficulties during a routine gynecological examination. In order to clarify the number and location of nodes, additional studies are used: ultrasound, hysteroscopy, laparoscopy.
Factors contributing to the development of fibroids include progesterone deficiency, increased levels of estrogen hormones, disturbances in the processes of synthesis and transformation of sex hormones, and changes in the sensitivity of the myometrium (uterine body) to them. The hereditary factor also plays a certain role. The cause of the development of fibroids can be a previous abortion or chronic inflammatory diseases of the genital organs. The likelihood of developing this disease increases in women who postpone pregnancy until later in life.
Sources:
https://vekzhivu.com/article/2230-uzlovaya-fibromioma-matki-chto-nuzhno-znat-zhenshchinam https://krasotka.guru/zabolevaniya/uzlovaya-mioma-matki https://www.kakprosto.ru/ kak-898973-uzlovaya-fibromioma-matki-priznaki-i-simptomy-
Diagnostic measures
Fibroids are detected during a standard gynecological examination with speculum.
As the disease develops, the uterus becomes enlarged and hardened. To confirm the initial diagnosis and determine the form of the disease, as well as the exact location of the nodes and their size, the gynecologist prescribes the woman a series of instrumental studies and tests:
- Ultrasound of the pelvic organs is performed in two ways: abdominal, which is also called external, and transvaginal - a special sensor is inserted into the vagina. Transvaginal ultrasound allows you to accurately determine the structure of the tumor, its size and location.
- A complete blood count can detect anemia.
- A smear for flora and atypical cells allows you to exclude malignant neoplasms of the cervix and associated infectious pathologies.
- Hysteroscopy - a gynecologist examines the uterine cavity using a hysteroscope - a special device equipped with a camera. The study allows you to determine the shape of the node, its size and exact location, as well as take a photograph in order to be able to observe it during drug treatment. If a malignant nature of the formation is suspected, during the examination the doctor takes tissue fragments for analysis in the laboratory.
- Computed tomography (CT) and magnetic resonance imaging (MRI) of the pelvic organs. Both tests are performed using X-rays that are sensitive to soft tissue. During the study, layer-by-layer images are taken. Using a special computer program, the taken frames are combined and a three-dimensional image of the organs is obtained. During the study, it is possible to determine the exact number of nodes, their size and location, as well as the direction of growth.
Ultrasound and hysteroscopy are considered the gold standard in diagnosing uterine fibroids. CT and MRI are diagnostic diagnostic methods, but due to their high cost they are not often prescribed.
Survey
As a rule, diagnosing nodular fibroids is not associated with any difficulties, and therefore does not cause any difficulties. Usually, fibroids are detected already in the gynecological chair, but additional examination is required to accurately determine its shape, size and specific location.
Before taking any decoctions, you should definitely consult your doctor.
When examined by a gynecologist, the doctor palpates the uterus and detects nodes, determines their number, parameters and location. An ultrasound examination gives more specific results. Ultrasound is performed in different ways: transvaginally or abdominally. When examined through the vagina, the picture of the disease is more informative.
The list of prescribed procedures includes MRI and ultrasound diagnostics, Dopplerography and hydrosonography, hysteroscopy and laparoscopy. If nodes of a 12-16 week tumor are detected, its removal is prescribed. And 10-11-week formations require conservative treatment. Sometimes difficulties arise in identifying fibroids and identifying them with an ovarian tumor. But carrying out a diagnostic laparoscopic procedure, during which the uterine cavity is examined from the outside, makes it possible to accurately determine the location and nature of the tumor process.
Treatment of nodular fibroids
Even 20 years ago, the nodular form of fibroids was considered a precancerous condition and the tumors were removed along with the uterus, depriving women of the opportunity to give birth to children.
Numerous studies have shown that the probability of degeneration of benign nodes into malignant tumors is no more than 3%. Therefore, priority is given to organ-preserving treatment methods, and hysterectomy is resorted to only if the patient’s life is threatened.
When a woman is diagnosed with a nodular form of uterine fibroids, treatment can be carried out in the following ways:
- medicinal;
- operational;
- carry out embolization of the uterine arteries;
- perform the FUS ablation procedure.
The decision on how to treat nodular fibroids is made by the attending physician, taking into account the patient’s age and her desire to have a child.
Conservative treatment
If a woman is diagnosed with small nodular uterine fibroids, she is prescribed hormonal and concomitant therapy.
Hormonal therapy includes taking the following groups of drugs:
- Antagonists of gonadotropic hormones or GnRH for short, which slow down the synthesis of estrogen and thereby help reduce the size of myomatous nodes. The following drugs are popular: Buserelin, Goserelin and Leuprorelin.
- Androgen derivatives reduce the amount of female sex hormones by increasing male ones. Omnadren 250 is often prescribed.
- Gestagens are prescribed very carefully and mainly to women of late reproductive or premenopausal age who are simultaneously diagnosed with myomatous nodes and endometriosis. Previously, it was believed that only estrogens affected the growth of fibroids, but studies conducted in recent years have confirmed the influence of progesterone.
- Combined hormonal oral contraceptives normalize hormonal levels and stop the growth of nodes, as well as promote their regression. Often prescribed: Ethinyl estradiol, Norgestrel and Desogestrel.
- Antigonadotropins inhibit the pituitary gland's production of follicle-stimulating and luteinizing hormones, which stimulate the ovaries to synthesize sex hormones: estrogen and progesterone. They cause a number of side effects and therefore are prescribed only if there is no effect from taking other medications. Popular drugs: Gestrinone and Danazol.
The drugs, dosage and duration of use are prescribed exclusively by the doctor, based on the results of blood tests for hormones and instrumental studies, as well as taking into account the presence of concomitant diseases.
For intense periods, concomitant therapy is prescribed, including taking the following vitamins, microelements and acids:
- vitamin complexes, including B vitamins, especially vitamin B9 or folic acid, which have a beneficial effect on the functioning of the hematopoietic system;
- preparations containing iron;
- tranexamic acid, which prevents the destruction of platelets and, as a result, reduces blood loss.
Vitamin complexes should be prescribed by a doctor, based on the results of general and biochemical blood tests.
Surgery
When surgically treating nodular uteruses, we try, if possible, to preserve the uterus or at least its cervix. Surgical removal of only the nodes is called myomectomy, and removal of tumors along with the uterus is called hysterectomy.
There are different ways to carry out operations, which we will discuss further. Recently, they are increasingly resorting to methods of minimally invasive intervention: uterine artery embolization and FUS ablation.
Uterine artery embolization
Uterine artery embolization, or EMA for short, is a gentle method of treating fibroids. A woman is punctured in the femoral artery and emboli - very small synthetic balls - are inserted into the uterine arteries through a special catheter. They, along with the blood, enter the terminal vessels, which feed the nodes and block them.
Since the supply of nutrients is stopped, the fibroid cells die. The nodes gradually decrease in size and over time either resolve or become covered with a capsule of connective tissue. They look like small nodes, but their structure is not fibroids, and they do not interfere with pregnancy and childbirth.
EMA does not affect uterine cells because their blood circulation is different from that of tumors. The procedure is carried out under the control of a special X-ray complex, generating ultra-low doses of radiation. A contrast agent is injected into the arteries through the catheter tube, allowing the vessels to be visualized under X-ray light.
The UAE procedure is not performed in the following cases:
- subserous nodes on a thin stalk have developed;
- large intramural-subserous fibroids - the size in diameter exceeds 8 cm;
- giant fibroids – more than 20 weeks of pregnancy;
- there is a suspicion that the node is malignant;
- inflammatory or infectious diseases of the pelvic organs have been diagnosed.
In the described cases, doctors choose other methods of treating fibroids.
FUS ablation of nodular fibroids
The procedure for exposing the myomatous node to focused ultrasound waves is called FUS ablation. It is carried out under the control of a magnetic resonance imaging scanner. During the procedure, ultrasonic waves affect the cells of the node.
They heat up and begin to necrotize - die. FUS ablation is prescribed to women who do not plan to have children in the future. Because the procedure has a number of complications due to the fact that the rays affect not only the tumor, but the uterine tissue and nearby organs.
Myomectomy and hysterectomy
During a myectomy, the surgeon removes only the nodes and preserves the uterus.
It is carried out in the following ways:
- Laparotomy - open abdominal surgery is indicated for large myomatous nodes, multinodular fibroids and suspected malignant tumor.
- Laparoscopy is a minimally invasive operation in which several punctures are made in the lower abdomen to insert a special instrument and a laparoscope - a device equipped with a video camera. The nodes are excised and removed.
- Mechanical myectomy involves surgical intervention with a special instrument inserted together with a hysteroscope into the uterine cavity through the vagina and cervical canal. The hysteroscope is equipped with a video camera and lighting. The operation is prescribed for submucous fibroids on a pedicle and on a wide base, grown into the myometrium by no more than 50%.
They try to resort to hysterectomy, which involves removing the nodes along with the uterus, only when there is a threat to the patient’s life.
Prevention
Experts have developed preventive measures to prevent the development of fibroids:
- undergo a preventive examination by a gynecologist every six months, and if problems arise, immediately consult a doctor;
- promptly treat all inflammatory and infectious diseases of the reproductive system;
- plan to have children before the age of 40;
- stop smoking and minimize alcohol consumption;
- eat a balanced diet and do not adhere to strict diets;
- regularly engage in sports and other physical activities, but with moderate exertion;
- have a regular sex life, taking care of contraception and so as not to resort to abortion;
- control your weight.
By leading a healthy lifestyle and being attentive to the physical condition of her body, and the reproductive system in particular, a woman can minimize the risk of developing fibroids, even if she has a genetic predisposition to the disease.
Risk factors
There are conditions that contribute to the formation of fibroids in a woman’s body. The main and most common ones include:
- irregular menstruation;
- first menstruation after 15 years;
- significant amounts of bloody discharge lasting five days or more;
- childbirth at a late age;
- termination of pregnancy, miscarriages;
- chronic inflammatory processes, infections in the genital organs;
- endometriosis, polyps, polycystic disease;
- diseases of the endocrine system;
- diabetes;
- lack of physical activity;
- constant stressful conditions;
- smoking, drug use, alcoholism;
- overweight, obesity.
Possible consequences
The consequences of fibroids occur when a woman has advanced the disease, and the node has grown to such a size that conservative treatment is no longer prescribed, and based on the results of the diagnosis, removal of the tumor along with the uterus is indicated.
After removal of the uterus, the patient faces the following conditions and complications:
- infertility;
- decreased libido;
- pain during sexual intercourse;
- weight gain;
- depressive states;
- the appearance of rapid fatigue;
- memory impairment;
- increasing the likelihood of prolapse of the vaginal walls.
After a hysterectomy, a woman will not necessarily have all of the listed complications, some of them will be vague, and some will not exist at all.
Compatibility with pregnancy
With nodular fibroids, a woman can become pregnant. During pregnancy, nodes are not treated, but only monitored. The most dangerous condition is when the myomatous formation begins to grow. In this case, there is a threat of miscarriage due to impaired circulation in the uterus and increased contractions.
The nodes interfere with the normal position of the fetus, which complicates childbirth. Therefore, women with uterine fibroids are often prescribed a cesarean section.
To avoid problems with bearing and giving birth to a baby, it is advisable to undergo a full medical examination at the pregnancy planning stage. When fibroids are detected, doctors recommend first curing it and then having offspring.
Prerequisites for the development of the disease
The reasons leading to the appearance of nodular uterine fibroids are varied and are not fully understood in our time. Most scientists and practicing doctors support the hormonal theory of gynecological pathology. This is confirmed by the following factors:
- Receptors for sex hormones are found on the surface of benign tumor cells.
- The peak development of the neoplasm occurs during the reproductive period and is characterized by an increased level of estrogen in the body.
- The pathology can regress on its own during menopause with a decrease in estrogen levels in the blood.
- With hormonal therapy with estrogen preparations, intensive growth of myomatous nodes is observed.
Hereditary predisposition plays a significant role in the occurrence of the disease. According to statistics, in 60% of cases, in addition to the patient herself, her closest relatives - mothers, sisters - suffer from this pathology.
Folk recipes
If nodular fibroids are detected, folk recipes can only be used as an auxiliary treatment. Before you start taking any folk remedy, you should consult your doctor. Myomatous nodes are hormone-dependent and therefore, taking products that include plants with phytoestrogens can provoke their growth.
If the doctor does not object, then you can take freshly squeezed potato juice, which has an immunostimulating and anti-inflammatory effect. The juice is taken once a day - in the morning on an empty stomach in the amount of 100 ml. You can eat after 30-40 minutes. The standard duration of juice therapy is 3 months, and the minimum is 1 month.
To get the maximum effect from treatment, you need to choose the right raw materials. Potatoes should only be taken with pink skin. Squeeze the juice from unpeeled tubers, which are only thoroughly washed. Potatoes that have been stored for no more than 3 months after harvest are suitable for treatment.