girls, this is the situation. The first birth took place with cervical ruptures. No stitches were needed, it healed on its own. scar deformation remained. Conization was prescribed. While I was breastfeeding, while I was being examined, while I was treating all sorts of colpitis, I became pregnant again. There were no ruptures during childbirth, but the scar deformation had nowhere to go. So I still have to undergo conization, but we’ll wait until I stop feeding. I would like to determine the opinions of those who have encountered this or the procedure. How it all happens. My gynecologist only said that he came and went, there is no need to go to the clinic. but there was no time to ask in detail. Is some kind of anesthesia given? Does it hurt later after the procedure? Are there any complications? Do ABs inject, as during surgical interventions? I would be grateful for any information.
I had a cone made on the pretext of cervical dysplasia. Indeed: he came and went. On a chair, under general anesthesia, the procedure itself lasted perhaps 10-15 minutes, after which I lay on the couch for 1 hour. At the time when the anesthesia had completely worn off, I came to the doctor’s office (who was performing the operation), she pulled a tampon out of me on the chair (it is placed at the end of the cone), looked at how everything looked there and sent me home. It goes without saying that you won’t get there on your own (it’s a bad situation), I went by taxi. You need to stay at home until evening. Nothing hurts there, I think my lower abdomen hurt until the evening. I bought painkillers in advance; I didn’t need them. I spent the first week going to the doctor to have the wound treated. For the first month, don’t lift anything heavy. Look like that's it.
Since I created a topic, I’ll post in it now. I did conization. I would like to share information, in case someone needs it.
What needs to be done before conization?
It is necessary to undergo a gynecological smear for flora, cytology and analysis for HPV (human papillomavirus). If any infection is found, treat it. It is also necessary to think in advance who will help after the conization is completed, since there are later restrictions, which I will write about later.
When exactly and why?
Conization is done immediately after the end of menstruation - on the 2-3rd dry day. Firstly, it is now most possible that the lady is not pregnant. Secondly, there is enough time left for the cervix to heal before the next menstruation.
How is conization carried out?
It is carried out on a simple gynecological chair in a position familiar to us ladies. An iron plate is placed under the butt (as I realized, it is an electrode, or something like it). An anesthetic injection is given in the neck. The sensations are slightly unpleasant, but completely tolerable. There is no such pain, but while the doctor is cutting out the tissue, there is a ache in the lower abdomen, like during menstruation. The doctor immediately cauterizes the opened vessels. Scabs form in these places (or scabs - I don’t know which is correct). At the end of the procedure, the doctor treats the cervix with an antiseptic and places a medical tampon, which will need to be removed after a couple of hours.
What's at the end?
Since all the vessels are cauterized, there is no bleeding immediately after conization. The belly ached for several more hours. It is possible to take a painkiller. Immediately after conization, copious watery discharge begins. On the 7-10th day, the scab begins to come off, and the discharge becomes bloody, but not profuse (to put it simply, a spot). Such discharge lasts until the period itself. At the end of menstruation, the cervix should have healed sufficiently so as not to bleed a lot.
Medications
Initially, the doctor prescribed only suppositories. From the next day after the end of conization Gravagin 10 days, then immediately Betadine until menstruation. But since I know that I am prone to bleeding, I asked to be prescribed something additional to reduce the risk. I took Dicinon in pills for 5 days and drank Ascorutin in a minimal dose. If painkillers were needed, I drank Tamipul.
What specific restrictions?
It is strictly forbidden to: - lift weights (the doctor told me no more than 2 kg) - soar your feet / steam / take a bath / go to the sauna - drink alcohol - take vasodilators - have sexual activity - use tampons, as well as during your next menstruation.
In general, we perform sexual rest for 4 weeks, do not lift anything heavy and do not allow vasodilation. Just based on this, before conization it is necessary to find someone who will help: lift the child if necessary, bring bags from the store, etc.
What specific complications?
From what I remember, this is bleeding and may somehow affect the next pregnancy (perhaps it may not affect it - this is only a probable complication). To avoid bleeding, follow everything the doctor says.
Complete healing occurs after 3-4 months. But the restrictions are lifted when the scab comes off and there is no risk of bleeding. Then it is possible to return to simple life, and after a few months just see a doctor. The material that is excised during conization is necessarily sent for biopsy.
Z.Y. Everything outlined above concerns electroconization. This is how everything happens specifically in Kharkov, specifically in the clinic where I was. Somewhere, perhaps, something is different.
A scab is a crust that forms on the surface of a wound, regardless of its etiology. The structure of the scab consists of clots of coagulated blood, pus and necrotic tissue. The stupa is of great importance, since its presence helps protect the wound surface from infection and ensures the process of epithelization of the defect. After complete healing of the wound, it disappears on its own.
The appearance of this crust is familiar to everyone from childhood; visually, the scab after cauterization of the erosion looks almost the same as with wound skin defects. Most often, the scab goes away on its own within 14-28 days. Normally, the process of its separation is not accompanied by any discharge, including bloody discharge. Also, like the uterus, it should be absolutely painless.
Attention!
The information on the site is presented by specialists, but is for informational purposes only and cannot be used for independent treatment. Be sure to consult your doctor!
Collapse
Coagulation is the most popular and effective procedure for the treatment of cervical erosion. As a result of treatment, an unusual formation called a scab forms on the area of former erosion (on the area treated in one way or another). Later it separates on its own. What does a scab look like after cauterization of erosion on the cervix? This is discussed in this article.
Definition
It forms after any coagulation, regardless of the method used. After a new healthy epithelium forms at the cauterization site, the film comes off, and until this moment it performs a protective function, preserving new epithelial cells.
The scab may differ in appearance with one or another type of coagulation. Indeed, depending on the method, certain changes occur in the cells of the pathological epithelium. The appearance of the layer depends on their character.
The essence of the concept
A scab is a kind of film of tissue that forms exactly at the site treated during the manipulation process. It has a soft structure, so it is not felt when it comes out. The color of this formation is white, grayish, yellowish or sandy.
Depending on the parameters of the patient’s body, her regenerative abilities, the size and thickness of the accumulation of destroyed cells, it is separated from the surface 5-12 days after cauterization. Also, the difference in the time of separation of the layer is explained by the method by which the medical intervention was carried out.
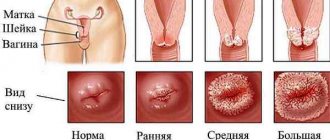
What a scab looks like can be seen in the photo below:
Cauterization process
Scab after cauterization
Healing process
Why does it appear?
A scab is a collection of dead, destroyed cells. That is, during treatment with low or high temperatures, or another method, pathological cells die and are destroyed. Most often, during the cauterization process, protein denaturation occurs in pathological epithelial cells, that is, the cell dies. It is this accumulation of dead cells that constitutes formation.
This accumulation prevents bleeding from vessels affected during medical manipulation. In addition, it prevents infections, viruses and fungi from entering directly into the bloodstream through an open wound. For this reason, such a formation is not removed at the cauterization stage, but must go away on its own.
Cauterization of cervical erosion with radio waves: advantages and disadvantages
The advantages of treating cervical erosion with radio waves are as follows:
- The entire treatment lasts a maximum of 15 minutes, and this includes time for minimal preparation and rest to avoid dizziness;
- There is complete absence of blood and pain, maximum – fear and discomfort;
- After the session, no scars, scars or other consequences of injury are formed;
- The reappearance of uterine cervix erosion is almost completely eliminated;
- The doctor can control the depth of influence of the rays, causing only pathological cells to die and eliminating possible negative consequences of the procedure in general;
- After the session, there are no injuries to healthy tissues surrounding the cervical erosion;
- The technique is suitable for both women who have given birth, as well as virgins, nulliparous patients and older women;
- After this treatment there is not a single side effect.
Of the negative aspects, the patient singles out only one - the high cost of such cauterization. Also, some note the frequency of bad consequences in the form of discharge, which can be disturbing for several weeks. Ideally, after radio waves there should be no discharge, although experts never exclude the possibility of an individual reaction of the mucous membrane even to such non-contact therapy.
How long does it take to leave?
When does this cell layer come off? It depends on many factors. If the erosion was small and shallow, then the scab will be small and thin. The epithelium underneath will recover quickly. That is, such a scab can go away after 3-5 days.
If during the coagulation process a large area and to a great depth was processed, then the film will be large. Healthy epithelium at the site of the removed pathological one will grow for quite a long time. In this case, the accumulation of dead cells may disappear 10-12 days after the manipulation.
The method of gynecological medical intervention plays a big role. Laser and radio wave methods lead to the formation of a small scab, as they work at a shallow depth. After such an intervention, the layer of destroyed cells separates from the healthy epithelial layer on average in 5-7 days. It can also be quickly eliminated by chemical coagulation. And sometimes in this case it is not formed at all.
The largest scabs are formed as a result of electrocoagulation. This is due to the fact that this outdated method works at a fairly large depth, partially cauterizing healthy tissue. As a result, a very large scab is formed.
How does it leave?
Deliberate separation of this formation is not required. When the new healthy epithelium is completely formed, the scab begins to separate. This can happen over several days or all at once. This is due to the fact that it is separated in parts or completely.
These parts or the entire film enter the vagina. From there they come out along with vaginal secretions or during showering. This happens completely painlessly. Usually, the patient does not notice at all that this has happened.
Complications
Normally, the removal of a scab is not accompanied by any complications. In extremely rare cases, such complications are possible when the scab leaves the body after cauterization of cervical erosion:
- Mild painful sensations of a localized nature (in the cervix);
- Nagging or aching pain in the lower abdomen;
- Spotting bleeding on the day of scab separation, which should stop within a few hours.
If bleeding continues, you should immediately consult a doctor.
Regardless of the method chosen, cauterization of the cervix is traumatic. After treatment, a wound is formed that is open to infection. Healing goes through certain stages, and bleeding after cauterization of erosion is inevitable. The nature of bleeding varies: it is determined by the day after surgery and the condition of the patient. Discharge formation after cauterization of cervical erosion is likely, requiring special treatment.
Why does erosion occur?
Almost every second woman has suffered cervical erosion at least once in her life. Ectopia or erosion is a superficial defect of the mucous membrane that requires medical attention. In rare cases, congenital erosion of the mucosa is possible, which disappears on its own upon completion of puberty. True erosion occurs in the form of a wound on the mucous membrane; over time, it heals on its own. In other cases, we are talking about false erosion, it does not go away spontaneously, this condition can lead to serious problems, including the development of cervical cancer.
Stages of Natural Healing
The main specificity of wound healing after cauterization is that this process takes place under the scab.
. Blood clots that quickly appear begin to clog the vessels, so bleeding is not observed. Fluid from tissues, lymph, and clotted blood create a crust on the surface of the wound that protects against the entry of pathogenic bacteria or re-injury.
All wounds go through several stages before new epithelium appears in their place:
- Inflammatory process.
- Proliferation.
- The appearance of new epithelium.
The stage of the inflammatory process is slightly expressed. Fibroblasts and leukocytes begin to flock to the site of injury, absorbing secretions after cauterization of the erosion by radio waves, which appeared during the decay. At the same time, collagen production is activated.
During the proliferation stage, the tissue under the scab increases over time, and small vessels begin to grow into it. By the end of this phase, new epithelium has formed on the thin tissue, and the scab disappears.
The proliferative stage consists of the growth of epithelial tissue. Moreover, it is decided whether there will be a scar on the wound site or whether there will be new healthy epithelium.
Contraindications
Cauterization of erosion with radio waves attracts wealthy patients with the opportunity to get rid of the disease in just one session, without seeing blood, without experiencing pain and other unpleasant sensations during the recovery process. Despite the fact that the described technique is completely drug-free, it is not allowed for everyone.
The list of contraindications includes:
- Presence of a pacemaker;
- The presence of malignant neoplasms;
- Chronic pathologies in the acute stage;
- Inflammation affecting the pelvic organs;
- Carrying a child (any period);
- Infection, etc.
Features of discharge
If you cauterize uterine erosion, then immediately after radio wave coagulation of the cervix no discharge is noted: the scab begins to firmly fix the vessels. Initially, a watery discharge may appear. They are small and light in color and may contain blood streaks. These effects of cauterization of cervical erosion can take up to 2 weeks. Over time, they change to pinkish mucous.
At a further stage, scanty brown discharge is noted. They are spreadable and thick and last no more than 6-8 days.
In certain situations, the scab begins to come off gradually, in which case, during this time, its particles appear in the form of dense clots. Often the bleeding begins to intensify 3 weeks after cauterization. This is a sign that the scab has passed, but some vessels are damaged and bleeding occurs. It should be completed within 3-4 hours.
If we consider the amount of time after cauterization of erosion and how long the discharge continues, then the norm is discharge that lasts up to 21 days, and over time it changes its color and unpleasant odor. Afterwards the usual leucorrhoea begins to subside, then menstruation begins.
Cauterization of erosion with radio waves: the essence of the technique
Cauterization of cervical erosion with radio waves is a relatively new technique. It involves the use of a device that emits radio wave rays collected in a beam. The latter is carried out along the line separating damaged and healthy tissues of the mucous membrane.
- At the site of influence of the rays, a high temperature is pumped up, heating the thin upper layer of cells and causing them to literally evaporate from the plane of erosion of the uterine cervix.
- Cauterization with radio waves is a virtually painless procedure, after which a woman can go home almost immediately. The device does not cause bleeding, at the same time it has a pronounced analgesic effect, the subsequent healing process occurs quickly and without the use of any medications, and the woman herself recovers from her experience without unnecessary difficulties and worries.
- Cauterization with radio waves literally “closes” all damaged capillaries that bleed blood. As a result, the wound heals quickly, and there are no scars left on the cervix that could prevent its opening during future childbirth. Essentially, this is a non-contact way to force the internal energy of cells to reach a peak value. It is this that is necessary for the evaporation of pathological areas of the mucous membrane of the uterine cervix.
Possible complications
If you cauterize uterine erosion, the consequences may be different. When using the latest methods - laser or radio wave treatment - they are insignificant. The main reasons why the nature of the discharge changes are as follows:
- Attachment of an infectious disease.
- Deformation of blood vessels.
- Periodically appearing erosions.
- Cyst development.
- Endometriosis of the cervix.
Cauterization of a minor defect is usually not accompanied by side effects. Significant erosions, as a rule, are subsequently accompanied by unpleasant symptoms.
Possible pathologies
You need to monitor abnormal discharge and at the same time know what it should look like. For convenience, you can use sanitary pads with a cellulose surface. The use of tampons is prohibited. It is also better not to use scented pads: fragrances are an additional source of irritation that can cause allergies or inflammation.
Medical attention is necessary when the discharge is not normal. You need to worry in the following situations.
The formation of bloody discharge within a day indicates injury to the vessel. This bleeding cannot be stopped at home, so you need to see a doctor.
If blood is released after several weeks, and its release is completed within 1-2 hours, then this is due to the discharge of the scab. When, at the same time, constant bleeding occurs and an increase in temperature is noted, this is a reason to contact a gynecologist.
Discharge may occur after the last period. In some cases, after sexual contact there is a slight smear of blood. Often this is a consequence of a complication that has appeared - a cyst. This pathology has no specific symptoms.
Side effects may appear after cryodestruction, cauterization with nitrogen and other methods. Moreover, the scab clogs the glands and does not allow the contents to escape. Over time, cystic dilations appear, bursting during sexual contact with the release of a small amount of blood.
Changing the color of the liquid output
Discharge that has a brown or pinkish tint may change color. If the discharge is green or yellow, with a liquid consistency, this is a sign of infection.
The cause of the complication is insufficient vaginal sanitation before cauterization. If phase 4 purity is diagnosed based on smears, then cervicitis or colpitis must be treated before the procedure. Why are vaginal suppositories or local medications used, taking into account certain microflora.
Certain diseases are expressed by uncharacteristic discharge. This may occur during sexually transmitted infections. For example, during the development of trichomaniasis, the discharge is liquid with a green tint.
In some cases, the appearance of bacterial vaginosis is noted, and the discharge becomes whitish or gray-white.
Odor occurrence
As long as the wound heals, the discharge will not have an unnatural odor. However, in some cases this indicates a violation of natural recovery.
The development of gardnerella may indicate signs of vaginosis. During development, this pathogenic organism releases volatile amines that smell similar to rotten fish.
A dangerous symptom is discharge with a purulent odor. These symptoms appear during the development of a purulent process. The condition will require emergency surgery. The simultaneous manifestation of purulent discharge and an unpleasant odor from the vagina is an indication for contacting a gynecologist as quickly as possible.
Other unpleasant clinical symptoms
Additionally, each of the above symptoms may be accompanied by clinical symptoms such as fever and pain.
After cauterization, minor pain may be normal for a certain time. Increased pain due to heavy discharge will require medical treatment.
Pain may be an indicator of a developed inflammatory process. If the infection penetrates the appendages or the body of the uterus, or an acute chronic process is noted, then the pain manifests itself as a pulling and dull character, and in some cases it may intensify. During infection of the appendages, pain occurs on the side where the inflammatory process occurs.
Inflammatory reaction
In some cases, women may experience severe discomfort in the lower abdomen. If the pain intensifies, this may be the first symptom of a developing inflammatory process.
An increase in temperature is also considered an unfavorable symptom, which always indicates inflammation. Antibiotics are used for treatment.
Main action steps
In order to prevent complications, it is necessary to strictly follow the doctor’s recommendations. In this case, if the nature of the bleeding changes, then a different algorithm must be followed:
You can distinguish bleeding from menstruation by the time the spotting appears. For many, the first menstruation begins after 20-30 days, at which time the discharge that was noted after cauterization ends. Menstruation itself varies in color by shade. The blood during menstruation is dark, and in some cases there are clots in it. The nature of the bleeding also changes - at first it is insignificant, in the end it decreases until bleeding appears.
Risk prevention
Proper preparation for treatment and following all doctor’s recommendations will help prevent unpleasant side effects.
Before treatment, a woman must definitely take a vaginal smear, which indicates one of 4 stages of purity, in which the first stage is a completely healthy state of the woman, and the fourth is a pronounced inflammatory process. When a woman, after examining a smear, is diagnosed with the third or fourth level of purity, then before cauterization it is necessary to treat vaginitis. Why are local medications used in the form of suppositories, for example, Terzhenan, Genezol. If there is a slight presence of coccal microflora, the gynecologist will recommend treating the vagina (for example, with Povedon-Iodine suppositories).
When a smear reveals candida spores or pseudomycelium, antifungal therapy is required. The doctor may prescribe vaginal suppositories Pimafucin or Clotrimazole.
Detected gardnerella in the smear indicates vaginal dysbiosis or the probable development of bacterial vaginosis. In this situation, treatment is carried out with Metronidazole tablets.
If the examination reveals diseases that are sexually transmitted, then the required therapy must be carried out. Ureaplasma, chlamydia, trichomonas, mycoplasma, HPV often develop simultaneously with cervical erosion and support the process of inflammation on it.
How is everything going?
Treatment of uterine cervix erosion using the described method occurs under absolutely sterile conditions. The doctor and his assistant are present during the procedure. Both specialists must wear gowns, caps and use gloved hands.
The following items should be present from the set of auxiliary devices:
- Disposable wipes;
- Single use gynecological diaper;
- Specific devices;
- Tools for inspection after completion of the entire action.
The whole procedure takes a few minutes, during which the doctor manages to cauterize the pathological tissue. Afterwards, the woman is asked to lie down for a while, as there is a high risk of dizziness.
Cauterization with radio waves is prescribed taking into account when a woman’s period started/ended. As a rule, the session falls on the first stage of the cycle. The procedure itself is positioned as completely painless, although everything depends on the natural pain threshold. It happens that unpleasant sensations appear at the moment of cauterization, immediately after it, and even several hours later.
Treatment and prevention of the disease
In order to prevent the occurrence of side effects, a comprehensive preliminary examination of the vaginal microflora is required to identify and determine bacteria.
After all manipulations, it is necessary to monitor the condition of the discharge for 3-5 days. Directly during healing it is prohibited:
- Steam in a sauna and steam bath, use a hot bath.
- Sexual contact is prohibited.
- You can't sunbathe.
- Public swimming pools and natural bodies of water are prohibited.
- You can't use tampons.
- Exercise.
- Carry weights.
To speed up recovery, the gynecologist may prohibit certain medications. These are Genfiron, Depanol, Betodin suppositories. Patients in whom erosion has developed due to a viral etiology can be prescribed Kolpocid - this drug has an antiviral effect. Terzhenan tablets and Levomekolev ointment have antibacterial properties.
Effective treatment of any disease will depend on the coordination of all actions of the treating gynecologist and the woman’s compliance with the recommendations. If the patient listens to the doctor’s instructions, carries them out in a timely manner, and the doctor takes into account the woman’s individual characteristics, then the effect of treatment will certainly be only positive.
Content
When performing conization, part of the cervix is excised in a cone shape. At the site of the damaged area that is removed, a wound surface remains. Gradually, it begins to heal and become covered with a scab, which eventually separates, in the place of which normal epithelial tissue is restored. The postoperative recovery process varies differently for women. It depends on the type of operation and the body’s reaction to the intervention.
Types and reasons
In order to determine whether cauterization is necessary, erosion should be classified as a specific option. Experts classify the following types of erosion.
Congenital
It is often detected in young girls. Its appearance is associated with the maturation of the cervical epithelium. Previously, congenital erosion was considered a pathology. However, as a result of research, scientists have found that during intrauterine development, the vaginal part of the cervix is covered not with flat multilayered epithelium, but with cylindrical single-layer epithelium. Over time, the cells of the cervical canal are replaced by multilayered tissue. As puberty progresses, the defect decreases and regresses. However, in some girls this process occurs with some delay, which is associated with estrogen deficiency. In this case, the spot is detected in girls after the onset of sexual activity and is called congenital erosion.
True
Occurs if the integrity of the tissue is compromised. Thus, local destruction of the mucosa can be noted. As a result, a wound is formed, which is also accompanied by inflammation. The appearance of true erosion is influenced by various damaging factors. True erosion is rarely diagnosed, as it lasts no more than two weeks. Then the wound heals. Gynecologists note that infections prevent the normal restoration of the integrity of the epithelium. In most cases, erosion does not heal properly.
Pseudo-erosion
This means that due to destruction, subsequent restoration of the tissue did not occur correctly. Epithelization in this case occurs not due to flat cells, but due to cylindrical elements that normally line the surface of the cervical canal. Pseudo-erosion has a risk of the formation turning into cancer. That is why mandatory treatment is recommended for this form, which involves cauterization. Moreover, pseudo-erosion should be differentiated from precancerous and malignant processes that have the same visual signs.
Thus, taking into account the factors that lead to the appearance of different types of erosion, scientists identify the following causes of the defect:
- hormonal fluctuations during pregnancy, puberty, menopause;
- intrauterine developmental anomalies;
- hereditary predisposition;
- trauma to the cervical epithelium;
- rare or rough sexual intercourse;
- infections and inflammatory processes.
Before cauterization of erosion, it is necessary to eliminate, if possible, the factors that provoke the condition of the cervix. This is necessary in order to avoid relapses after cauterization.
Wound healing
Always after conization of the cervix, a scab forms. This is the name given to the crust that covers the wound surface.
To understand how the scab comes off after conization of the cervix, you need to understand how and why it forms. When treated with a laser, radio waves or electric loops, proteins are denatured. The cells are destroyed. A scab is a collection of dead cells.
But the process of formation of a scab on the neck has its own characteristics. In the moist environment of the vagina, a soft scab forms on the cervix. It can be grayish, yellow or sandy in color. Due to its soft consistency, the scab comes off almost unnoticeably in most patients.
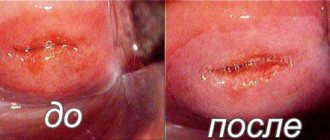
This cell layer is necessary to prevent bleeding. It prevents various pathogenic microorganisms from entering the blood through the wound. A new epithelium forms under the scab in a short period of time. But you can see how the cervix is healing only during a gynecological examination.
Usually after 5-7 days the accumulated dead cells begin to be rejected. But if a significant area of the patient’s cervix has been excised, the removal of the scab may be delayed: for some, this begins on the 10th day.
The method by which conization was performed is also important. When laser or radio wave removal of the problem area, a small scab is formed. Typically, dead cells begin to separate on the 5th day. With electroconization, a larger scab is formed. It leaves a little later: on the 7-8th day.
There is no need to perform any special medical procedures to separate the dead layer of cells. As soon as new epithelium forms under the scab, the crusts will begin to come off on their own. At the moment the scab leaves, women notice a second wave of bloody discharge.
Features of the operation
Regardless of the type of operation chosen, a wound surface is formed on the cervix. During the process of conization, the top layer is destroyed under the influence of laser, electricity or radio waves. In place of the damaged cells, a scab forms, which comes off over time.
- In most clinics, women are offered conization with a special electric loop. This method is considered optimal in terms of price-quality ratio. The cost of loop conization is low. In this case, the tissue of the cervix is minimally damaged.
During the operation, the problem area is cut out in the shape of a cone. Damaged vessels are coagulated immediately after the operation is completed. The excised area remains intact during the operation, so it can be sent for histological examination. An eschar forms in most women after conization with electric loops. But not everyone notices how he moves away.
- Laser surgery is more expensive. Using a laser, you can cut out the damaged part of the cervical canal and cervix as accurately and accurately as possible. The undeniable advantage of such an operation is the fact that during its implementation the doctor can change the intensity and depth of laser exposure. This means that during the process of conization, the surgeon can change the size of the excised area depending on the picture that opens.
- Radio wave conization is considered a highly effective method that allows you to get rid of a number of cervical pathologies. A scab after such an operation is formed in the same way as after conization with electric loops. During the process of radioconization, the area with pathologically altered tissues is cut out, and the vessels are immediately coagulated. The likelihood of complications or infection is minimal.
- Excision of the pathological area on the cervix with a surgical scalpel is currently practically not performed. When performed, complications often develop, since the method is quite traumatic. With the knife method, part of the cervix was cut out with a regular scalpel; healing took a long time and was accompanied by complications in many patients.
The likelihood of negative consequences when performing modern operations is minimized. But sometimes complications arise.
The danger of erosion for women's health
Considering the fact that the erosive process can be cured in several ways, the number of women who do not want to take care of themselves and use modern medical technologies continues to surprise. In the meantime, there are procedures that allow you to get rid of erosion of the uterine cervix in almost one visit to the doctor.
The patient has the opportunity to choose therapy that takes into account existing contraindications, pain threshold and even the financial side of the issue.
The main thing is not to miss the primary symptoms of the disease, which look like this:
- Copious vaginal discharge that changes color from whitish to greenish, yellow or clear. They may contain blood and even pus;
- Pain in the lumbar region;
- Painful sensations during intercourse and at the end of it;
- The presence of genital warts on the mucous membranes of the external genitalia.
Postoperative period
Women who are faced with the need to undergo conization of the cervix are worried. They are interested in how the operation itself is performed and how the postoperative period goes. Doctors warn that you should not rely on the experience of other women. The sensations will depend on the following factors:
- pain threshold;
- cervical conditions;
- size of the remote area;
- individual reaction to anesthesia;
- features of the operation;
- the amount of scab formed and the intensity of its discharge.
Patients who underwent conventional knife conization often complained of intense bleeding and severe pain after surgery. The removal of the scab was often accompanied by bleeding.
After the knife method, an inelastic scar may remain on the cervix. It does not bother a woman, but can cause problems during pregnancy and childbirth. Sometimes scars remain after electroloop conization. And laser and radio wave procedures, as a rule, do not leave traces.
For many, healing occurs in 4-6 weeks. But in some cases, the process lasts up to 4 months - the duration depends on the individual ability of the body to regenerate tissue.
If there were no problems during conization, and the woman adheres to the doctor’s recommendations, then the likelihood of complications occurring is minimal. Many patients do not even have blood in the first month, they only have copious watery discharge. Blood or spotting may appear only when the scab is removed.
In the postoperative period, women face the following problems:
- bleeding within 2-3 weeks after surgery;
- pain in the lower abdomen, similar in intensity to pain during menstruation;
- an increase in the volume of bloody discharge when the scab passes;
- unpleasant vaginal discharge.
Pain and increased volume of discharge may indicate damage to the tissue of the cervix and the onset of bleeding. An unpleasant odor appears when the damaged area is affected by pathogenic microorganisms.
Within a week after surgery, most patients begin to lose the scab. This may significantly increase the volume of discharge. For many, they become not only more abundant, but also darker.
In rare cases, bleeding may occur if the scab begins to come off. In such a situation, immediate hospitalization of the patient is required.
Some women who have undergone such an operation do not even know when the scab comes off after conization of the cervix. The formation and rejection of the crust in some patients is completely asymptomatic. They do not feel pain and do not notice an increase in the volume of discharge.
Cauterization of erosion with radio waves: consequences and rehabilitation
Immediately after the session, you may experience minor discomfort in the lower abdomen and vaginal mucus, which contains minimal blood.
The described therapy for cervical erosion requires the woman to comply with the following medical instructions:
- Monthly abstinence from sexual intercourse. Otherwise, brown discharge may appear, which will stain the blood from the healing vessels;
- Immediately after the session and for one month after it, visiting saunas, swimming pools, natural reservoirs and water health clinics is prohibited;
- While the mucous membrane is healing, it is necessary to completely avoid carrying heavy objects.
In each individual case, the doctor himself writes out a complete list of precautions that a woman should follow after undergoing the procedure of non-contact cauterization of cervical erosion. In different patients, the treated mucous membrane heals at its own pace, and while one week is enough for some to recover, others may need a couple of months for a similar recovery.
In the case when, after treating erosion with radio waves, a woman continues to be bothered by painful or unpleasant sensations, she is allowed to take painkillers such as Ibuprofen or Acetaminophen. An increase in body temperature, as well as blood that does not want to stop flowing from the vagina, should be a reason for immediate contact with a specialist.
A lot of questions are asked about discharge after the procedure, which can often contain blood.
Transparent and slightly brownish mucus is almost normal, and it disappears if the following doctor’s recommendations are followed:
- Careful observance of personal hygiene, and the genitals in particular;
- Elimination of even minimal hypothermia;
- Refusal to be in hot water (even applies to showering and washing, not to mention steaming in the bathroom or warming up using traditional methods).
Correct and timely use of radio waves allows you to get rid of erosion literally in one session, and this without pain and blood. But if you refuse this or any other therapy, then after a couple of years of ignoring the problem will develop into a large-scale erosive process, inflammation, heavy bleeding, infertility and tumors.
Established restrictions
You can avoid problems in the postoperative period if you follow the recommendations of doctors. Doctors say women need:
- do not lift heavy objects;
- do not visit swimming pools, open reservoirs, saunas, baths;
- refuse any physical activity;
- avoid situations in which the cervix may be injured (sexual activity, douching, and the use of tampons are temporarily prohibited).
If a woman does not want to start bleeding when the scab comes off, then she should stop using medications that thin the blood. Acetylsalicylic acid, Warfarin and similar drugs are prohibited.
Some people say that you should not sit for a week after conization. But only a part of operating gynecologists adhere to this opinion. Others do not see the connection between sitting and healing of the cervix in the postoperative period.
Possible complications
In most cases, after conization of the cervix, the scab comes off painlessly. But some women say that this period is accompanied by the following:
- pain appears in the lower abdomen;
- there is discomfort in the cervical area;
- the amount of bleeding increases.
Patients claim that the pain is similar in nature to menstrual pain. They can be pulling and aching. If necessary, you can take Ibuprofen or Ketonal to alleviate the condition. If cutting, sharp pain occurs, you should consult a doctor.
An examination by a gynecologist is necessary if a woman’s scab comes off and the following is recorded:
- temperature rises;
- intense discharge began, reminiscent of bleeding;
- severe itching bothers me.
Dead tissue does not always begin to come off painlessly. Cutting pains accompanied by the appearance of heavy bleeding may indicate damage to the tissue of the cervix. In this case, the gynecologist must treat the damaged area to stop the bleeding. This way the scab should not come off. Women are also prescribed antibiotic therapy to prevent complications.
Some people feel great discomfort as the scab comes off. Patients complain of weakness, drowsiness, chills, and slight dizziness.
Many people are interested in how exactly the scab comes off after conization of the cervix. You can understand that the process of its rejection has begun if you look at the discharge. In them, women may notice dried blood in the form of crusts.
Symptoms and examination
A cervical defect is detected during a gynecological examination and is a so-called diagnostic finding. This is due to the fact that ectopia does not have specific symptoms, for example, pain, abnormal discharge and bleeding. Ectopy does not affect the duration of the cycle.
However, we should not forget that usually a spot on the cervix is accompanied by other gynecological diseases. That is why some women mistake manifestations of other diseases of the female genital area for ectopia. Therefore, if unusual symptoms appear, you must contact a gynecologist and undergo an examination.