Cervical cancer has been one of the most common malignant tumors for the last 30 years. According to statistics, this disease ranks second among all cancer pathologies in women after breast cancer. Every year, oncologists and gynecologists identify approximately 500 thousand cases of this oncology.
APPOINTMENT WITH AN ONCOLOGIST—RUB 1,000. APPOINTMENT WITH A GYNECOLOGIST – 1000 rub. CONSULTATION WITH DOCTORS ON THE RESULTS OF ULTRASOUND AND ANALYSIS - 500 rubles!
CLICK TO SIGN UP
The growth rate of the tumor is high, and the initial stages are asymptomatic, so the tumor is detected in the later stages, when long and complex treatment is required or it is no longer possible to help the patient.
Causes
Malignant formations arise as a result of the oncogenic activity of the P-53 gene. Cervical cancer is no exception. In light of modern ideas about the development of cervical cancer, it is also necessary to point out that cervical cancer is a disease that can be sexually transmitted due to the presence of chronic infection with oncogenic types of human papillomavirus (HPV). There are some factors that increase the risk of cervical cancer.
- Causes of cervical cancer:
- Beginning of sexual activity before age 16
- Frequent change of sexual partners
- A large number of pregnancies and births
- HPV - human papillomavirus
- Sexually transmitted diseases
- HIV infection
- Long-term use of oral contraceptives
- Smoking
Individuals infected with the human immunodeficiency virus (HIV) also frequently become infected with HPV and are at higher risk of developing both obligate cervical precancer and cervical cancer itself. In most cases (about 75%), women diagnosed with cervical cancer also have human papillomavirus (HPV). From this fact we can conclude that most often it is HPV that is the root cause of the appearance of the tumor.
Cervical cancer
According to the decision of the International Agency for Research on Cancer, human papillomavirus serotypes 16, 18, 31, 33 and 35 are officially considered high-risk viruses for developing cancer. Therefore, among the risk factors is a frequent change of sexual partners - since the human papillomavirus can be transmitted even during protected sexual intercourse through micropores in a condom, not to mention the fact that many neglect the use of condoms and have casual sex. However, even if the human papillomavirus serotypes 16 and 18 has entered the body, its activity is controlled by the immune system; nevertheless, when the body’s defenses are weakened, the virus multiplies rapidly, causing irreversible changes in the cells of the cervical epithelium (this virus destroys the “antitumor” protection of the cells ).
The next risk factor is the earlier onset of sexual activity in girls - the fact is that up to the age of 16, immature epithelial cells of the cervix in girls are extremely susceptible to pathological changes and easily transform into cancer.
In addition, smoking abuse simultaneously weakens a person’s immunity and provokes the appearance of cancer due to the content of carcinogenic substances in tobacco smoke. Studies have shown that in many cases of cervical cancer, women, in addition to HPV, also had sexually transmitted diseases such as chlamydia, genital herpes, cytomegalovirus infection and HIV. Cervical cancer is preceded by a more or less long period of dysplasia, usually at the junction of squamous and columnar epithelium, which under certain circumstances can develop into invasive cancer. In cervical cancer, facultative obligate precancers are distinguished. Optional precancers (they are also called background processes of the cervix) are erosions, pseudo-erosions, polyps or condylomas. However, the presence of this condition does not mean that without treatment this condition will develop into a malignant tumor. If a woman is diagnosed with an obligate precancer (also called cervical intraepithelial neoplasia or CIN), then if the woman does not treat this disease, then this condition will directly develop into preinvasive cervical cancer, microinvasive cervical cancer, and then into invasive cervical cancer. Thus, despite the fact that cervical cancer is a potentially preventable disease in most countries of the world, its incidence remains quite high. Cervical cancer is the first most common malignant tumor of the female genitalia in developing countries and is approximately the third most common in economically developed countries.
Classification of cervical cancer
Stages of cervical cancer (table)
| Stage | Description | |
| Tx | The study is uninformative, there is not enough data to make a diagnosis | |
| T0 | The tumor is not detected (absent) | |
| Stage 0 or Tis | Preinvasive carcinoma - the found cancer cells do not form a tumor and are located on the surface of the cervical tissue | |
| Stage I or T1 | The tumor is located only on the cervix (A - detected microscopically, B - detected clinically) | |
| I A1 | Cancerous tumor up to 3 mm deep and up to 7 mm wide | |
| I A2 | Cancerous tumor up to 5 mm deep and up to 7 mm wide | |
| I B1 | Cancerous tumor up to 4 cm in size | |
| I B2 | Cancerous tumor larger than 4 cm | |
| Stage II or T2 | The tumor has spread beyond the uterus, but without germination into the pelvic wall and the lower third of the vagina | |
| II A or T2a | The tumor is located in the upper and middle third of the vagina | |
| II B or T2b | The tumor is located with invasion into the space surrounding the uterus | |
| Stage III or T3 | Cancerous tumor with spread to the pelvic wall and the lower third of the vagina | |
| III A or T3a | Tumor in the lower part of the vagina, but without damage to the pelvic wall and kidney | |
| III B or T3b | The tumor is widespread on the pelvic wall and leads to impaired kidney function | |
| Stage IV or T4 | The tumor has spread to neighboring organs | |
| IV A or 4a | Cancer has spread to the bladder or rectum or extends beyond the pelvic area | |
| IV B or 4b (stage M1) | Metastases were detected in distant organs | |
Photos of cervical cancer stages
According to the levels of damage, the following stages of cervical cancer are distinguished: first stage - oncology is limited to the cervix; second stage, the oncological process has spread beyond the cervix, but has not affected the pelvic wall and the lower third of the vagina; third stage - the malignant tumor has spread to the pelvic wall, the lower third of the vagina and caused hydronephrosis; fourth stage - the tumor process has spread to the area of the rectum, bladder, and in stage 4b metastases appear in distant organs.
Of course, the earlier cervical cancer is diagnosed, the better the prognosis.
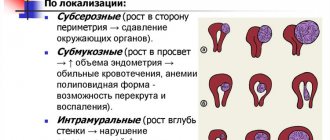
The following forms of cervical cancer are also distinguished: exophytic form - when the tumor grows in the vagina in the form of a cauliflower; endophytic form - the tumor grows in the thickness of the cervix and the cervix becomes barrel-shaped; ulcerative-infiltrative and ulcerative-necrotic form.
Signs and symptoms of cervical cancer
Diagnosis of cervical cancer is greatly complicated by nonspecific and scanty symptoms. At the early stage of the disease, the symptoms are mild; they gain strength as the malignant tumor grows and develops.
The first subtle signs of a precancerous condition and the initial stage of cervical cancer:
- failure of the menstrual cycle (menstruation disappears altogether or becomes too long, painful, discharge is unusually large or too scanty);
- bleeding after sexual intercourse, gynecological manipulations, douching;
- unusual vaginal discharge (clear, white, pink or brownish, patchy, mixed with blood) not associated with menstruation;
- unpleasant odor from the genitals, discharge of purulent masses;
- sensations of inflammation in the genital organs (itching, itching, pain during or after sexual intercourse).
At subsequent stages of cancer development, the above are joined by new symptoms that are much more pronounced:
- nagging pain below the abdomen, in the lumbar region;
- copious watery discharge;
- difficulty in the functioning of the urinary system, rare urination, problems with bowel movements, blood in the urine and feces;
- large size and pain of the lymph nodes;
- swelling of both or just one leg (as a result of narrowing of the vessels in the pelvic area).
In addition to signs of genital disease, one can observe a significant deterioration in a person’s general condition: a feeling of powerlessness, exhaustion, weakness, drowsiness appears, the woman quickly gets tired, loses appetite, loses a lot of weight, sweats unusually a lot, the skin turns pale and peels, and the body temperature rises.
First signs and symptoms
This type of tumor is rarely detected in the early stages, since at first the symptoms are completely absent or manifest themselves in the form of difficult-to-differentiate discomfort. However, as the disease progresses, the following symptoms begin to appear:
- Symptoms of cervical cancer:
- Heavy vaginal bleeding not associated with menstruation
- Lower abdominal pain
- Beli
- Changes in the menstrual cycle
- Pain and bleeding after intercourse
- Prolonged general fatigue and weakness
- Sudden weight loss
Also, the development of cervical cancer may be accompanied by systemic effects such as increasing weakness, increased fatigue, weight loss, anemia, and increased ESR.
Where to treat cervical cancer
If you have symptoms of cervical cancer or simply want to undergo a preventive examination, contact the modern Diana Clinic. We have our own laboratory, equipped with everything necessary for taking samples and diagnosing a tumor at the primary stage of development. The advantages of our medical center are the high professionalism of gynecologists and oncologists, and the affordable cost of treatment.
If you find an error, please select a piece of text and press Ctrl+Enter
Diagnostics
Due to the absence of pronounced symptoms at the initial stage of the formation of pathological changes in epithelial cells, regular (at least once every 2-3 years) examinations (examination) by a gynecologist are necessary for the timely detection of malignant neoplasms of the cervix. The first method that allows you to reliably detect cancer cells is an oncocytology smear (with its help you can detect cancer at any stage). Poikilocytosis found during a cytological examination is a symptom of a precancerous condition.
RMS (scheme)
If signs of cancer are detected, the woman is sent for the next test - colposcopy. Briefly, the essence of the procedure can be described as follows: the gynecologist applies special medical reagents (acetic acid solution or Lugol's solution) to the cervix of the uterus with a soft swab and studies changes in the tissue of the cervix through a colposcope - an optical device with an image magnification of 40 times - with such treatment, pathologically changed cells some stand out in a different color against the background of healthy ones. In this case, a biopsy is taken from the cervix to further study the structure of the cells. Diagnosis of cancer and precancer of the cervix includes a clinical-visual method when an analysis of the patient’s complaints is performed, a general examination is performed, examination of the cervix in the speculum and manual examination, colposcopy, as well as morphological research methods such as the cytological method of examining smears, the histological method of examining biopsy specimens and molecular biological research methods (PCR).
- To fully diagnose cervical cancer, it is also necessary to carry out the following types of diagnostics:
- Ultrasound of the pelvic organs
- Ultrasound of the abdominal organs
- Chest x-ray
- Cystoscopy
- Sigmoidoscopy
- CT, MRI
Methods for diagnosing cervical cancer
The examination of the patient always begins with a visual examination on the gynecological chair using mirrors. Based on the appearance of the surface of the mucous membranes of the cervix (growth, unevenness, the presence of ulcers, growths), a qualified doctor may suspect a defect in the integument.
A cytological examination of a smear from the mucous membrane of the cervix and cervical canal should be carried out at a gynecological appointment annually for every woman. It allows us to identify early structural changes that can subsequently lead to a precancerous or cancerous state of cells.
Staining the epithelium of the cervix with solutions of acetic acid and Lugol makes it possible to identify areas with signs of cell degeneration into malignant ones; in the photo they are distinguished by heterogeneous staining.
Using colposcopy, the doctor examines the cervix in detail with a magnification of up to 40 times. This enlargement of the picture allows for the diagnosis of erosion, leukoplakia, dysplasia and other precancerous conditions of the cervix, as well as cancer in the initial stages.
Biopsy is the removal of a piece of the surface of the cervix using a scalpel or an electric knife for subsequent thorough examination under a microscope for the presence of cancer cells.
Ultrasound and computed tomography of the pelvis are prescribed after cancer is diagnosed to determine the extent of tumor growth and the stage of the disease; necessary before surgery to create the most effective surgical plan.
Since in most cases with cervical cancer, renal dysfunction can be observed, up to complete failure, their condition is determined using urography.
To analyze the condition of the intestines and bladder, rectoscopy and cystoscopy are prescribed.
In the later stages of cancer, if metastasis of the cancerous tumor is suspected, an x-ray and ultrasound examination of the chest and abdominal cavity should be performed.
Treatment
To treat cervical cancer, an integrated approach is used, which includes a combination of several methods:
- Treatment methods for cervical cancer:
- Surgical
- Radiation therapy
- Chemotherapy
- Immunomodulatory therapy
Surgical
The first principle of treatment is the surgical method - the method of choice in the early stages. The surgical method of treating cervical cancer involves performing gynecological operations (surgical oncogynecology). There are two main areas of gynecological oncological operations - the first is organ-preserving, which is aimed at removing cancer tumors in the initial stages, while preserving reproductive functions in young nulliparous girls (for example, electrosurgical loop excision or cone-shaped amputation of the cervix) and the second - radical, aimed at removing severe cancerous tumors with removal of the uterus (for example, hysterectomy - removal of a woman’s uterus along with its appendages) - this method allows you to completely rid a woman of cancer, but unfortunately she will no longer be able to get pregnant. The method of surgical treatment - a radical operation is the Wertheim-Meigs operation - is extirpation of the uterus with appendages and lymphadenectomy of the pelvis and ligation of the internal iliac artery.
Radiation and chemotherapy
Radiation therapy, along with chemotherapy (and more often their combined use) occupies the main place in the treatment of cervical cancer in women in cases where surgical treatment is impossible (in later stages). In the case of radiation therapy, a dose of radiation is applied to the area where cancerous changes have occurred in the cells - this is combined radiation therapy (external and contact gamma therapy).
Cervical cancer treatment
If chemotherapy is used (used for a common process in the form of preventive courses, as well as for low tumor differentiation), then the woman is prescribed cytostatic drugs. These drugs, firstly, make it possible to increase the effectiveness of radiation therapy, and secondly, they help get rid of the tumor, and also reduce the chances of the appearance of a radiation-induced tumor.
Immunomodulatory therapy
This is a new direction in the treatment of cervical cancer - the point is to preserve a person’s immunity against the background of radiation and chemotherapy so that the body fights the tumor on its own. As immunomodulatory therapy, the administration of interferon drugs is used in various dosages, calculated by the attending physician.
Cervical cancer
Cervical cancer is a tumor lesion of the lower part of the uterus, characterized by malignant transformation of the integumentary epithelium (ecto- or endocervix). Specific manifestations of cervical cancer are preceded by an asymptomatic course; subsequently, contact and intermenstrual bleeding, pain in the abdomen and sacrum, swelling of the lower extremities, urination and defecation disorders appear. Diagnosis of cervical cancer includes speculum examination, extended colposcopy, cytological scraping examination, biopsy with histological conclusion, and endocervical curettage. Treatment of cervical cancer is carried out taking into account the histological form and extent using surgery, radiation therapy, chemotherapy or a combination of these.
Symptoms of cervical cancer
Symptoms of cervical cancer are divided into general and specific.
General symptoms: weakness, weight loss, loss of appetite, sweating, causeless rises in body temperature, dizziness, pallor and dry skin.
Specific symptoms of cervical cancer may include the following:
1. Bloody discharge from the genital tract, not associated with menstruation, can be slight, spotting, or profuse; in rare cases, bleeding is observed. Often, spotting occurs after sexual intercourse - 'contact discharge'. Possible manifestations in the form of acyclic discharge or against the background of menopause. In the later stages, the discharge may acquire an unpleasant odor associated with the destruction of the tumor.
2. Pain in the lower abdomen: may accompany bloody discharge, or occur in advanced forms of cancer as a result of infection or tumor invasion of other pelvic organs or structures (nerve plexuses, pelvic walls).
3. Swelling of the extremities and external genitalia occurs as the disease progresses in advanced and advanced cases; it occurs as a result of metastasis to nearby pelvic lymph nodes and their blocking of large vessels that drain blood from the lower extremities.
4. Impaired bowel and bladder function occurs when a tumor grows into these organs - the formation of fistulas (openings between organs that do not normally exist).
5. Urinary retention associated with mechanical compression of the metastatic lymph nodes of the ureters with subsequent shutdown of the kidney, the formation of hydronephrosis, the consequence of which is poisoning of the body with waste products (uremia) in the complete absence of urine - anuria.
In addition, the described changes lead to the penetration of purulent infection through the urinary tract and the death of patients from severe infectious complications. Hematuria (blood in the urine) is possible.
6. Edema of the lower limb on one side - can occur in the later stages, in the presence of metastases in the pelvic lymph nodes and compression of large vessels of the limb.
Treatment of cervical cancer (cervical cancer)
In the early stages of cervical cancer, the tumor is limited to the cervix. Treatment of such patients may be surgical (eg, modified radical hysterectomy or breast-conserving surgery). At the initial stages of treatment for cervical cancer, radiation therapy (in combination with or without chemotherapy) can also be used. The choice of treatment method depends on both the characteristics of the tumor and the patient’s condition.
Forecast
According to statistics, timely treatment for cervical cancer guarantees survival for at least 5 years:
- Cervical cancer survival rate:
- at stage I, the vast majority of patients 90%
- at stage II - 75%
- at stage III - 40%
- at stage IV - 10%
It follows from this that timely diagnosis and treatment begin save the lives of women diagnosed with cervical cancer.
Klinnik
The first signs of cervical cancer can be observed during a gynecological examination of a woman, since the tumor in the first stages develops asymptomatically, although sometimes liquid discharge may appear.
When the cancer process is already advanced, a woman may observe spotting, which appears chaotic and may intensify before or after menstruation. According to reviews, bleeding from cancer can be contact, that is, after physical activity, sexual intercourse, after a vaginal ultrasound or palpation examination. Symptoms of pain may be felt when there is cervical stenosis, which retains discharge in the uterus. When the tumor grows and presses on the sacral plexus, pain also occurs. Severe and prolonged pain is observed in women who have a late stage of cancer with tumor cells growing into nearby tissues and organs. When pelvic vessels are compressed by infiltrates of cancer, symptoms are observed, which are expressed by edema of the lower extremities and, in severe cases, hematuria, diarrhea with blood and renal failure.
Prevention
To prevent the occurrence of cervical cancer, modern medicine recommends regular examinations by a gynecologist.
It is recommended to visit a gynecologist at least once a year with a visual examination and taking a smear for flora. A cytological examination or colposcopy must be performed at least once every 3 years - this is where the first signs of cervical cancer can be detected and, if necessary, a biopsy can be taken from suspicious tissues.
Also, during examinations, the gynecologist can identify precancerous conditions - cervical erosion or dysplasia, which are subject to treatment. The time between visits to the gynecologist is reduced for those women who have risk factors for gynecological oncology, for example, are infected with the human papillomavirus or have had a large number of sexual partners (risk factors are described in more detail in the “Causes” section).
- In addition to inspections, it is necessary to observe preventive measures:
- The sexual partner must be permanent; frequent changes of partners are highly discouraged
- It is advisable to avoid long-term use of oral contraceptives
- The use of a condom during sexual intercourse (especially with unfamiliar partners) is mandatory
- Smoking is harmful. Give it up
- Chronic sexually transmitted diseases also increase the risk of cancer
Women who have undergone a course of treatment against cancer and defeated it must undergo smears for oncocytology at least 2 times a year in the first 3 years after the end of treatment - this is necessary for timely detection of the return of cancer (unfortunately, such cases do occur). It is the state and development of prevention that largely determines the level of incidence of malignant tumors in the population and mortality from them. We are talking about comprehensive prevention of malignant neoplasms, including primary, secondary and tertiary prevention.
Development of cervical cancer
Primary prevention is aimed at preventing the occurrence of malignant tumors and the pre-tumor processes that precede them. Secondary prevention of malignant tumors is aimed at identifying and treating pre-tumor diseases and early-stage malignant tumors. The objectives of tertiary prevention are the prevention, as well as early detection and treatment of relapse of the disease after completion of the main course of treatment. Vaccination is a method of primary prevention. There are two vaccinations (vaccines) against the human papillomavirus, which in turn plays an important role in the occurrence of cervical cancer - Gardasil and Cervarix. Both vaccines have clinically proven effectiveness in protecting against oncogenic human papillomavirus serotypes 16 and 18 (these vaccines are used only as a preventive measure; they are powerless against HPV that has already entered the body). The course of using the Gardasil vaccine consists of 3 vaccinations (the first vaccination is given on the day of administration, the second is given 2 months after the first, and the third 4 months after the second). When using Cervarix, the duration of the course remains the same, but the second vaccination is given 1 month after the first.
What are the types of discharge due to uterine cancer?
Pain due to uterine cancer
Cervical cancer most often has a latent course, especially in the initial stage. Therefore, it is most often diagnosed accidentally, when a woman consults a doctor for other reasons. Often this cause is vaginal discharge of various types.
Most often they appear on days that fall in the middle of the menstrual cycle, but not all women attach importance to scanty bleeding. They are usually not painful or accompanied by other symptoms, but only at the beginning of cancer development.
Characteristics of discharge in cervical cancer:
- Dirty pink discharge with a green tint indicates the beginning of tumor disintegration. They usually appear during physical activity associated with lifting weights or tensing the abdominal muscles. Sexual intercourse can also provoke the appearance of discharge, this is due to the increased sensitivity of tissues affected by cancer. Trauma to these areas during sexual intercourse causes bleeding.
- If a woman has reached menopause and has bloody discharge, she should consult a doctor; such symptoms are characteristic of a malignant neoplasm.
- In women of childbearing age, slight bleeding may appear in the middle of the cycle and in the absence of an external irritant. This is usually a brown discharge, mucous in consistency, and may have an unpleasant odor. The appearance of any discharge should prompt the woman to visit the clinic. Dark brown discharge can also appear with other pathologies, such as polyps in the uterus, but in any case the woman needs to see a doctor.
- A malignant neoplasm can cause sudden heavy uterine bleeding. This occurs due to the destruction of the walls of the blood vessels of the woman’s genital organs.
- Sometimes bleeding from cervical cancer and characteristic symptoms may be absent. The pathology may appear as yellowish mucus with an unpleasant odor.
- In some women, especially in the early stages of the disease, the discharge may be white, watery or foamy, with or without an odor. This is usually due to the onset of tissue necrosis and opening of the lymph nodes. In addition, an infection can join the development of oncology and cause an inflammatory process with the additional production of vaginal discharge that has an unpleasant odor.
A woman should pay attention to how her periods proceed; if they become heavier and more painful, this may be associated with the development of cancer.
Cervical cancer screening
The target groups are women 30-70 years old, with the following laboratory tests carried out every 4 years: all women in this target group undergo a Pap test - a diagnostic method that identifies women at increased risk of developing cervical cancer. If necessary, extended colposcopy and HPV testing are also performed. A screening examination aimed at detecting cervical cancer consists of 3 stages: the first stage is the filling out of a statistical outpatient card by mid-level medical personnel at the level of medical stations, paramedic outpatient clinics, medical outpatient clinics and examination rooms. At the second stage, if necessary, this is an in-depth examination and further tactics at the level of a city or regional clinic. The third stage of providing specialized care at the level of a city or regional oncology clinic. Remember, it is the timely detection of the first signs of precancerous conditions and cancer cells and promptly initiated treatment that plays a decisive role in preserving the life and health of a woman - the survival rate of patients with stage I cancer reaches 90%. In addition, treatment of stage I cancer helps preserve a woman’s reproductive function; she not only remains healthy, but will also be able to have children in the future. Therefore, everything is in your hands - regular examinations with a gynecologist will help maintain your health.
This may be useful for you:
Cause of cervical cancer
Like any malignant neoplasm, cervical cancer is caused by damage to the genetic connections of cells due to various traumatic environmental factors.
The threat to women is:
- viral infections: herpes, papilloma virus;
- birth injuries to the cervix, urological infections;
- promiscuity or early initiation of sexual activity;
- smoking and other carcinogenic intake.
A precancerous disease, the likelihood of which will transform into cancer is very high - dysplasia of the cervical mucosa. This condition is detected at an appointment with a gynecologist, so you should visit a specialist at least twice a year. If dysplasia is detected, the specialist conducts an examination and prescribes treatment that can completely prevent uterine cancer.
It is also recommended to undergo regular examination by a female urologist for timely detection of urological infections - their timely treatment reduces the risk of dangerous pathology by 20%.