6296
0
The pathology is increasingly found not only in older women, but also in young girls and, worst of all, in nulliparous women. Statistics show that this disease is the most common in women after breast cancer.
Unfortunately, it is very difficult to identify the disease at an early stage of development, since the symptoms are mild, so patients are in no hurry to contact specialists, and lost time that could have been spent on treatment aggravates the situation. The stages of the disease have their own symptoms and prognosis. The lower the level of damage, the greater the chance of recovery.
Causes of the disease
The exact causes of the development of cancer are still not fully understood. Typically, this requires the influence of a number of factors, one of which is the entry of HPV or human papillomavirus into the body. However, the disease begins without infection, provided there are problems with the immune system.
They appear against the background:
- Smoking (more than five cigarettes per day);
- Promiscuous sexual intercourse (this includes the husband’s numerous partners);
- Pregnancy;
- Progressive sexually transmitted infections (genital herpes, cytomegalovirus);
- Childbirth at an early age;
- Poor nutrition, lack of vitamins (especially A and C);
- Genetic predisposition to cancer pathologies;
- Long-term use of hormonal drugs;
- Refusal to use barrier contraceptives;
- Early onset of sexual activity, before the age of eighteen.
When the human papillomavirus enters the body, it leads to the formation of condylomas. Over time, they can degenerate from benign to malignant tissue. Similar processes are observed with leukoplakia, erosion and cervical dysplasia, so they need to be diagnosed and treated in time.
Prevention
Prevention of uterine cancer allows you to minimize the likelihood of developing pathology. In this regard, women are recommended:
- Get vaccinated in a timely manner against the human papillomavirus, which can lead to the appearance of a malignant tumor (this must be done before the start of sexual activity).
- Lead a healthy lifestyle, including regarding sexual relations.
- Complete routine examinations and screening examinations in a timely manner.
- Immediately begin treatment of precancerous conditions when they are detected.
- Avoid abortion if possible (induced abortion has a negative effect on the cervix).
Classification of stages
Cancer stages are classified according to different systems; the international TNM is considered more common. It more accurately determines how strongly the process is running. Cervical cancer has four stages with several additional grades.
Stages of the disease:
- T0. This abbreviation denotes healthy people without cancer education;
- T1. The first stage of cancer, which is divided into T1 A and T1 B;
- T2. The second stage of cancer, which has a similar division into T2 A and T2 B;
- T3. The third stage of cancer, divided into T3 A and T3 B;
- T4. The fourth stage has no additional division.
Stage 2 A indicates the exact localization of malignant cells; they have not yet spread to adjacent tissues of the periuterine space. At this stage, the cancer is able to reach the upper parts of the vagina, but cannot affect nearby lymph nodes or organs located far from the localization point.
Stage 2 B means that malignant cells have reached the periuterine space. However, they are still not present in any distant organs or nearby lymph nodes. The main difference between the stages is the presence or absence of damage to the parametrium fiber.
Characteristics of the second stage
It is easiest to cure a disease detected at the first stage, however, even in the case of the second stage, patients have a chance of survival under surgical intervention. This stage is characterized by the formation extending beyond the cervix, but it has not yet affected the lower third of the vagina and the pelvic wall.
Types of process propagation at the second stage:
- Vaginal. Malignant cells invade the upper part of the vagina;
- Parametric. Pelvic tissue is affected on both sides, but metastasis does not form;
- Transition to the body of the uterus. A particularly severe type of spread of the disease.
During this period, the malignant formation becomes large enough to be seen with the naked eye, but the symptoms often remain blurred. Patients often encounter signs characteristic of any cancer process.
Among them:
- Weakness, loss of strength;
- Poor appetite;
- Unexplained weight loss;
- Reduced ability to work;
- Dizziness;
- A slight increase in temperature that does not go away.
The second stage of cancer has more specific symptoms. First of all, this is bloody vaginal discharge that begins immediately before or immediately after menstruation. They acquire a sharp, unpleasant odor associated with cell decay. Sometimes blood appears after sexual intercourse or after lifting heavy objects.
Due to pathological bleeding, menstruation becomes profuse, and the cycle is often disrupted. Depending on the size of the tumor, some patients experience pressure on the pelvic organs. As a result, swelling of the legs develops, and cases of intestinal obstruction and pain during urination occur. Typically, after these symptoms, a person experiences a loss of strength and sudden weight loss.
Characteristic signs of this stage
Depending on the extent of the process, uterine cancer (CC) is divided into stages 2A and 2B. In the first case, cancer cells spread from the cervix to the upper parts of the vagina, in the second - to the periuterine space and body of the organ (metastases are not observed either in nearby lymph nodes or in distant tissues).
As the pathology progresses, women begin to worry about the following symptoms:
- the appearance of bloody, foul-smelling discharge after sexual intercourse, lifting heavy objects, before menstruation or immediately after its completion;
- pain of aching nature, periodic in nature and intensifying against the background of excessive physical exertion;
- Irregularities of the menstrual cycle - its lengthening or shortening, prolonged heavy menstruation.
In addition, there are signs characteristic of all types of malignant neoplasms:
- weakness;
- dizziness;
- decreased performance;
- loss of appetite;
- sudden weight loss;
- slight increase in body temperature due to the presence of inflammation;
- anemia (detected by a blood test).
Diagnosis of the disease at the second stage
To diagnose cervical cancer at the second stage, various methods are used, including cytological examination. This process involves collecting cells from the surface of the affected area. The structure of tissues is examined under a microscope. If anomalies are noticed, additional studies are carried out.
Other diagnostic methods:
- Biopsy. Intravital tissue sampling followed by histological examination;
- Colposcopy. Examination of the cervix using a colposcope;
- Ultrasound. Effective when viewed in three dimensions. If the cancer has spread too much, or the patient has abdominal adhesions, the examination result is blurred;
- Curettage of the cervical canal. It is carried out after a cytological examination if abnormalities were noticed, but more often doctors turn to colposcopy;
- Magnetic resonance imaging. Used to assess the health of neighboring organs and select treatment tactics.
After diagnosing the disease, it is necessary to examine the body for the development of metastases, including in distant organs. Therefore, doctors prescribe skeletal scintigraphy, chest x-ray and computed tomography of the abdominal cavity.
Analyzes
An integral element of diagnosing cervical cancer is an analysis for the human papillomavirus. The PCR method determines the type of pathogen and detects the presence of particles of high oncogenic risk. To find out the degree of virus concentration in a biopsy specimen, an HPV DNA test is used.
The blood of sick women is checked for the presence of tumor markers. Cervical cancer is characterized by an increase in SCC. The larger the size of the education, the more the indicator increases. However, the presence of a tumor marker in the blood does not guarantee that cancer develops in the cervix. The growth of SCC sometimes indicates cancer of the lungs, vagina, vulva, esophagus and other organs.
Note. Changes in tumor markers are taken into account if the diagnosis was confirmed by biopsy.
Biopsy is one of the decisive diagnostic elements. It is mandatory to carry out in cases of suspected oncological processes, with the exception of situations where the procedure becomes impossible.
Contraindications to biopsy are:
- Period of menstruation;
- Pregnancy;
- Problems with blood clotting;
- Infections and inflammations of the genital organs.
Most often, a biopsy is performed 5-7 days from the first day of menstruation, since during this period the damaged tissues have time to heal. This is done on an outpatient or inpatient basis, using local anesthesia if necessary. After the biopsy, a sick leave certificate is issued for several days or a certificate of incapacity for work for a week.
Development of the disease
Numerous studies have proven that human papillomavirus DNA is found in almost all cases of precancerous conditions and cervical cancer. HPV infection precedes subsequent squamous (squamous) intraepithelial dysplasia of the cervix. The third stage of intraepithelial neoplasm of the cervix (stage 0) occurs only in the presence of persistent infection with high oncogenic risk papillomavirus genotypes (usually types 16, 18).
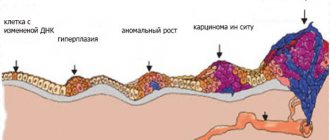
Typically, cervical cancer develops slowly over several years (5-10 years). It usually takes about 10 years from the onset of stage 0 carcinoma to invasive cervical cancer. Before tumor cells develop, the cervical tissue undergoes changes at the cellular level - epithelial dysplasia appears. If left untreated, it progresses from mild to moderate to severe. CIN III includes both severe dysplasia and intraepithelial carcinoma or carcinoma in situ. This is an early stage of non-invasive cancer.
The progression of pathological changes on the cervix to invasive cancer goes through the stage of microinvasive cancer, which can only be determined by histological examination of the tissue. Cervical cancer detected at an early stage can almost always be cured. The five-year survival rate for cancer in situ (atypical cells do not spread beyond the surface layer) is 100%; Ia art. - 96.8%; Ib art. - 92.4%. Depending on the prevalence, cervical cancer is divided into (see table below).
Stages of cervical cancer
| TNM stage | FIGO stage | Description |
| Tx | Little data available for tumor assessment | |
| T0 | The primary tumor is not determined | |
| Тis | 0 | Preinvasive carcinoma, carcinoma in situ |
| T1 | I | Cancer limited to the cervix (excluding the uterine body) |
| T1a | IA | Invasive tumor only microscopically |
| T1 a1 | IA 1 | Stromal invasion up to 3.0 mm in depth and up to 7.0 mm in surface |
| T1 a2 | IA 2 | Stromal invasion up to 5.0 mm in depth and up to 7.0 mm on the surface |
| Т1b | I.B. | Clinically detectable lesion limited to the neck or microscopically detectable lesion larger than T1A/1A2 |
| T1 b1 | IB1 | Clinically detectable lesion up to 4.0 cm in greatest dimension |
| Т1 b2 | IB2 | Clinically detectable lesion greater than 4.0 cm |
| T2 | II | Tumor of the cervix with spread beyond the uterus, but without invasion of the pelvic wall or lower third of the vagina |
| T2a | IIA | Without parametrium invasion |
| Т2b | IIB | With parametrium invasion |
| T3 | III | Cervical cancer with spread to the pelvic wall, damage to the lower third of the vagina, impaired renal function |
| T3a | IIIA | The tumor affects the lower third of the vagina, but does not spread to the pelvic wall |
| T3b | IIIB | Tumor extends into the pelvic wall and/or results in hydronephrosis and a non-functioning kidney |
| T4 | IVA | The tumor spreads to the mucous membrane of the bladder or rectum and/or extends beyond the pelvis |
| M1 | IVB | Distant metastases |
Symptoms
Initial forms of cervical cancer (cancer in situ, microinvasive cancer) are asymptomatic. In the early stages there are no signs or they are associated with concomitant diseases. More often it is: contact bleeding, usually corresponds to invasive cancer. discharge like meat slop, pain, fever, dysfunction of neighboring organs usually correspond to advanced forms of cancer. In case of advanced cancer, the cervix is enlarged, barrel-shaped, with an uneven tuberous surface, uneven pink-marble coloring; rectovaginal examination reveals infiltrates in the parametrium and small pelvis.
The main symptom for diagnosing “cervical cancer” in gynecology is the detection of a “focus of tumor growth.” As it develops, subtle visual changes appear, contact bleeding and leucorrhoea (pathological discharge), sometimes irregular menstruation.
Early diagnosis of cervical cancer
If cervical cancer is suspected, tests are necessary to clarify the diagnosis and establish the stage of the disease (determine the form of tumor growth, its relationship with surrounding structures), and assess the condition of other organs and systems.
The most important diagnostic methods and tests for cervical cancer:
- Liquid cytology for preclinical forms of cancer (stage 0-Ia), when the cervix cannot have visible changes.
- Vaginal examination with speculum, rectovaginal, bimanual palpation.
- Incisional biopsy of the lesion in the neck, at the border of tumor and normal tissue;
- Digen test analysis for HPV oncotypes and their number;
- Curettage or aspiration from the cervical canal, depending on the condition of the cervix;
- Extended colposcopy to establish the boundaries of the pathological process, targeted biopsy and removal of the lesion;
- Cystoscopy to determine whether the bladder is involved in the process;
- Tests for tumor markers (SCC, HE4, etc.);
- Cone biopsy (therapeutic and diagnostic).
CERVICAL CANCER TESTS
Considering that everything usually starts with precancer, regular screening examinations for cervical cancer, including examination by a gynecologist, provide a good diagnostic effect. This allows you to notice and begin treatment of pathology at an early stage. The detected cytological signs of cervical cancer in a smear analysis for oncocytology during screening studies include the following gradations:
- Cytogram without features (normal),
- Inflammatory type of smear (high risk of precancer),
- Dysplasia 1, 2, 3 (precancer):
- Suspicion of cancer
- Cervical cancer.
Cervical cancer treatment
If cervical cancer is detected at the first stage, treatment is carried out through surgery. Radiation therapy acts as an additional intervention. This is also typical for stage 2 A. If surgical intervention is possible, hysterectomy is performed, that is, removal of the cervix and body. As a result of the operation, complications often arise in the form of:
- Fistulas;
- Adhesive bowel disease;
- Bleeding;
- Pulmonary embolism;
Stage 2 A is usually treated with a combination of brachytherapy and radiation. For cancer that has grown more than four centimeters in diameter, chemotherapy is added to the treatment package. Sometimes doctors turn to radical hysterectomy, that is, removal of the pelvic lymph nodes. Chemotherapy or radiotherapy consolidates the result.
Save article
For contact irradiation, substances such as:
- Cobalt;
- Iridium;
- Cesium.
When the disease progresses to stage 2 B, treatment focuses on chemotherapy and radiotherapy, and sometimes external beam irradiation is used. Upon completion of the course, doctors monitor the further course of the pathology. If positive dynamics are detected, a Werthemer operation is performed.
Complications
Complications of uterine cancer develop both as a result of the progression of the pathology and during its treatment. In the first case, new organs will be involved in the process, which ends in the death of the sick. In the second, the consequences are determined by the impact of certain therapeutic methods on the body.
The results of chemotherapy are:
- baldness caused by damage to hair follicles;
- nausea;
- loss of appetite;
- bleeding and the appearance of hematomas.
As a result of exposure to radiation therapy, women experience:
- weakness and chronic fatigue;
- difficulty urinating;
- deterioration of the condition of the skin - they become dry and irritated;
- pain, burning and dryness of the genitals.
The consequences of surgery may be:
- fistulas;
- adhesive bowel disease;
- bleeding;
- pulmonary embolism;
- problems with excretion of feces and urine;
- the onset of menopause.
In addition, you should remember the psychological aspect. Detection of the disease entails depressive states, and after the operation, many sick women experience emotional devastation. In this case, they need the help of psychologists.
Features of treatment
If the doctor sees the possibility of surgery, he can remove different parts of the organ, depending on the severity of the pathology. Sometimes in the second stage, conization of the cervix is sufficient, which will allow the woman to have children in the future.
Note. The issue of ovarian removal is considered individually in each case.
Typically, during the operation, the pelvic lymph nodes, uterine body and paracervical tissue are removed. Radiotherapy is then used to consolidate the result. The choice of dosage is influenced by previous treatment and the volume of previously received radiation. In the second stage of cancer, it is not always possible to achieve a complete recovery. If the patient experiences a relapse, she is treated with chemotherapy and radiation therapy using:
- Paclitaxel;
- Rinotecan;
- Capecitabine;
- Ifosfamide;
- Cisplatin.
One of the newest methods for treating cervical cancer at the second stage is photodynamic therapy. The procedure involves the introduction of a photosensitive component into the formation, which is then exposed to a laser.
If cancer treatment does not give a positive result, the disease begins to destroy the woman’s body. First of all, the reproductive system suffers. Gradually, the malignant tumor spreads beyond the cervix, affecting its body and increasing the risk of metastases. Their spread throughout the body poses the greatest danger.
Forecast
The answer to the question of how long people live with stage 2 uterine cancer is ambiguous and depends on a large number of factors. Factors influencing life expectancy include:
- speed of contacting a doctor and the latter’s qualifications;
- age of the patient;
- presence of concomitant diseases;
- adequacy and timeliness of prescribed treatment;
- food and living conditions;
- state of the immune system;
- individual psychological attitude towards healing.
Some women recover completely and continue to lead almost full lives, while others’ bodies cannot cope with the disease, resulting in death. Survival rates range from 45 to 75% of cases.
Folk remedies
It is impossible to cure cancer with folk remedies, but it is permissible to use them as an element of a complex effect. Tinctures of hemlock and barberry are actively used. The latter is prepared as follows:
- Barberry leaves and 40% alcohol are mixed in a ratio of 1 to 5;
- The liquid is placed in a dark place for about seven days;
- Drink the prepared tincture 25 drops before meals, three times a day.
When using hemlock tincture for treatment, the number of drops taken is gradually increased. On the first day, drink one drop three times a day, on the second day, two. The dosage increase continues up to forty drops, after which it is reduced back to one in the same way.
Hemlock tincture can lead to poisoning, so it is necessary to monitor the condition of the body . If pathological symptoms occur, the dosage is reduced by five drops. Self-treatment is not recommended; medical supervision is required.
Reviews about the effects of hemlock:
“Effective at the initial stage, helps avoid relapses. It is important to be able to accept correctly; mature seeds need to be combined with immature ones.”
“If nausea occurs, you should take a break and reduce the dosage by a couple of drops until relief occurs. The diet should not contain detoxifiers such as dairy products. It’s better to lean on protein in the form of fish, eggs and meat; red caviar will help raise hemoglobin.”