Is chronic candidiasis treatable?
Currently, pharmaceutical companies offer a large selection of antifungal drugs indicated for the treatment of candidiasis. Medicines for internal and external use have a high therapeutic effect when identifying an infection in an acute form. The chronic form of candidiasis requires a long course of treatment and elimination of the causes that led to the development of the disease.
Thrush can be cured completely if you strictly follow the medication regimen prescribed by your doctor.
Also, in case of chronic fungal infection, a diet is required, which involves excluding yeast products, sweet dishes, and fresh milk from the daily menu.
Candidiasis of the genitourinary organs (thrush) in women
There are many drugs to treat this disease. Some of them are used topically (cream, vaginal tablets or suppositories), others are used orally (tablets or capsules for oral administration). For mild cases of vulvovaginal candidiasis (damage to the vagina and external genitalia), local treatment is sufficient. Drugs for topical treatment (vaginal tablets or suppositories) include (international names are given first, then commercial names are listed in parentheses): - clotrimazole (Antifungol, Yenamazole 100, Candibene, Kanesten, Kanizon, Clotrimazole) - the most common drug for local treatment; — isoconazole (Gyno-travogen Ovulum); — miconazole (Ginezol 7, Gyno-daktarin, Klion-D 100); — natamycin (Pimafucin); - nystatin (Polygynax, Terzhinan).
At the same time, nystatin (part of the drugs Polygynax and Terzhinan) is an outdated and not very effective drug.
Some doctors prescribe a 5-10% solution of borax in glycerin for candidiasis topically (in the vagina). This is a very ancient and ineffective method of treating candidiasis.
In addition, for mild cases of the disease, instead of drugs for local treatment, a single dose of fluconazole, 150 mg orally, is possible. Commercial names of fluconazole are Medoflucon, Diflazon, Diflucan, Mikosist, Forkan, Flucostat.
The use of vaginal tablets and broad-spectrum suppositories (Terzhinan, Polygynax, Betadine) for candidiasis is inappropriate, since these drugs contribute to the development of gardnerellosis. These drugs contain broad-spectrum antibacterial agents that suppress the normal microflora of the vagina.
In some cases, treatment is prescribed that complements antifungal drugs (immunotherapy, restorative drugs, physiotherapy, etc.).
Treatment of recurrent vaginal candidiasis If a woman experiences recurrent fungal infections regularly, this is a serious reason to be examined for endocrine and other chronic diseases. It is important to take into account the fact that chronic genital candidiasis usually affects nearby organs and systems of the body - the bladder, intestines. Therefore, to achieve complete cure and prevent re-infection, it is necessary to take antifungal drugs not only locally, but also orally. Treatment of patients with chronic forms presents significant difficulties. Treatment failure may be due to insufficient dosage and duration, as well as individual insensitivity to one or another group of antifungal drugs. Therefore, it is necessary to conduct bacteriological studies (cultures) to determine sensitivity to antifungal drugs. It should be taken into account that fungi have the ability to quickly adapt and develop resistance to the drugs used.
For recurrent candidiasis (more than 4 exacerbations during the year), the following treatment options are possible: - Suppositories or vaginal tablets with clotrimazole (Antifungol, Yenamazole 100, Candibene, Kanesten, Kanizon, Clotrimazole) once a week for several months. — Fluconazole (Medoflucon, Diflazon. Diflucan, Mikosist, Forkan, Flucostat) 100 mg orally once a week for several months.
It is advisable to treat recurrent vaginal candidiasis as recommended by a doctor. In some cases, examination and observation are necessary.
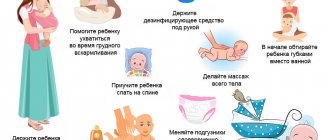
Treatment of candidiasis in pregnant women For candidiasis in pregnant women, only local treatment is indicated. And always under the supervision of a doctor.
Causes of the chronic form
Often, a man or woman who has successfully treated thrush does not follow all the doctor’s recommendations regarding sexual activity with one partner and the use of barrier protection during dubious sexual relationships. Secondary infection and the use of medications lead to a decrease in immunity, which in turn creates the preconditions for the development of another relapse of candidiasis.
Some patients, noting an improvement in their general condition and a decrease in the symptoms of a fungal infection, stop taking pills and using medications in the form of fungicidal ointments. An incomplete course of therapy causes exacerbation and development of complications.
Candida actively grows in the presence of diseases associated with metabolic disorders, including diabetes. In these cases, candidiasis quickly becomes chronic and difficult to treat.
Also, the reasons for the development of chronic thrush may be:
- diseases of the genitourinary system;
- kidney or liver pathologies;
- hormonal imbalance;
- frequent use of antibacterial drugs;
- reduced immunity.
Normally, a certain amount of fungi is present in many people, but candida begins to become active when the functioning of the immune system deteriorates, which weakens under severe and prolonged stress, infatuation with sweet foods and marinades, and alcohol-containing drinks. Hypothermia of the body can also contribute to the activation of pathogenic bacteria and fungi. People suffering from tuberculosis, HIV, and leukemia are prone to developing chronic candidiasis. In such patients, fungi often affect the mouth and intestines.
Prevention
The symptoms of thrush are unpleasant and interfere with a quiet life. The best way to avoid getting to know her is prevention.
To do this, just follow the recommendations:
- do not engage in casual sex;
- use breathable underwear;
- maintain personal hygiene, but do not use antimicrobial agents excessively, so as not to wash out the healthy microflora;
- monitor body weight, include more fruits, vegetables, dairy products in the diet, limit the consumption of sweets and starchy foods;
- When using antibiotics, follow your doctor's instructions.
Signs and symptoms of the chronic form in men and women
Despite the fact that women are more likely to develop chronic thrush, the stronger sex may also exhibit symptoms of the disease. 30% of men are Candida carriers. Their fungal infection is activated under the influence of a number of factors.
The chronic form of candidiasis is manifested by the following symptoms:
- Pain syndrome. Unpleasant sensations occur in the groin area, penis when emptying the bladder, during sexual intercourse.
- Spots on the skin and mucous membranes. They appear in the lower abdomen, penis and have yellowish, brown or red shades. Later, the skin becomes covered with peeling and blisters.
- Urethritis. Infection of the urinary tract by fungi and the development of inflammatory processes causes problems with urination.
- Unpleasant odor and white coating. Such symptoms are characteristic of both acute and chronic forms of thrush.
The manifestation of candidiasis in women is similar to the signs of fungal disease in men. The symptoms are:
- white vaginal discharge;
- discomfort when urinating;
- pain in the groin area;
- vulvitis;
- failure of the menstrual cycle;
- the presence of plaque on the mucous membranes.
Features of the pathogen
The causative agent of candidiasis is a fungus of the genus Candida. There are about 150 species of this microorganism, of which 20 live on human skin and mucous membranes.
Externally, fungi resemble oval cells with spores inside, which are necessary for reproduction.
When placed in a favorable environment, budding and the formation of new colonies begin. The cells stretch out and become like rods. Then they unite with each other and form pseudomycelium. This form of candida is pathogenic.
When exposed to conditions where survival may be difficult, the pathogen forms a dense shell around itself. Thus, vitality is preserved and it is possible to survive an unfavorable environment. This feature affects the survivability of fungi, which can even be found on household items or food.
Diagnostics
Chronic fungal diseases are diagnosed through laboratory tests of biological materials at the time of exacerbation. Using special equipment, Candida colonies are studied. If their integrity is compromised, the diagnosis is confirmed. The results of the study allow us to create an effective treatment regimen.
For laboratory tests, discharge from the lesion, blood, and urine are used. Using serological methods, antibodies to the pathogen are detected. In some cases, a histological examination of the material taken via biopsy is required. For asymptomatic infections, it is possible to analyze the patient's dried urine.
Causes of the disease
The main reason for the development of candidiasis is a decrease in the body's immune defense. Factors contributing to the activation of the fungus:
- diseases of the endocrine system, for example, adrenal or thyroid glands, diabetes mellitus;
- immunodeficiency or HIV infection;
- chronic stress, excessive fatigue;
- hypothermia;
- infectious diseases;
- taking antibiotics, cytostatics, glucocorticosteroids, immunosuppressants, oral contraceptives;
- pregnancy and lactation;
- contraception using an intrauterine device;
- traumatic damage to the skin and mucous membranes;
- wearing underwear made of synthetic fabrics;
- sexually transmitted diseases leading to a decrease in local protective factors.
Effective treatment regimens and drugs
Advanced candidiasis is treated with drugs that do not cause resistance to fungi. Therapy is prescribed after identifying the reasons for the decrease in the body's defenses.
The examination regimen is drawn up individually and depends on the presence of chronic pathologies.
To prevent candidiasis from reoccurring frequently, in addition to antifungal medications, the patient is prescribed physical therapy and medication with an immunomodulatory effect. Stimulation of protective forces allows you to completely suppress the activity of the infectious agent.
Methods of transmission of the disease
- Candidiasis of the genital organs is transmitted from one partner to another, but this is not significant. Fungi of the genus Candida are representatives of normal microflora and live on the mucous membrane of the genital tract of almost every person. The source of infection is often a woman. In men, the fungus is quickly washed away when urinating and washing.
- Sometimes candidiasis is transmitted through household means. The development of infection is possible when using the same hygiene products, towels, bed linen or clothing with the sick person. The risk of getting the disease is not great, but the option still exists.
- If a pregnant woman is sick with candidiasis, then there is a possibility of infection of the baby while passing through the mother's birth canal or in utero.
Illness during pregnancy
The chronic form of thrush often worsens in women during pregnancy. The causes of relapses are serious hormonal changes and decreased immunity. The presence of chronic diseases in a woman is also the reason for the activation of candida, which is contained in small quantities and does not reveal itself in any way before conception. An increased need for minerals and vitamins and their deficiency also lead to immunodeficiency and the development of symptoms of a fungal infection.
During pregnancy, many women experience cravings for sweet foods, smoked meats and marinades. This hobby is a provoking factor that increases the proliferation of candida.
Any type of vaginal infection carries an increased risk for the child. A fungal disease can trigger the spread of candida into the amniotic fluid, causing the development of amnionitis. Activation of chronic infection increases the risk of miscarriage or premature birth.
Candidiasis can cause premature rupture of water and the appearance of a child with underweight.
Fungal disease in pregnant women must be differentiated from helminthiases, bacterial infections of the vagina, and sexually transmitted infections. The laboratory examines a smear taken from the mucous membranes of the cervix and genital organs.
Genital candidiasis: what is it?
Thrush is one of the most common diseases; it occurs regardless of age and gender, but is most often diagnosed in people who are sexually active. It is almost impossible to completely eliminate genital candidiasis.
A patient who has once had it will be forced to regularly undergo preventive treatment.
Fungi that cause disturbances in the body are part of the microflora of the reproductive system. In the body of a healthy person, candida are forced to lead a passive lifestyle, since their activity is regulated by the immune system. The growth of fungal numbers occurs under the influence of external and internal factors, which is facilitated by:
- long-term use of antibiotics;
- changes in hormonal levels during pregnancy, menopause or disorders in the body;
- use of oral contraceptives;
- diseases affecting the immune system, this could be tuberculosis, AIDS or diabetes;
- poor nutrition;
- lack of vitamins in the body;
- nervous system disorder;
- disruption of the gastrointestinal tract;
- climate change;
- use of low-quality underwear.
Based on their prevalence, the following types of genital candidiasis are distinguished:
- Systemic. The external and internal genital organs are affected. It appears in immune deficiency, diabetes and tuberculosis.
- Surface. The external genitalia are exposed to fungi. The disease has a mild course and is often observed in older people.
- Candidal sepsis. The most dangerous form of pathology. Yeast-like fungi enter the bloodstream and begin to spread throughout the body.
Possible complications
If left untreated for a long time, candidiasis of internal organs may develop. Fungi penetrate the bladder, causing inflammation. They can then move up the ureters towards the kidneys, causing kidney damage.
There is also a risk of fungi entering the reproductive organs. The result will be infertility. This complication is typical for both men and women.
In especially severe cases, the pathogen may spread through the bloodstream. A condition called sepsis develops. The disease is treated in a hospital, as there is a possibility of death.
Consequences
Very often, chronic thrush manifests itself with scant symptoms, so patients prefer not to see a doctor or treat themselves. In both cases, this can lead to dangerous damage to internal organs:
- Fungal sepsis is the most dangerous complication.
- Perforations of tissues that cause severe pain.
- Various types of bleeding.
- Ulcers can penetrate into surrounding tissue.
- Women develop infertility.
- Tissue necrosis.
It is very important to comply with the timing of therapy. When treating chronic forms, medications must be taken for six months. But after this you will be able to get rid of the disease forever. To reduce the risk of recurrence of the disease, it is necessary to promptly treat acute illnesses; it is useful to undergo examination for the presence of hidden sexually transmitted infections. It is necessary to wear cotton underwear and keep your skin clean. It is also better to completely abandon the use of perfumed bath products.
Preventive actions
To avoid the development of the disease, you need to follow simple recommendations:
- reduce the amount of carbohydrates consumed;
- regular personal hygiene;
- underwear should be made from natural fabrics;
- If possible, it is better not to wear tight clothes;
- prescribing antifungal drugs for long-term antibiotic therapy;
- restoration of vaginal microflora with probiotics after a course of antibiotics;
- treatment of somatic diseases.
Candidiasis is a disease that is very easily treated. With timely treatment, the disease disappears after 2 weeks, and complications do not develop.
Read
Also:
- Can thrush lead to infertility in women and men?
- Systemic candidiasis - leads to death
- Treatment of candidiasis: thrush in the first trimester of pregnancy
- Treatment of urogenital candidiasis
- Candidiasis urethritis in women, treatment of genitourinary candidiasis
- Treatment and symptoms of genital herpes, what does herpes look like on the labia
Symptoms
We have figured out what could be the cause of cervical erosion and thrush, but now it’s worth understanding how these pathological processes can manifest themselves. It is worth considering that they can be accompanied by completely different signs that you need to be able to distinguish.
| Symptoms of thrush | Symptoms of erosive lesions of the mucous membrane |
| A clear sign is a cheesy, white discharge. | The appearance of bleeding that is not associated with menstruation |
| A woman may experience itching and burning in the vaginal area | Presence of mucous discharge mixed with pus |
| During urination and sexual intercourse, there is a discharge and the appearance of pain. | After sexual intercourse there is a discharge with bloody impurities |
| Presence of a specific odor |
If you notice symptoms of thrush or cervical erosion, you should immediately consult a doctor. The specialist will be able to conduct an adequate examination, on the basis of which he will prescribe the appropriate treatment.