Oophoritis is an ovarian disease of an infectious-inflammatory nature. It is the most common among other pathologies of the female reproductive system and, in the absence of qualified treatment, can cause infertility. It mainly affects women of reproductive age, but can occur at an earlier or later age. Next, we will consider the specifics of the disease, treatment of oophoritis, drugs and antibiotics to quickly relieve the inflammatory process.
Salpingitis and oophoritis: what is it?
Salpingitis and oophoritis are inflammatory diseases. They often occur in the same context, since in most cases they appear against the background of each other.
Salpingitis is an inflammation of the fallopian tubes. Oophoritis is inflammation of the ovary. Often the disease begins with one pathology, and after a while another appears. Therefore, in medicine there is a separate diagnosis “adnexitis”, which indicates inflammation of the oviducts and ovaries at the same time.
Salpingitis and oophoritis are usually detected in women of childbearing age and often result from unprotected sexual intercourse. Therefore, the main method of prevention is sexual education of girls at the stage of puberty.
Salpingitis has different forms of progression and is classified according to several indicators. The treatment method and prognosis of the disease depend on this. The main danger of the pathology is that over time, inflammation of the fallopian tubes leads to the development of adhesive disease with all the ensuing consequences. Patients after prolonged salpingitis often remain infertile, suffer from chronic pain in the pelvis and experience relapses of the inflammatory process.
Diagnostics
It can be difficult to identify oophoritis in a patient the first time, since the main signs of oophoritis, pain in the lower abdomen and temperature can be symptoms of abdominal diseases. To diagnose oophoritis, a gynecological examination of the patient is performed and an analysis is taken to check the vaginal microflora. An ultrasound examination of the ovaries is also prescribed, which can show changes that have occurred inside them. But in the case of an acute form of the disease, this type of research becomes inaccurate.
The main method for diagnosing oophoritis is laparoscopy. Using an endoscope, you can look at the ovarian tissue and determine the stage of the inflammatory process. Additionally, patients are prescribed an endocrinological examination and, together with the doctor, an ovulation diary is compiled.
Classification
Salpingitis and oophoritis are divided into left-sided, right-sided or bilateral . In other words, the inflammatory process develops in the appendages on the left, right or both sides. There are rare cases where left-sided oophoritis and right-sided salpingitis are detected, or vice versa.
According to the nature of the flow, they are distinguished:
- Acute salpingitis. The disease is characterized by an abrupt onset with a pronounced clinical picture. With the right treatment regimen, the prognosis is favorable. Acute salpingitis usually lasts no more than one week and ends with complete recovery without adverse consequences.
- Chronic salpingitis. Pathology becomes the result of an untreated acute form or develops due to an incorrectly chosen therapeutic regimen. Chronic salpingitis has a long course (more than 3 weeks) and practically does not manifest itself. The disease has relapses and often leads to complications.
Depending on the causative agent of the inflammatory process, acute salpingitis has the following forms:
- Non-specific. The cause of the pathology is microorganisms that are normally present in a woman’s body. They are part of the intimate microflora, but should not be in the fallopian tubes and ovaries. For some reason, they penetrate the appendages and provoke inflammation.
- Specific. The disease develops as a result of infections caused by pathogenic microorganisms. They can enter a woman’s body during sexual intercourse, as well as become the result of diseases of other organs and penetrate the appendages through the blood or lymph flow.
Treatment
The course is compiled individually, taking into account the identified etiology of the disease, concomitant pathologies, as well as other features of the case.
We list the main methods of combating ovarian inflammation.
- Drug therapy: antibiotics, the spectrum of action of which includes the identified pathogens; anti-inflammatory vaginal suppositories, douching; absorbable drugs for the elimination and prevention of adhesions.
- Physiotherapy: anti-inflammatory, restorative.
- Mud and hydrotherapy.
- If suppuration develops, the pus from the ovaries is removed promptly, usually laparoscopically.
Causes of the disease
Salpingitis in 70% of cases is caused by an association of microorganisms. They can be either specific or nonspecific. Less commonly, inflammation of the appendages is caused by a single agent.
Salpingitis is caused by:
- streptococci;
- enterococci;
- chlamydia;
- gardnerella;
- E. coli and others.
It is impossible to say for sure why the pathogens of the inflammatory process penetrated the fallopian tubes and ovaries. Most often, salpingitis and oophoritis lead to:
- frequent change of sexual partners;
- refusal to use barrier contraceptives;
- failure to maintain intimate hygiene;
- practice of non-traditional methods of sexual intercourse;
- instrumental interventions in the functioning of the genital organs;
- installation of an intrauterine contraceptive device;
- childbirth;
- carrying out gynecological manipulations without observing the rules of asepsis.
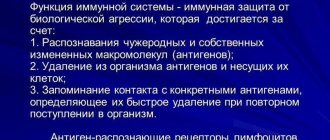
The risk of salpingitis increases in patients with reduced immunity. Frequent colds, taking certain medications, bad habits, and unhealthy diet lead to suppression of the body's resistance.
Is it possible to get pregnant?
Even with unstable ovarian function, pregnancy is possible, but doctors do not recommend planning conception during illness. Against the background of the inflammatory process, there is a high probability of an unfavorable course of pregnancy.
The right thing to do is to be patient, undergo a full course of treatment and rehabilitation, and then think about motherhood.
Read more about the treatment of bilateral oophoritis
To make an appointment or get advice, call the 24-hour number
+7
or fill out the form
Symptoms of salpingitis and oophoritis in women
Inflammation of the appendages in a woman begins with a pronounced clinical picture. Acute salpingitis develops over 5-7 days and, if left untreated, becomes chronic. In the initial stages, the disease seriously worsens the patient’s well-being and forces her to seek medical help.
If a woman ignores severe symptoms or tries to cope with them at home, then by the second week chronic salpingitis occurs. In this case, the severity of the symptoms decreases, the disturbing signs disappear and only mild discomfort remains.
Characteristic symptoms of salpingitis and oophoritis:
- shooting pain on the left or right in the lower abdomen (depending on the location of the disease);
- discomfort during sexual intercourse and gynecological examination;
- increased body temperature;
- discharge from the genital tract (abundant, foamy, with an unpleasant odor, colored).
Inflammation of the appendages can lead to menstrual irregularities and heavy bleeding. Over time, adhesive disease develops, which leads to obstruction of the fallopian tubes, anovulatory cycles and other problems, culminating in infertility.
Treatment of complications of oophoritis
If a purulent tumor occurs, drug therapy is not enough. Even a combination of strong antibacterial agents will not be able to remove the focus of suppuration, so it is necessary to combine surgical and medicinal treatment:
- first, the doctor will prescribe a powerful antibiotic or a combination of two drugs with antimicrobial action;
- then surgery is performed (laparoscopic or open tumor removal);
- the course of antibiotics lasts at least 2 weeks.
The main criteria for stopping treatment with antimicrobial agents are:
- improvement of general condition;
- normalization of body temperature;
- no abdominal pain;
- positive changes on ultrasound.
Diagnosis of inflammation of the appendages in women
Salpingitis is quite easy to diagnose. The gynecologist may suspect inflammation of the appendages during the initial appointment, when he hears about the symptoms from the patient. An ultrasound is prescribed to confirm the diagnosis. Normally, the fallopian tubes are so large that they cannot be seen on an ultrasound. If the oviducts are visualized during the scan, then we are talking about inflammation. Sometimes a concomitant disease is hydrosalpinx, in which fluid accumulates in the pipe.
Inflammation of the ovaries is also determined during ultrasound. Oophoritis is characterized by an increase in the diameter of the female reproductive glands. To determine the cause of the disease, a woman is prescribed a laboratory blood test and vaginal smears.
, it is important to perform an antibiotic sensitivity test to determine the causes of inflammation . Only in this case can effective treatment be prescribed.
Principles of therapy
When selecting medications for the treatment of inflammation in the ovary, it is important to consider the following factors:
- effectiveness of the drug;
- course duration required for cure;
- frequency of taking the drug;
- dosage of the drug;
- number of medications used;
- drug compatibility;
- option of use (tablets, vaginal or rectal suppositories, injections);
- contraindications for each medicine used.
The doctor always takes into account all these factors, giving the woman clear instructions for the treatment of chronic oophoritis. In the acute version of the disease, therapy is carried out in a gynecological hospital, when a course of antibiotics in the form of injections is optimal and effective.
In case of moderate exacerbation or chronic form of the disease, treatment is carried out in a clinic, when a doctor prescribes therapy and monitors the result of treatment.
Chronic and acute salpingitis: treatment
Acute salpingitis is treated with antibiotics and antiprotozoal agents. It is important to identify the disease in a woman at the initial stages so that it does not become chronic. Acute salpingitis, with the correct treatment method, can be easily corrected and ends with recovery after 7-14 days of therapy. Chronic salpingitis requires more serious treatment, which is not always effective.
To treat inflammation of the appendages in women, a pathogen sensitivity test is performed. Drugs that are effective in a particular case are prescribed. An individual list of medications is selected for each patient. Broad-spectrum antibiotics for oral and injection use are usually used, as well as topical suppositories with antiseptic and antibacterial effects. In addition, when using antibiotics, antifungal agents are prescribed.
For the treatment of chronic salpingitis, in addition to antibiotics, auxiliary drugs are selected. The use of proteolytic drugs, painkillers, anti-inflammatory and antispasmodics is recommended.
In the acute period, the patient is prescribed symptomatic medications that alleviate general well-being. They are selected according to symptoms. After treatment, especially for chronic salpingitis, physiotherapy is recommended to prevent adhesive disease, for example, in the gynecological department of the LC on Timur Frunze.
Directions of treatment
When treating oophoritis, it is necessary to adhere to an integrated approach. This is important in order to prevent the disease from becoming chronic, and if it already exists in the patient’s history, to prevent exacerbations.
Antibiotics
The main direction in the treatment of oophoritis is antibiotics. They differ in pharmacological groups, scope of action, side effects and other criteria.
A specific drug is prescribed only after tests have been carried out to determine the type of pathogen (bacterial culture, smears for flora). Despite the fact that most modern antibiotics have a complex effect and several types of microorganisms are sensitive to them, a gynecologist can prescribe two drugs at the same time.
The most effective for oophoritis are cephalosporins and penicillins. Tetracyclines are sometimes used, but they have a lot of side effects and are therefore used extremely rarely, in emergency cases.
Metronidazole is almost always used to eliminate the inflammatory process in the ovaries and/or appendages. It is prescribed simultaneously with drugs such as Clindacin, Gentamicin, Unidox Solutab, Hemomycin, etc. An improved analogue of Metronidazole is Trichopolum. It is easier to tolerate by the body and does not cause nausea or loss of appetite.
Antibacterial drugs are used in the form of tablets, injections, and local drugs are also prescribed - vaginal suppositories. Several forms can be combined at once.
Features of the use of various forms of antibiotics
| No. | Candles | Injections | Pills |
| Efficiency | They have an antibacterial effect at the local level. Used in combination with other forms of medications | High efficiency due to rapid absorption into the blood | Highly effective, but the effect takes a little longer than injections |
| Difficulty of application | Candles are easy to use, usually used once a day, at night. | Require special skills, it is difficult to give an injection without outside help | Easy to use, but you need to drink them 2-3 times a day |
| Price | Varies depending on the drug and the active substance, not the release form | ||
| Side effect | It also depends not on the form of release, but on the specific drug. But suppositories can cause itching and burning in the vagina | ||
| Effect on the gastrointestinal tract | Absent | Absent | May irritate the mucous membranes of the stomach |
After treatment with antibiotics, the balance of the natural microflora of the intestine and vagina is disrupted, and this happens not only after vaginal suppositories, but also after other forms of drugs. To restore the microflora, you can use products with lactobacilli - Bifidumbacterin, Bifiform, Linex, Acylact, etc.
Antibiotics are prescribed without fail; without them, inflammation cannot be stopped. In case of chronic oophoritis, they are used only during periods of exacerbation, and even then not always. Recently, some doctors have been inclined to believe that a long course of oophoritis causes pathogen resistance to antibiotics, therefore it is preferable to treat this disease with other methods.
Prevention of inflammation of the appendages
Prevention of salpingitis and oophoritis should be carried out throughout life. Even before puberty, it is important to organize sex education for the girl, teach her personal hygiene and other natural rules of protection against genital tract infections.
To reduce the risk of salpingitis, it is recommended:
- do not start sexual activity early;
- use barrier contraceptives with new partners;
- have unprotected sexual contact only with a trusted man;
- take a responsible approach to any gynecological manipulations and carry them out only in certified medical institutions, which include the GMS clinic;
- lead a healthy lifestyle;
- Visit a gynecologist regularly and get tested even if there are no complaints.
Russian doctor
Modern methods of treatment of salpingitis and oophoritis Standards for the treatment of salpingitis and oophoritis Protocols for the treatment of salpingitis and oophoritisSalpingitis and oophoritis
Profile:
obstetrics and gynecology.
Stage:
hospital.
The purpose of the stage:
stopping the inflammatory process.
Duration of treatment:
10 days.
ICD code:
N70 Salpingitis and oophoritis N70.0 Acute salpingitis and oophoritis N70.1 Chronic salpingitis and oophoritis N70.9 Salpingitis and oophoritis, unspecified.
Definition:
Salpingitis and oophoritis are inflammatory diseases of the uterine appendages (tubes, ovaries).
Classification:
According to the course: • Acute • Subacute • Chronic Risk factors: • any intrauterine interventions, such as the introduction of intrauterine devices, • surgical termination of pregnancy; • several sexual partners; • sex without barrier methods of contraception and during menstruation; • inflammatory diseases of the female genital organs suffered in the past • (there remains a possibility of persistence of a chronic inflammatory process with previously undetected “hidden” infections and the development of vaginal dysbiosis); • hypothermia.
Admission:
planned, emergency.
Indications for planned and emergency hospitalization:
• The patient is young and has no children. • Doubts about the diagnosis. • Severe feverish reaction. • Tuboovarian abscess. • Impossibility of organizing outpatient treatment or its insufficient effectiveness. • In case of an acute process, emergency hospitalization.
The required scope of examinations before planned hospitalization:
• Serological screening for syphilis • General blood test (6 parameters) • General urine test • Determination of RCG (for differential diagnosis) • Examination of native smears from the vaginal vault, urethra, cervical canal. • Abdominal or transvaginal ultrasound of the uterus and adnexa helps in diagnosing adnexal masses, normal or ectopic pregnancy, especially if severe pain interferes with bimanual examination of the pelvic organs. Using ultrasound data, one can judge the dynamics of the disease and the effectiveness of the therapy.
Diagnostic criteria:
- Bilateral pain in the lower abdomen. — Pathological discharge from the genital tract. - Fever.
The severity of clinical manifestations varies among patients, and the disease may even be asymptomatic. Objective data:
- Pain in the cervix and body of the uterus. — An increase in the size of the ovary or the definition of a tubo-ovarian formation and its painfulness.
Laboratory research:
— Determination of the concentration of C-reactive protein in the blood (increased). — General urine analysis (for differential diagnosis). — Complete blood count (increased ESR, leukocytosis).
Differential diagnosis:
- Acute appendicitis. - Ectopic pregnancy. - Ovarian cyst. - Endometriosis. - Urinary tract infection.
Diagnostic principles:
1. History (complaints) - Bilateral pain in the lower abdomen. — Pathological discharge from the genital tract. — Dysfunctional uterine bleeding. - Fever.
2. Objective data: - Pain in the cervix and body of the uterus. — An increase in the size of the ovary or the definition of a tubo-ovarian formation and its painfulness. — With the development of perihepatitis, pain is detected in the upper abdomen on the right. — Mucopurulent discharge from the genital tract.
List of main diagnostic measures:
1. Determination of the concentration of C-reactive protein in the blood 2. General urine test 3. Determination of hCG 4. Tests for chlamydial and gonorrheal infections 5. Papanicolaou smear 6. Smear for purity 7. General blood test 8. LBC culture from the cervical canal sensitivity to antibiotics 9. 3-hour thermometry.
List of additional diagnostic measures:
1. ECG 2. Coagulogram 3. Blood biochemistry 4. Laparoscopy 5. Ultrasound of the pelvic organs 6. HbsAg 7. Anti HCV.
Treatment tactics:
1. Antibacterial therapy. Broad-spectrum antibiotics are used, taking into account antibiotic sensitivity. 3-4 generation cephalosporins in combination with broad-spectrum tetracycline or macrolides and metronidazole. Alternative drugs: fluoroquinolones in combination with metronidazole and broad-spectrum tetracycline.
Parenteral administration is used until clinical improvement and continues for another 48 hours, then switched to oral administration. Duration is at least 7 days, in severe forms up to 14 days.
2. Desensitizing therapy. 3. Infusion therapy. 4. Prevention and treatment of mycoses. 5. The IUD should be removed. 6. All sexual partners of the patient must be examined and, if necessary, treatment prescribed. 7. For the treatment and prevention of mycosis during long-term massive antibiotic therapy, itraconazole oral solution 200 mg 2 times a day for 7 days.
List of essential medications:
1. Cephalosporins 3-4 generations, macrolides, fluoroquinolones taking into account sensitivity to antibiotics, amp., table. 2. Doxycycline 100 mg, caps 3. Metronidazole 100 ml, vial 4. Metronidazole 250 mg, table 5. Itraconazole oral solution 150 ml - 10 mg/ml 6. Itraconazole 100 mg, caps 7. Dextran solution for infusion in a 200 ml vial, 400 ml 8. Glucose solution for infusion, bottle 400 ml 9. Crystalloid solutions bottle 400 mg 10. Ascorbic acid solution for injection 5%, 10% in ampoule 2 ml, 5 ml 11. Fluconazole, caps 150 mg.
Criteria for transfer to the next stage of treatment:
disappearance of pain, normalization of temperature and menstrual cycle, normalization of laboratory parameters and vaginal data.