Successful conception and pregnancy do not always lead to the desired result - the birth of a new person. The notorious natural selection dictates its conditions. Not all mothers carry their children to 38-40 weeks healthy and ready to see the world. Some people are really unlucky. For some, due to a number of circumstances, while others, due to inexperience or ignorance, make unforgivable mistakes even at the stage of pregnancy planning.
Unfortunately, the outcome of the pregnant woman and the fetus is not always positive. Pregnancy may result in arrest of embryo development at the initial stage or death of the fetus in the second decade of pregnancy. Why does this happen, why is it dangerous and most importantly – what is histology after diagnosing a frozen pregnancy and what is it needed for? More on this below.
Why pregnancy freezes
According to statistics, the majority of missed pregnancies occur in the first trimester. To be more precise, the problem especially often makes itself felt in the period from 4 to 8 weeks. Detecting pathology at such an early stage is not easy even for experienced doctors. The matter is complicated by the possible asymptomatic course of a frozen pregnancy, when the expectant mother cannot focus on the activity of the baby.
***
It is possible to make a diagnosis of “frozen pregnancy” in the early stages only after an ultrasound examination. The first ultrasound is scheduled as soon as the pregnant woman is registered. The procedure is repeated at 7-8 weeks, or if there are complaints from the patient.
The sooner it is possible to identify pathology during fading pregnancy, the greater the chance of removing the fertilized egg or fetus before it begins to poison the woman’s body. Delay in diagnosis can cause disseminated intravascular coagulation syndrome, which implies severe complications in the body's ability to clot blood. Moreover, if you miss the pathology and do not prescribe a cleaning or medical abortion on time, saving the woman’s life may be in question.
Every expectant mother should be responsible and be especially vigilant at the slightest signals from the body indicating a malfunction. Getting pregnant again after treatment for a frozen pregnancy is more than possible, but not everyone will be able to survive and recover from severe intoxication.
Signs of fetal freezing
In the very early stages of pregnancy, pathology makes itself almost invisible. The expectant mother experiences mild symptoms of toxicosis, breast swelling, and mood changes. Only after a while the symptoms of pregnancy will begin to subside little by little, giving way to pain and bleeding. The latter indicate the beginning of the process of detachment of the fertilized egg and the risk of miscarriage.
A week or two after pregnancy fading, the symptoms of toxicosis will disappear completely, the breasts will become soft and stop hurting, and the basal temperature will drop. All these are signs of fading pregnancy, which a woman can and should pay attention to even before visiting a doctor. At later stages, after the 16th week, when the baby is already making itself felt with kicks and movements, his tragic death is indicated by silence with the absence of any activity inside the womb.
***
In addition to the obvious visual signs of a frozen pregnancy, which a woman may not pay attention to, the problem can be learned from the test results. The supervising doctor should prescribe a blood test for the level of the hCG hormone and an ultrasound.
If the fetus does not develop, the hCG level will be significantly lower than normal. Using ultrasound equipment, the doctor will be able to determine the absence of the baby's heartbeat. Pathology can also be detected during a routine gynecological examination - the size of the uterus will not correspond to the duration of pregnancy.
To eliminate the problem in cases of asymptomatic frozen pregnancy, women are advised to register as early as possible and not miss routine examinations with doctors.
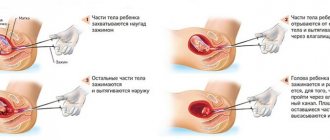
The diagnosis of “frozen pregnancy” leaves no hope for further pregnancy and childbirth. The baby inside the womb has died and must be removed from the uterine cavity as quickly as possible before the decaying tissue enters the mother's bloodstream. Depending on the duration of the frozen pregnancy, the doctor prescribes a method of treatment. It could be:
- medicinal method (the patient is asked to take pills that provoke uterine contractions for arbitrary miscarriage, prescribed for up to 5 weeks);
- surgical intervention with curettage during a frozen pregnancy;
- vacuum cleaning.
In extremely rare cases, when the pregnant woman’s body’s reactions allow it to wait, the doctor decides to give the body the opportunity to independently get rid of the dead embryo. During this period, the woman is under strict supervision to avoid the development of complications.
***
Why is pathology dangerous?
A stop in the development of the embryo and the death of the fetus in the later stages is a moral and physical test for a failed mother. In any of the options, the problem is solved by removing the embryo from the uterine cavity. The degree of risk and consequences depend on the period at which the pathology was discovered and the cleaning method.
For example, curettage can lead to uterine bleeding with the appearance of infections and the subsequent development of adhesions. All these are real problems that can prevent you from getting pregnant in the future.
Quite often, cleaning a frozen pregnancy leads to disruption of the intestinal microflora due to serious antibacterial therapy and surgery.
Website about pregnancy, childbirth and raising a child
Carrying a baby is a difficult but happy period in a woman’s life. Unfortunately, pregnancy does not always end with the birth of a child. Due to certain factors, the fetus dies in the womb. This is called a missed abortion (a miscarriage that has not yet occurred).
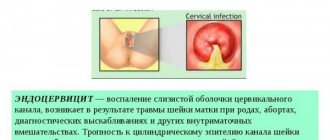
To determine its cause, a special examination of the tissues of a dead embryo through a microscope is used, which is called histology after a frozen pregnancy. It is performed when the embryo is scraped out of the uterus. The content of the article:
Histology of fetal freezing
Histology is one of those right steps that need to be taken after a frozen pregnancy on the path to correcting mistakes and a healthy pregnancy. We are talking about studying an aborted embryo to identify the reason for its death. The procedure is called histology and is prescribed to prevent the causes that caused the development of pathology in the future.
***
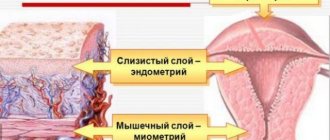
The remains of the fertilized egg or embryo during a frozen pregnancy, along with the endometrial layer, are sent for examination to a special laboratory. Histologists call the main causes of fetal death:
- sexually transmitted infections gonorrhea, syphilis, etc.;
- common viral diseases;
- hormonal disorders;
- abnormal structures of the uterus;
- genetic problems.
Based on the results of histology, after cleaning a frozen pregnancy, the doctor develops a treatment and rehabilitation plan for subsequent healthy conception and pregnancy in the future. A biopath examination does not always provide an opportunity to obtain accurate results about the reasons for the arrest of embryo development, so the woman may additionally be prescribed a comprehensive examination.
What it is?
If it is too late to detect a pregnancy that has stopped developing, this poses a danger to the woman’s health. A frozen fetus begins to decompose and can cause serious complications, including death.
Histology after curettage of a frozen pregnancy will help to find out the cause of what happened. This analysis involves microscopic examination of tissue from a frozen fetus.
Carrying out the research procedure
Doctors independently send embryo samples obtained as a result of curettage or vacuum suction to the laboratory for analysis. There, the material is prepared for detailed study, and microscopy of the endometrium provided is performed. The procedure for histological examination of a frozen pregnancy takes place in several stages:
- The tissue fragments are secured and treated with a solution to stop the decomposition process. In this way, histologists extend the life of the tissue for possible re-examination.
- The tissue sample is dehydrated for compaction purposes.
- The material is filled with paraffin to form an even cut.
- The solid biopath is cut into thin pieces.
- Samples are placed on a glass slide and coated with a reagent to identify cell structures.
- The final stage is storing the sample between two glass slides.
Experts conduct the study using a modern powerful microscope, after which they issue a conclusion. The entire process from preparing and studying the sample to the histologist’s conclusion takes on average about 10 days.
As a result of comprehensive work, histologists identify possible genetic problems that provoked the fading of pregnancy, or diseases of the woman’s reproductive system that did not allow her to carry a child to term.
***
Essence and stages of research
In order to conduct histological studies, a piece of tissue (small) is taken, a smear, a print or a small section from the organ that is being examined is enough. The test period usually varies from five to ten days; in rare cases where urgent results are needed, a rapid test can be done within twenty-four hours.
But such research is not always accurate. Research is carried out in seven stages:
- fixation. Tissue fragments are treated with a special composition in order to prevent the breakdown of cells and structure. This is done so that the material does not deteriorate during study;
- wiring. The materials are degreased so that they become compacted;
- filling. Impregnated with paraffin to prepare a hard cut;
- cutting. Using a microtome, the hardened material is cut into thin layers;
- coloring. These layers are placed on special glasses, stained with a special composition to determine different tissue structures (DNA, RNA, cytoplasm, etc.);
- conclusion. Sections on glass are covered with another glass on top to preserve the layers;
- study. The obtained samples are studied by histologists or pathomorphologists using a light microscope.
They are directly involved in deciphering the histology results if a frozen pregnancy, miscarriage, etc. occurs. Why does my left side ache during pregnancy?
In gynecology, histology is prescribed to study the fetus. Such a pregnancy is the same as a miscarriage that has not yet occurred. After determining the death of the fetus, cleansing is prescribed so that putrefaction does not begin in the woman’s body.
The material is cut directly from the uterus. You cannot have sexual intercourse within 24 hours. Everything is done under sterile conditions, local anesthesia is given, and a piece of flesh is taken for analysis. The material is sent to the pathology laboratory and examined there. If abnormalities are detected, treatment is prescribed.
What the results say
Can determine the origins of the disease
The extracted matter (placenta) is always sent for histology. Histology is carried out along with tests for infections, hormones, etc. This allows you to accurately determine the cause of the incident. This is necessary to avoid a repetition of the situation.
Gynecologists prescribe histology for inflammatory processes in the uterine cavity, neoplasms on it, after curettage, and during a frozen pregnancy. If multiple ovarian cysts are present.
It also helps to identify cancer at an early stage. Histology is also prescribed:
- with prolonged bleeding;
- pain in the lower abdomen that appears for no particular reason;
- leukoplakia;
- uneven surface of the organ;
- painful menstruation;
- for infertility;
- irregular periods;
- neoplasms on organs, etc.
The cost of such an analysis
- the quality of the material that was examined;
- quality of diagnostic equipment and qualifications of laboratory staff;
- qualifications and experience of pathomorphologists.
The price of histological analysis is from 2 to 3 thousand rubles
The cost of such a procedure ranges from two to three thousand rubles. Decoding and description is about five hundred rubles. Re-examination of glass costs about two thousand rubles. Immunohistochemistry costs approximately three to five thousand rubles.
After you have received the results of histology, which was carried out after a frozen pregnancy, each woman must undergo certain examinations:
- to identify TORCH infections, it is necessary to undergo examination a few days after curettage (no later), otherwise there will be no accurate result;
- undergo an examination to determine the level of hormones - progesterone, estradiol, thyroid hormone;
- undergo a pelvic ultrasound several times during one menstrual cycle;
- do an immunogram, immunological examinations, yourself and do the same for your spouse (partner);
- it is necessary to undergo a biocenosis study, sowing the flora of discharge from the genital organs. Determine sensitivity to the main spectrum of antibiotics, bacteriophages;
- identify infections that can be sexually transmitted;
- identify hemostasis indicators Fibrinogen, Prothrombin, Thrombin time, APTT, Antithrombin 3, Lupus anticoagulant;
- identify genetic risks in case of repeat pregnancy;
- determine blood clotting.
Of course, an accurate examination is prescribed by the attending physician. He takes into account the specifics of your case and prescribes the course that you need to take. This is usually from three to six months. You should not plan pregnancy for this period.
Partners, after they have received the results of your histology after a frozen pregnancy, need to carefully monitor their health, lead a healthy lifestyle, and eliminate bad habits and stressful situations. Spend more time outdoors and play sports. A woman needs to avoid heavy exercise, get more rest and eat right.
About the author : Borovikova Olga
What the results show: correct decoding
At the end of the study, histologists prepare a special standard sample form in which the conclusion is written. For patients without special education, terms in Latin do not mean anything, so it will not be possible to decipher the conclusion without the help of a doctor. The form with the results of the study should be shown to the observing obstetrician-gynecologist and under no circumstances should you try to independently search for answers on the Internet, once again causing stress.
In most cases, based on the results of histology, it becomes clear that the child did not survive as a result of genetic abnormalities. At the moment of conception or some time after it, a genetic failure occurred that provoked the fading of the pregnancy. Even healthy couples who carefully plan their pregnancy are not immune from this.
Less commonly, but still there is a hereditary genetic problem that can cause pregnancy to fail again.
Histologists do not rule out DIC syndrome, a disease associated with a violation of the blood clotting process, which can cause a stop in the development of the embryo and even cause the death of the woman herself.
In other rare cases, in the transcript of the study, experts indicate the diseases and pathologies that provoked the problem. If necessary, the woman is prescribed a comprehensive examination, which allows the cause of freezing to be determined as accurately as possible.
Measures after identifying the cause and research: how to eliminate mistakes in the future
Treatment and rehabilitation methods for subsequent healthy conception and bearing a healthy child will depend on the results of the research. In cases where the provided material could not provide an accurate answer, additional diagnostic procedures are prescribed:
- Analysis of the hormonal panel of the endocrine and reproductive systems (examining the level of progesterone, estradiol, cortisol, prolactin, LH, FSH, T4 and TSH).
- Analysis for TORCH infections. Carry out a few days after cleaning to obtain the most accurate result. An exacerbation of TORCH infection during pregnancy can be detected only if you do not delay the analysis.
- Ultrasound of the genital organs with examination of the functioning of the adrenal glands and thyroid glands, which play an important role in the production of hormones necessary for the normal development of the child.
- Immunogram of the couple. The study allows you to identify or exclude the immune factor of fetal death at an early stage.
- Genetic research of the couple to exclude recurrence of the situation in a future pregnancy.
- Spermogram with a visit to the urologist. Assigned to the child's father to identify possible anomalies.
- Repeated histology to exclude specialist errors. Conducted in an alternative laboratory.
- Examination of the vagina to identify microflora with additional PCR diagnostics.
- Complete blood work to obtain aPTT, lupus anticoagulant and fibrinogen hemostasis.
The blood of the expectant mother is additionally checked for the degree of coagulation to exclude disseminated intravascular coagulation syndrome. Based on the results of the tests and on the basis of the histologists’ interpretation, the woman is prescribed adequate treatment for the recovery period (at least six months), recommending protection during the entire rehabilitation period. After completing the course of treatment, the couple takes tests again and proceeds to planning a pregnancy.
What can histology results indicate?
Histology allows not only to identify the cause, but also to correctly navigate the treatment. Such an analysis most often reveals the following provoking factors for miscarriage:
- Sexually transmitted infections.
- Diabetes.
- Rubella, hepatitis and other viral diseases.
- Hormonal imbalances in a woman’s body.
- Deviations in the functioning of the organs of the reproductive system.
- Defects in the development of the uterus.
By analyzing a piece of tissue, you can identify signs of an inflammatory process. By examining the endometrium, it is possible to detect abnormalities in the structure of the tissues of the embryo, which may indicate chromosomal changes in the fetus.
Only a competent specialist can decipher the pathologist’s conclusion; it is difficult to do this on your own. It is necessary to have an idea of what a normal endometrium should look like during pregnancy.
After the fertilized egg is implanted into the endometrium, changes begin that will ensure the proper development of the fetus. The number of fibroblast cells that will synthesize protein molecules increases sharply. In histological examination, this area should allow the placenta to form. There are also trophoblast cells that provide nutrition to the fetus in the early stages of development.
If, in the process of histological analysis, abnormalities are detected in trophoblasts and fibroblasts, then we can say that the development of the fetus was disrupted at the initial stage, so it was not able to fix itself normally in the uterine cavity.
Problems may appear in the blood vessels; if their restructuring does not correspond to the period of pregnancy, this can cause miscarriage or fetal death. If it is possible to preserve it, then there is a high probability of developing gestosis.
Histologists call this condition hydatidiform mole. The condition is dangerous due to heavy bleeding and severe toxicosis, but the fetus most often dies in the early stages. Trophoblast tissue develops in the uterine cavity. Among the reasons for this condition, histologists name:
- Chromosomal disorders.
- Impact of viruses.
- Numerous pregnancy terminations.
- The expectant mother is too young or already over 35.
But most often, histology alone is not enough. After analyzing the results, the attending doctor refers the woman to other examinations:
- Determination of the level of sex hormones and thyroid gland.
- Detection of TORCH infections. But such an analysis is most reliable in a short time after curettage.
- Immunological tests. It is advisable that they be completed by both partners.
- During the cycle, an ultrasound examination is prescribed twice, which helps to detect diseases of the pelvic organs.
- The man is sent for a spermogram and subsequent consultation with a urologist.
After interpreting the results of all studies, the doctor selects a course of therapy. A woman needs to prepare herself for long-term treatment, which can last up to six months.
During the period of therapy, the doctor does not recommend that the woman become pregnant again until the causes of the missed abortion are eliminated, since there is a high risk of recurrence.
About the chances of giving birth after a frozen pregnancy
The chances of successfully conceiving, bearing and giving birth to a healthy child will directly depend on the results of histological tests and a comprehensive study of both parents. In some cases, treatment helps to start with a clean face with minimal risks. In other rarer cases, the only solution to the problem will be surrogacy.
One way or another, every expectant mother must responsibly approach the moment of planning a pregnancy after the fetus has died, and do everything possible to ensure that the fatal mistake does not happen again.
Decoding
Interpretation of the histology results after curettage is based not only on the conclusion about the structure of the tissues of the embryo, but also on the general history of the woman.
After completion of the study, the results are given to the woman. In conclusion, the following parameters are indicated:
- information about the embryo - period in weeks, date of cessation of development, size, etc.;
- description of fabrics;
- an indication of the presence of deviations in the structures, if any.
A woman will not be able to correctly decipher the results obtained on her own. Therefore, in conclusion, you need to consult a doctor.
The conclusion indicates not only pathologies. During the study, a complete description of the structures being studied is carried out.
Based on the histology results, the doctor can give recommendations on the woman’s further behavior. If there is a need to undergo treatment, they will definitely tell you about it.
As a rule, after a miscarriage or miscarriage, it is necessary to undergo a consultation with a geneticist and be tested for hidden infections. These are the most common causes of pathology.
Histological examination is rarely accompanied by positive emotions on the part of the woman. As a rule, it is carried out against the backdrop of very unpleasant events.
Studying the structural features of tissues can provide an explanation of why developmental arrest or miscarriage occurred, as well as make an assumption about the likelihood of having a sick child.
Based on a medical opinion, a woman will be able to properly prepare for the next pregnancy and give birth to a healthy baby.
If tissue testing is necessary during pregnancy, there is also no need to fear it. Possible risks during the procedure are small.