The metaplastic layer of the cervical epithelium represents normal cells that are located in the area of transformation. In the absence of abnormalities and pathological processes in the metaplastic epithelium, cells of varying degrees of maturity are detected during diagnosis. Experts note islands of columnar epithelium, which has open and closed types of glands, as well as a normal vascular pattern.
The immature stage of metaplastic epithelium indicates pathological processes in the cervix that require careful diagnosis. Metaplasia means a change in the basic properties of the tissue. Cervical metaplasia is diagnosed mainly in patients over 45 years of age. This disease is a precancerous condition, so untimely treatment can lead to serious complications.
Without treatment, healthy cells gradually begin to turn into malignant cells.
It is for this reason that it is important to begin treatment at the initial stage of development. Gynecologists recommend regularly coming for a preventive scheduled examination and doing a screening examination.
Causes
The most likely reasons for the development of cervical metaplasia is the spread of infectious agents. Pathogenic bacteria and viruses act as pathogens. A dangerous viral agent is human papilloma, which penetrates the woman’s genitals. The main danger is that this infection can occur for a long time without symptoms or obvious signs. Another possible agent is herpes, which has a high level of oncogenicity.
After pathogenic bacteria enter the metaplastic epithelium of the cervix, irreversible consequences begin to occur. Women need to be wary of ureaplasma, chlamydia, gonococci, toxoplasma and other microorganisms that penetrate cells and remain in them for a long time. They fight off immune cells and support inflammatory processes.
Rules for obtaining an informative smear for oncocytology
- The doctor must first take a swab and only then conduct a manual examination.
- Before taking a smear, mucous secretions are removed.
- The material on the glass should be distributed neither thick nor thin.
Swabs cannot be given:
- during the period of ovulation, when there is very abundant mucous discharge from the cervix (the so-called mucus plug);
- after a vaginal ultrasound (gel remains on the cervix);
- after sexual intercourse (sperm interfere with the study of cells under a microscope);
- if spermicides or any medications were previously introduced into the vagina;
- during menstruation, shortly before it or when it has not yet completely ended.
The rather complex process of diagnosing infections of the genital organs and genitourinary system most often does not allow the doctor to quickly and promptly prescribe the necessary treatment.
This is especially true for oncological diseases that are asymptomatic. Therefore, women of reproductive age are recommended to take a cytology test at least once a year.
Existing risk factors
There are several common factors that lead to pathological changes in the metaplastic epithelium of the cervix:
- bad habits (alcoholic drinks and smoking);
- poor environmental conditions;
- eating carcinogenic foods.
These factors help reduce the body's reactivity, so women develop functional and morphological changes within organs, as well as entire systems.
Those at greatest risk are women who had early sexual intercourse, frequently changed partners, had abortions, and did not seek help from a gynecologist for hormonal disorders.
What to do if there is proliferation?
If proliferation is detected anywhere, the specialist will first determine its cause and then draw up a management plan for the patient. There is no specific treatment for proliferation as such, because it is not an independent pathology, but a reflection of other diseases. If increased division is caused by inflammation, the doctor will prescribe anti-inflammatory therapy, supplementing it with antibacterial or antiviral agents if necessary.
Precancerous proliferation with atypia against the background of dysplasia may require more radical measures - excision of the affected area. In the case of proliferation against the background of carcinoma, treatment is carried out according to all principles of oncological care, up to organ removal.
Any proliferation indicating pathology serves as an alarming signal, so patients with such changes are always in the doctor’s field of vision. After treatment of the underlying disease, a control cytological examination or biopsy is usually performed to assess the effectiveness of therapy and the risk of tumor transformation in the future.
Author: oncologist, histologist Goldenshlyuger N.I. (OICR, Toronto, Canada)
The author selectively answers adequate questions from readers within his competence and only within the OnkoLib.ru resource. Face-to-face consultations and assistance in organizing treatment are not provided at this time.
People facing the diagnosis for the first time are interested in proliferation of the glandular epithelium, what it is. This pathology is an increase in the concentration of glandular elements in girls, which disrupts the functioning of the reproductive system.
Diseases
Pathological changes in the cervix occur in many women. Cancer is a common and common gynecological disease. Pathological processes are characterized by stages and stages in the development of carcinogenesis. Diseases are divided into several types.
- Background. These are pathologies of the vaginal part of the cervix, during the progression of which the integrity of the metaplastic epithelium, its differentiation, exfoliation and maturation are preserved. Such dangerous diseases include polyps, leukoplakia, papilloma, cervicitis, true erosion, ectropion and endometriosis.
- Precancerous. This group of diseases includes dysplasia of metaplastic epithelium and other pathological processes. They contribute to the development of hyperplasia, proliferation, and impaired differentiation. As a result of such processes, metaplastic epithelial cells mature and are rejected.
To prevent infection from entering the genitals, you need to monitor vaginal hygiene and regularly visit a gynecologist for examination.
Medical terms that scare you
Dystrophy or dystrophic epithelium - occurs with true erosion of the cervix or pseudo-erosion, which is also called ectopia. In a word, when there is a wound on the cervix. When it heals, cell degeneration will no longer be detected.
The medical term “metaplastic” is often present in the cytogram. Many people think that this indicates a malignant process. But no - metaplastic epithelium is a good smear result.
This indicates that the cells were taken exactly from the desired zone - the junction of two types of epithelium - from the endocervix (cylindrical) and exocervix (flat). These are the cells of the transformation zone, where atypia, precancerous or cancerous changes are most often found.
Acetowhite epithelium (ABE) is not an indicator that can be displayed on smears. ABE is visible during extended colposcopy after exposure of the cervix to acetic acid.
If there are pathological areas on it, the epithelium will begin to turn pale. Next, the doctor makes conclusions based on how quickly the whitening occurred, how bright it was, how long it lasted, whether it had boundaries, whether there was a sign of a ridge, etc.
If the reaction was not pronounced, most likely the women have chronic cervicitis (inflammation), HPV or LSIL (mild dysplasia). In case of severe ABE, HSIL is diagnosed - severe dysplasia.
In appearance, the cervix, even with severe dysplasia, can be quite healthy. And only the vinegar test shows what is not visible to the eye.
Not every gynecologist is a good colposcopist. An experienced specialist monitors the cervix during extended colposcopy after treatment with vinegar and iodine, literally without taking his eyes off, and makes very accurate diagnoses.
By the way, in some countries it is the vinegar test, and not the PAP test, that is a screening method for diagnosing precancer. If coarse acetic-white epithelium is detected, the woman is taken under control and treated.
Hyperplastic epithelium is usually synonymous with cervical canal polyp. Needs removal and histological examination.
Cells with signs of keratosis, keratinization - most often these words can be seen in the reports of women with suspected leukoplakia. But the same signs (features of epithelial cells) occur in precancer and cancer.
Pronounced reactive changes are an inflammatory process in the cervix.
Signs of mild dysplasia - lsil. If there are pronounced, deep changes, we are usually talking about HSIL - severe neoplasia, in which surgical intervention is necessary - conization of the cervix.
READ MORE: If a child has an enlarged thyroid gland
Koilocytosis is a feature of epithelial cells most characteristic of PVI (human papillomavirus, HPV). Viral infection.
Reparative changes in the epithelium are benign changes in cells, a variant of reactive changes (see above).
Degenerative changes are not cancer; they occur during a chronic or acute inflammatory process. In the same category, reactive changes include the following concepts: inflammatory atypia, squamous metaplasia, hyperkeratosis, parakeratosis.
Atypia, atypical changes - dysplasia (precancer) or malignant neoplasm.
Atypical squamous epithelial cells of unknown significance - asc-us. These are cells of unknown significance. The cytologist sees that they look unusual, changed, but cannot accurately determine what was the cause - inflammation, dysplasia, infection or irritation.
There is no need to be afraid of this formulation. It does not raise the doctor's suspicion of cancer. However, it is a reason to take smears from the cervix for HPV of high oncogenic risk (required types 16 and 18). And if they are detected, you need to undergo an extended colposcopy.
Proliferation of squamous epithelium - that is, proliferation or in medical terms - mitosis. Normally, this process proceeds slowly. Its purpose is to renew the upper layer of the cervical mucosa. During pregnancy, the process is more active, but normally moderate.
If, according to the results of scraping, proliferation is pronounced, then this happened for one of the following reasons:
- cervicitis (inflammatory process on the cervix);
- tissue trauma resulting from diagnostic curettage, abortion, difficult childbirth, conization;
- tumor growth - benign or malignant (cervical canal polyp, mild or severe dysplasia, cancer, papilloma).
That is, proliferation can be hyperplastic, inflammatory or post-traumatic.
Dyskaryosis is an enlargement of the cell nucleus. The cause is gynecological diseases (colpitis, cervicitis, vaginitis) or dysplasia.
Etiopathogenesis
Disturbances in the metaplastic epithelium of the cervix in most cases lead to patients developing cancer of stratified squamous epithelium.
These processes are associated with the fact that the cells have bipotent properties, and therefore often turn into flat and prismatic epithelium.
There are several ways to develop ectopic columnar epithelium:
- reserve cells are formed on the surface of columnar metaplastic epithelium;
- gradual replacement of erosion of flat metaplastic epithelium, on which there are inflammatory processes or microcracks.
Metaplasia is a process as a result of which reserve cells turn into a flat form of metaplastic epithelium. Squamous metaplasia is characterized by proliferation of reserve cells, which contributes to the development of malignant transformation. The formation of dysplasia or a precancerous condition leads to complete overlap of the cylindrical metaplastic epithelium.
The number of leukocytes in the visual field. to squamous epithelial cells
The number of leukocytes largely depends on the individual characteristics of the body and the day of the menstrual cycle (during the period of ovulation there are more of them), the presence or absence of sexual activity, and possible chronic cervicitis - inflammation of the cervix.
For this reason, doctors do not identify a specific norm for leukocytes. They only look at their ratio to the cells of the vaginal epithelium. The ratio of leukocytes to squamous epithelial cells should be up to 1:1. If the number of leukocytes to squamous epithelial cells increases to a ratio of 2:1, 3:1, 4:1 or more, this indicates an infection, more often candidiasis (thrush) or trichomoniasis. 1:1 is a borderline ratio. This is not necessarily an incipient disease. Perhaps the result was influenced by some chemical or mechanical factor. The same sexual intercourse if it happened a few hours before the smear test. That is, 15-20 leukocytes with 15-20 epithelial cells in the field of view may be a normal variant. This is especially common in pregnant women.
We bring to your attention a table from the guidelines for attending physicians. They can see that the number of leukocytes is greater than the number of epithelial cells in nonspecific vaginitis, candidiasis, and trichomoniasis. But with bacterial vaginosis, on the contrary, it is less.
Cytologists also pay attention to the structure of epithelial cells, their changes, and the ratio of their nucleus to cytoplasm. In disease, the cell nucleus is large. This is explained by the fact that the scraping contains cells from the lower layers of the epithelium. And the reason for this is the active desquamation of the surface epithelium due to an inflammatory reaction.
Proliferation refers to the process of cell division, leading to an increase in tissue volume. The most active proliferation occurs in the embryonic period, when the cells of the developing embryo are continuously and intensively dividing. This process is regulated by hormones and biologically active substances that can both enhance it (growth factors) and weaken it.
Seeing the term “proliferation” in the conclusions of specialists, many immediately try to find the meaning of this word, while at the same time feeling worried about possible troubles, but there is no need to panic: proliferation is not a disease.
The cells of many tissues need constant renewal; this is a natural physiological process realized through division. Cell renewal is especially pronounced in the skin, mucous membranes of the digestive tract, respiratory system, and uterus. That is, proliferation in these tissues is a normal and necessary phenomenon.
On the other hand, excessive cell proliferation cannot be considered normal and acquires pathological features.
Most often, proliferation is a manifestation of the inflammatory process (gastritis, cervicitis), damage (after surgery, trauma), and tumors. Increased proliferation underlies tissue proliferation in neoplasms and hyperplastic processes. Precancerous changes, including dysplasia, are also accompanied by increased cell proliferation.
If, in the case of inflammatory changes or traumatic injuries, proliferation is usually transient in nature and is intended to restore the tissue to normal, then in the case of tumors it takes on a different meaning. In neoplasms, proliferation is not only excessive, but also non-stop, cells divide continuously, leading to the appearance and growth of a tumor. There is no limit to such proliferation, just as there is no limit to cell division in a tumor.
Proliferation is often accompanied by atypia, that is, proliferating cells acquire features that are unusual for them and change in appearance and functionality. Atypia indicates a possible precancerous transformation. The appearance of uncharacteristic features in cells during increased proliferation is not surprising: rapid reproduction creates conditions for genetic mutations, and the cells do not have time to mature properly. In this case, quantity does not mean quality, and sooner or later abnormal, mutated elements appear in a rapidly multiplying clone of cells.
The fact that there is a high probability of atypia during cell proliferation makes this process potentially dangerous, so doctors are wary of it. If the cells have changed their appearance or properties, we can talk about precancer and urgent measures must be taken to eliminate the pathological focus.
cancer development – uncontrolled proliferation with atypia
In the conclusions of morphologists one can find an indication of the severity of proliferation processes. This indicator is quite subjective, because there are no clear criteria to distinguish these degrees. Moreover, in some organs, moderate proliferation may be considered normal, while in others, even a slight increase in cell division is cause for concern. In this regard, patients should not focus too much on the degree, but if we are talking about pathological proliferation, then it is clear that the stronger it is, the worse.
Video: about cell division and cancer development
What are metaplastic epithelial cells?
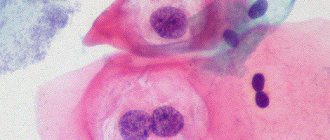
Cells of immature metaplastic epithelium at the time of diagnosis have a parabasal appearance. Chromatin is distributed evenly in a woman’s body. In rare cases, during diagnosis, specialists are able to determine the clearing zone. The cells have clear and even boundaries on one side.
After the cytoplasm matures, it acquires a lighter shade and an oval shape. Metaplastic cells that have matured are no different from squamous epithelium. The invasive form of cancer is a benign pathology. It is diagnosed in many patients who seek help from a doctor. In order for treatment to bring a positive result, it is necessary to start therapy in a timely manner.
Cytological screening will help identify even minor changes and precancerous lesions.
Early forms of cervical cancer can be cured using radiation and surgery. Scientists have repeatedly conducted epidemiological studies, the results of which have shown that pathological changes in the metaplastic epithelium of the cervix begin to develop as a result of early sexual activity, with frequent changes of partners, smoking and drinking alcoholic beverages.
The infection affects the upper layer of metaplastic epithelium of the cervix as a result of the development of condylomas. These are multiple papillary growths that consist of fibrous tissue. Metaplastic multilayered epithelium is formed on its surface. Condylomas are flat, pointed, enlarged and inverting. This pathological disease often occurs without obvious clinical manifestations, so it is important to regularly come for examination and diagnosis to a gynecologist.
Columnar epithelial cells with reactive changes
CYTOLOGY smear is a method of microscopic examination of the cervical epithelium for the purpose of PREVENTION AND EARLY DIAGNOSIS OF CERVICAL CANCER.
A cytology smear primarily performed to detect atypical cells , which allows early diagnosis of dysplasia (CIN, LSIL, HSIL) or cervical cancer.
It is an inexpensive and convenient method for reaching large numbers of women with preventative care.
Of course, the sensitivity of a single study is low, but annual mass screening in developed countries has significantly reduced the mortality rate of women from cervical cancer.
Due to the fact that atypical cells can be located in a relatively small area of the mucosa, it is very important that the material is obtained from the entire surface of the cervix, especially from the cervical canal ! For this purpose, special brushes have been created that make it possible to obtain material from areas inaccessible to inspection.
Particular attention is paid to the transformation zone, the cells of which most often undergo tumor degeneration. It is in the transformation zone that up to 80-90% of cervical cancer develops, the remaining 10-20% occur in the cervical canal.
When to take a smear for cytology? A smear for cytology should be taken starting from the 5th day of the menstrual cycle and 5 days before the expected start of menstruation.
The analysis cannot be carried out within two days after sexual intercourse or insertion of suppositories into the vagina. Failure to follow these rules may lead to erroneous interpretation of the results.
[/attention]
It should be noted that collecting material is a rather unpleasant procedure. The gynecologist must scrape the epithelium from the surface of the cervix and enter the cervical canal. The more epithelium from different zones gets in, the better the diagnosis. Sometimes bruising may remain after cytology, this is considered normal.
Thus, the main significance of a cytology smear is to determine qualitative changes in cells. To determine the infectious agent that caused the inflammation, it is better to use a smear on the flora or bacteriological culture .
However, during a cytological examination, the doctor may note the presence of any microorganisms. Normal microflora includes rods (lactobacillus), single cocci, and in small quantities there may be opportunistic flora.
The presence of specific infectious agents (Trichomonas, amoebas, fungi, gonococci, gardnerella, leptothrix, chlamydia, an abundance of cocci) is considered a pathology that needs to be treated.
Processing of smears. Cytology deadlines
After collecting the material, the sample is transferred to a glass slide, fixed and stained. When directly transferring a smear from a brush, partial loss of material and cell deformation are possible, which leads to a decrease in the sensitivity of the method and a large number of false results. The classical method was replaced by liquid cytology, which significantly increased the accuracy and quality of the study.
Liquid cytology is a new technology for processing smears, which involves placing samples in a container with a special stabilizing solution. In this case, the entire resulting epithelium enters the solution, which is then centrifuged and cleared of unwanted impurities (mucus, etc.).
Today, liquid-based cytology is becoming the “gold standard” for examining smears from the cervical mucosa. But even in this case, the sensitivity of a single study does not exceed 60-70%. During reproductive age, false negative results are common, and in menopausal women, false positive results are common.
Only triple cytological examination allows one to approach 100%.
There are various methods for staining preparations: according to Papanicolau (Pap test), according to Romanovsky, according to Wright-Diemsa, according to Gram.
The Pap test is widely accepted and is now used as the main standardized test.
How long does the test take? Depending on the organization of the process, the result can be obtained within 2-3 days.
Cytogram without features - what does this mean?
Cytological findings vary widely.
As a variant of the norm, the following conclusions can be used: “ cytogram without features ”, “ cytogram within normal limits ”, “ cytogram without intraepithelial lesions ”, “ cytogram corresponds to age - atrophic type of smear ”, “ NILM - Negative for intraepithelial lesion or malignancy”, " proliferative type of smear ." All this is NORMAL!
The cervical mucosa is normally smooth, shiny, and moist. The squamous epithelium is pale pink, the glandular epithelium is bright red. The cellular composition that can be found in normal cytology is presented in the table.
| Exocervix | Well-preserved cells of squamous epithelium, mainly of the superficial, intermediate layers. |
| Endocervix | Cells of glandular (cylindrical) epithelium. |
| Transformation zone | Squamous epithelial cells, single cells or small clusters of metaplastic squamous epithelium, small clusters of glandular epithelium. |
Atrophic type of smear - what does it mean?
In women in perimenopause and menopause, due to a decrease in the overall level of estrogen, many metabolic processes slow down, which results in atrophy of the squamous epithelium. These changes can be seen in the cytogram.
The atrophic type of smear refers to a variant of the normal cytogram. You can often find in the conclusion the phrase “ cytogram corresponds to age ” or “ age-related changes nilm ”.
All these are variants of the norm!
You need to understand that in menopausal women, false-positive cytogram results are very common - this is the case when it is difficult for a cytologist to distinguish atrophic squamous epithelium from dysplasia.
This needs to be understood because subsequent cervical biopsies usually do not find any pathology.
In addition, older women may have a tendency to keratinize the epithelium with the formation of hyperkeratosis (leukoplakia).
| Exocervix | Well-preserved squamous epithelial cells, mainly of the parabasal and basal layers. More often there are smears of the atrophic type, but they can also be of proliferative or mixed types. |
| Endocervix | The absence of columnar (glandular) epithelial cells is not an indicator of poor quality of the smear, since during this period the transformation zone moves deep into the canal and to obtain glandular epithelium the brush must be inserted to a depth of more than 2-2.5 cm. |
| Transformation zone | Cells of squamous, metaplastic epithelium. |
The mucous membrane of the cervix in menopause is thinned, easily injured and damaged, which is a consequence of a decrease in estrogen.
Terminology
Cytology smear is normal
Dyskaryosis and dyskaryocytes are abnormal cells with hyperchromatic (dense and dark) nuclei and irregular nuclear chromatin. Dyskaryosis will be followed by the development of a malignant neoplasm. Used as a synonym for dysplasia, but as a more general term.
Atypia is any difference in cell structure from the norm. The meaning often depends on the context. But more often it is used to describe pre-tumor and tumor changes.
Inflammatory atypia is a combination of degenerative, reactive, proliferative changes in cells during inflammation. These changes can cause a false-positive diagnosis of dysplasia or cancer.
Dysplasia is a process of impaired maturation of squamous epithelium. It is a true pre-tumor process. Has 3 degrees. The first usually includes a viral lesion, the second and third - a lesion with tumor potential.
Severe epithelial dysplasia
ASCUS are atypical cells that are difficult to differentiate from reactive atypia and the pretumor process itself. Atypia of unknown significance.
Dyskeratosis is a disorder of keratinization of individual squamous epithelial cells. Is a sign of HPV.
Parakeratosis is a disorder of keratinization of the epithelial layer. Surface squamous epithelial cells always have some degree of keratinization - this is a protective mechanism. Parakeratosis can be observed normally, with irritation of the mucous membrane for any reason, or with HPV infection.
Koilocytosis (koilocytic atypia, koilocyte) is a specific nuclear change characteristic of the human papillomavirus.
Koilocytes, multinucleate cell
Hyperkeratosis (leukoplakia) is pronounced keratinization of the epithelial layer with the appearance of a protective structureless layer of keratohyalin. This is a normal process for the skin, but in the mucous membranes it is considered a pathology. It is observed with HPV infection, as well as with irritation of the mucous membrane, especially with prolapse of the pelvic organs and uterine prolapse.
Squamous metaplasia is a protective mechanism, a physiological process of replacing delicate glandular epithelium with more stable squamous epithelium. Metaplastic epithelium often becomes a source of dysplasia and cancer, as it is easily affected by the human papillomavirus.
Glandular hyperplasia - proliferation, active growth of glandular epithelium. It is a reactive process during inflammation and erosion of the cervix. Often occurs when using hormonal drugs.
Bethesda classification (USA) - cytogram decoding
| Full material | Contains squamous and columnar epithelial cells in sufficient quantities. |
| Material unsatisfactory for assessment (uninformative) | Poor or absent number of cells. |
| Cytogram within normal limits (NILM) | Contains cells of the superficial and intermediate layers of multilayered squamous epithelium, metaplastic epithelial cells, leukocytes, columnar epithelial cells, endometrial epithelial cells. |
| Metaplasia (normal) | Cells of squamous metaplastic epithelium indicate that the material was taken from the transformation zone. |
| Cytogram of inflammation | Degenerative and reactive cell changes, inflammatory atypia, squamous metaplasia, hyperkeratosis, parakeratosis, koilocytosis and other signs of viral damage. |
| Atrophy | Cells of the basal and parabasal types are small cells with a hyperchromatic nucleus and scanty cytoplasm. They can often be misinterpreted as atypia cells, giving a false positive cytology result. |
| ASCUS (atypical squmous cells of undetermined significance) | Changes that are difficult to differentiate between reactive changes in the epithelium and dysplasia. ASCUS identifies cells that are difficult to interpret—cells with dyskaryosis, enlarged and hyperchromatic nuclei. Dynamic observation and further examination are recommended, namely repeated cytological examination after 6 months and HPV testing. If ASCUS is confirmed and the presence of human papillomavirus of high oncogenic risk, colposcopy is performed. Research shows that 20% of women with ASC have dysplasia after more careful examination. |
| LSIL (CIN I) | Mild intraepithelial lesion, including human papillomavirus infection. Observation without active therapy is recommended. In most women, LSIL resolves on its own within a few years. This group includes all changes with low malignant potential, since the cytologist often cannot distinguish between changes due to HPV infection and CIN 1 itself. |
| HSIL (CIN I-II) | Moderate to severe intraepithelial lesions. It is recommended to remove all affected tissue using a method (conization) followed by morphological examination. This group includes all changes with a high malignant potential. |
| AGC (atypical glandular cells) | Atypical columnar epithelial cells. It is recommended to scrape the cervical canal for histological examination. |
| Squamous cell carcinoma | Malignant tumor of squamous epithelium. |
| Glandular cancer | Malignant tumor of the glandular epithelium of the endocervical type. |
| Endometrial cancer | A malignant tumor that develops from the lining of the uterus and grows into the cervical canal. |
Source: https://probotox.ru/venerologija/kletki-cilindricheskogo-jepitelija-s-reaktivnymi.html