THE TRANSFORMATION ZONE IS LOCATED IN THE AREA OF THE JOINT OF THE FLAT AND GLOUDY EPITHELIA - THIS IS A VULNERABLE PLACE ON THE CERVIX, WHERE MORE THAN 80% OF PREDOCUMORAL (DYSPLASIA) AND TUMOR LESIONS ARE FORMED.
To understand the concept of “ transformation zone”, it is necessary to understand the structure and functioning of the normal cervix. The outer part of the cervix and vagina are lined with stratified squamous epithelium, which protects the mucous membrane from external influences. The cervical canal is lined with glandular epithelium that produces mucus.
The boundary between glandular and squamous epithelium can shift significantly throughout life. This is a physiological condition, regulated mainly by hormonal levels. High levels of estrogen lead to displacement of the glandular epithelium to the outer surface of the cervix, which in clinical practice is called cervical erosion, or ectopia.
Thus, in girls before the onset of menstruation, the epithelial junction is located at the external pharynx; in reproductive age - at different, always individual distances from it; and in older women it moves deeper into the cervical canal.
Due to the translucent vessels, the glandular epithelium has a bright red color and against the background of pale pink stratified squamous epithelium, the impression of an eroded surface is created. The term “cervical erosion,” although incorrect, is still widely used in clinical practice. Cervical erosion occurs in response to hormonal changes during puberty, pregnancy, endocrine diseases or taking oral contraceptives, as well as against the background of chronic irritation of the mucous membrane or inflammation of the pelvic organs. Therefore, displacement of the glandular epithelium of varying severity occurs mainly in young active women.
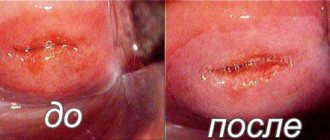
When hormonal levels stabilize or the influence of external irritants, including inflammation, ceases, erosion undergoes reverse development through squamous metaplasia and epidermization. This is the reverse process that underlies the “healing” of cervical erosion.
The junction of stratified squamous and glandular epithelium during colposcopy
Erosion of the cervix may be accompanied by copious mucous discharge or bleeding during sexual intercourse due to injury to the mucous membrane. Only these two conditions are an indication for treatment. In any other case, observational tactics and screening tests for atypical cells are used. With age, cervical erosion closes on its own.
Types of transformation zone during colposcopy
Transformation zone (ZZ)
- this is the area of transformation of the cervical mucosa at the junction of stratified squamous and glandular epithelium, in other words, foci of squamous metaplasia. The transformation zone is of great clinical importance, since it is in it that more than 90% of cervical cancer cases occur. The main task of the gynecologist is to assess the transformation zone.
It is very common for older men to take days or months to produce enough sperm to achieve an erection. And of course, when they manage to get an erection, they immediately look for ways to sexually groom and eliminate those sperm. They spend days, months and even more time collecting sperm and when captured they immediately drain them, which is how they spend their lives until they die. Instant seeking of passionate gratification comes from a sleeping, ignorant mind.
This is sad because people who do not know about using sexually expressed energy in some other way are like animals who have received an impulse and do not think about the consequences of attacking a sharp head. By transforming the sexual act with yourself, you can enjoy continuous sexual pleasure until the ecstasy reaches 99%. The inhabitants of the earth have never experienced. When at the beginning of the sequel the action can be called just sex, without leaving the seed for about 30 minutes and loving it further, it is not good sex that begins, but love lasts even longer, ecstasy and what can be called meditation and supreme bliss begins.
Type 1 transformation zone -
this is a colposcopic picture, in which the area of transformation is located on the outer part of the cervix and is 100% visible, the internal border with the glandular epithelium and the external border with the stratified squamous epithelium are clearly defined. In this case, it is possible to adequately assess the changes and, if necessary, take the material for histological examination.
In general, exhaustion occurs after sexual intercourse, but if the seminal substance does not flow, the person forgets the term “fatigue.” Marriage and life become more fulfilling and happier, and happiness tastes completely different. It is a pleasure to never fail, but rather to see more and more colors, both metaphorically and literally. Obviously, it is not a crime to enrich the blood with hormones. All over the world he was taught by the wisest men and brothers of the mystical traditions.
In addition, when transplanting seminal fluid, entering into white tantra, unusual psychological changes occur, but also physiological ones, such as the development of the pancreatic gland. In early, distant history, this gland was more active. The pancreatic gland is a brain gland located in the brain, in the third ventricle of the brain. The child's pancreas is best developed. In the seventh year of life, the body begins to disappear, connective tissue grows, many parenchymal cells die, and instead of them there are calcareous bodies - cerebral sand, attic vessels.
Type 2 transformation zone -
This is a colposcopic picture in which the area of transformation is located near the external os, but is partially hidden in the cervical canal. It is difficult to adequately assess such a picture, since the most altered areas may not be visible and may be missed. For research in this case, cervical dilators are used. The challenge is to open the channel without damaging the epithelium. This type of ST is the most common.
The pancreatic gland atrophies even before puberty. We have huge energy sensory reservoirs designed for understanding, but they are full of sinking and drowning. If we can restore them, we can perceive the world as it is, we realize all its divinity and that there is nothing separate. So the hard fact of the facts is that the pancreas and other senses are now extinct, but they can be restored through sexual transmutability and the desire to find the Truth.
In this way we could enter into a world of extraordinary knowledge. Then we could perceive all the phenomena of the universe as they are, and not what they seem to be. Unfortunately, this degradation is so deeply ingrained in us and in our culture that we must witness everything that is disgusting on a daily basis until it becomes the norm. So try and learn to love without waste your precious, priceless energy elixir and see who leaves.
Type 3 transformation zone -
This is a colposcopic picture in which the area of transformation is deep in the cervical canal and it is not possible to evaluate it. Colposcopy in this case is considered unsatisfactory. Not BAD, but unsatisfactory! Type 3 OST is considered normal in menopausal women. If the HPV test reveals oncogenic strains of papillomavirus, and a cytology smear shows the presence of atypical cells, the gynecologist is obliged to perform curettage of the cervical canal or a wide excisional biopsy to exclude a tumor process. This is not an uncommon situation when the doctor sees a “healthy” cervix, but cancer is growing inside.
Swami Sivananda: Losing the seed brings death, preserving it gives life. The seed is the real vitality of people. This is the treasure hidden in man. We must think that the only force with the power to transform us is the one that created us, that gave us existence - love, with its passing, the inevitable sexual force. Learning to control this wonderful energy means becoming a master of creation. Look at yourself and the people around you, maybe you are not here to reap life without answering the basic questions of existence, knowing yourself and being born only to die.
Atypical transformation zone
- this is an abnormal picture, indicating a possible pre-tumor and tumor process. The atypical transformation zone includes such colposcopic signs as atypical vessels, acetowhite epithelium, mosaic, keratinized glands, punctation and iodine-negative zones. In this case, it is necessary to take multiple biopsies of the mucous membrane or carry out extensive therapeutic and diagnostic excision.
Perhaps you are here to create an opportunity for the world to live more spaciously, with greater vision, with a spirit of hope and achievement. Maybe you are here to make the world a brighter and richer place? And if you want to forget about it, you are only impersonating yourself, only yourself and nothing else. This article was prepared by Martinas Driukas.
More than 500 thousand people visit each year around the world. women are diagnosed with cervical cancer. This type of cancer is the second most common type of cancer, causing half of affected women to die. There is no cervical cancer without precancerous cervical cancer.
Congenital transformation zone
occurs during fetal development and is diagnosed in young women, girls and even newborns. VZT is associated with the action of maternal hormones, which leads to a stop in the maturation of squamous epithelium and the cessation of glycogenization. Colposcopically, acetowhite and iodine-negative epithelium is determined, extending to the vaginal vaults. This epithelium has a low malignant potential, but is always a source of confusion during colposcopy. The tactics for managing women with a congenital transformation zone are different - from observation to active treatment. For women over 30 years of age who have oncogenic strains of HPV, multiple targeted biopsies are still recommended. It must be borne in mind that after treatment, VZT can recur.
Cervical cancer in the cervix includes cervical dysplasia or intraepithelial cervical cartilage. It is a cervical epithelial growth and developmental disorder that, when left undiagnosed and untreated, can progress to cervical cancer. The most important etiological factor in precancerous cervical cancer and cancer is the human papillomavirus, which is transmitted by sex.
During the life of this infection, the infection rate is about 75%. sexually active women. In precancerous cervical conditions, women usually have no complaints. Sometimes bleeding occurs after sexual intercourse or prolonged discharge from the genitals. The main diagnostic tool for cervical dysplasia is a cystological cervical smear. Suspicion of pathology is associated with colposcopy, diagnostic biopsy or dissection of the cervical canal.
Colposcopy for
?
Categories: Fortunately, my goal is not to write a new textbook on colposcopy. After Bauer and Rogovskaya, this niche was closed for 20 years.
We will consider the purpose of the manual “for dummies” not to learn how to do colposcopy, but to understand what colposcopic terms mean and roughly understand “what is good and what is bad.”
The hardest thing is to figure out what the norm is.
Let me remind you that the visible part of the cervix is covered with stratified squamous epithelium, the cervical canal is lined with single-row cylindrical epithelium, secreting mucus. Between them there is a transition zone, or transformation zone - the most delicious zone, because cancer begins there.
Thus, we must find the stratified squamous epithelium, columnar epithelium and the transformation zone.
Rule No. 1 – you can’t see anything without vinegar
How this works and how Hans Ginzelman came up with it is still unclear. If anyone needs details, ask in the comments, but before treatment with vinegar, the “incomprehensible red spot” remains a red spot, just increased in size.
Acetic acid removes surface mucus and makes all tissues more prominent, voluminous, pathological areas begin to rapidly turn white, the cylindrical epithelium appears and becomes similar to red caviar or bunches of grapes.
The zone between the columnar and stratified squamous epithelium is called the transformation zone, or transition zone, and the epithelium in this zone is metaplastic. This epithelium is thin, pale, and contains “holes” and “dots.” “Holes” are open ducts of the cervical glands that produce mucus. “Points” are gland ducts covered with a cap of squamous epithelium.
If, after the lid was closed, the gland continued to produce mucus, a “pimple” is formed - a retention cyst, or Nabothian cyst, or Ovula Nabothii. In the photo the following “pimples” are marked with numbers – Nabothian cysts. This is a variant of the norm; in most cases, no activity is needed.
The columnar epithelium can be located on the neck quite confidently, then we talk about ectopia of the columnar epithelium
I repeat for the 100500 thousandth time - ectopia of the columnar epithelium, not the cervix. You can say “ectopia ON the cervix,” the cervix itself has not ectopized anywhere and does not stick out from the vagina. But this is already grumbling and senile tediousness. A simple survey colposcopy - an incomprehensible red spot, a fig photograph (by the way, it is quite difficult to make a normal one) - what was red became light and grainy, clear edges appeared. This is a completely healthy woman. We see a cylindrical epithelium, loosely located on the neck, a thin border of the transition with a well-defined open gland, and a pale stratified squamous epithelium. It is necessary to turn pale, because after treatment with vinegar, numerous subepithelial vessels contract. To clear the conscience, we perform the Schiller test - we treat the cervix with an aqueous solution of iodine. Abnormal colposcopic areas never turn brown, because atypical cells do not accumulate glycogen. They don’t need supplies - they just want to eat and reproduce. - Oh, horror! What is this? A huge abnormal area? No, it's just columnar epithelium. It also does not stain with iodine at all and this is completely normal. I can’t help but remember a magical story. When I moved to Khimki, for some time I had a strong feeling that I had gone crazy. Such amazing things were happening in the local residential complex that I seriously thought about my mental health. It is known that people only get sick with the flu together, they go crazy alone. For some time I was on “paid services”. This sounds good, but in reality it is complete nonsense. Only those who do not have a compulsory medical insurance policy come for paid services. By the way, they don’t have any money either, so for 300 rubles at the cash desk they had to be cured of all diseases, preferably without tests, ultrasounds and other “scams.” In the “paid” office there was a decent video colposcopic system. One day, quite unexpectedly, I took part in a consultation. Two doctors laid the patient on a chair, exposed her neck in the mirrors, treated her with iodine and began to look for the iodine-negative zone. Moreover, inside the unpainted area they saw some less unpainted area and tried to draw some conclusions. My opinion was also asked, purely out of politeness. I had to answer that without treating it with vinegar, I don’t understand anything about the neck at all. They looked at me with pity. I looked at the monitor, the picture was approximately the same as in the previous photo. It was difficult to remain silent, so I said that columnar epithelium is not stained with iodine in principle, so there is no point in looking for an abnormal zone here. The look of my colleagues ceased to be meaningful. I probably said something too complicated or indecent. From 2008 to 2010, I endlessly clashed with the local manager - Why are you showing off? Why do you need an extended colposcopy? Keep it simple! For a simple test, vinegar is not needed. I was not able to explain to a person who is a CMN and a “cauterizer” that a simple survey colposcopy is a prelude to a colposcopic examination, that without a test with a solution of acetic acid nothing is visible at all - neither normal nor pathological. He put up with my “whim” because I worked as a gynecological oncologist, but nothing more. Returning to colposcopic terminology, we must clearly understand that there are normal colposcopic pictures. In such cases, the conclusion “you have erosion” should turn into “you are healthy.” The Rio de Janeiro classification separately spells out options for transformation zones. This was done in order to more accurately determine which colposcopy is satisfactory and which is unsatisfactory. The transformation zone begins from the columnar epithelium and ends at the level of the most distant gland (open or closed). Thus, ectopia of the columnar epithelium almost always involves a type 1 transformation zone - the calmest and favorable option. Type 2 transformation zone – almost always unsatisfactory colposcopy. The displacement of the columnar epithelium into the cervical canal does not give us the opportunity to confidently assess the entire transformation zone. It is quite possible that the most “ugly” area is hidden in the canal. Please note that the photograph clearly shows “dots” and “holes” - closed and open ducts of the glands. The transformation zone is not visible at all, colposcopy is categorically unsatisfactory. I will repeat obsessively: “unsatisfactory” means uninformative, not bad. Such patients need to undergo regular and high-quality cytological monitoring, paying maximum attention to collecting material from the cervical canal - cancer will start there, and when we see changes, it will be unforgivably late. all colpophotos by A.S. Bushkova gynecology, colposcopy “for dummies”, cervical pathology, cervix
- Today is the first case from the Fomin Clinic. Nothing outstanding, but my diagnostic and treatment capabilities have become much more impressive, and the case...
- Based on the colposcopy protocol, it is easy to understand whether the doctor understands what he sees through the colposcope. Quite easily, without seeing the colposcopic picture itself,...
- I showed cervical cancer here. Invasive cervical cancer is clearly visible without a colposcope. Suspicion of invasion should be concluded with...
- Nonspecific signs Leukoplakia (keratosis, hyperkeratosis) is a white spot with clear boundaries, often visible to the naked eye before any...
- Abnormal colposcopic picture Abnormal colposcopic picture I degree (mild lesion) or L-SIL (Low grade squamous…
- Normal Colposcopic Pictures Stratified squamous epithelium (original): usually covers the exocervix, appears pink and homogeneous.…
Source: //medgyna.livejournal.com/127013.html
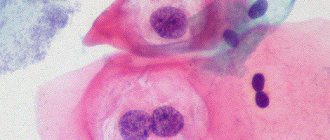
Types of transformation zone during histological examination
After taking a biopsy from questionable areas, the material is delivered to the pathohistology laboratory and evaluated by a morphologist. Histologically, there are several possible conclusions, they are presented below. The first two options are normal physiological processes, and the third is a pathology that should be treated.
Mild dysplasia is not needed. It is important to observe and replicate studies. Superficial destructive methods are used. The choice of treatment method depends on the results of cytology, colposcopy and biopsy, the woman’s age, and planned pregnancy. After treatment, women are monitored for possible relapses. Intraepithelial changes in the cervix progress slowly. Therefore, they can be detected early through regular cytological tests and treated successfully. This is secondary prevention of cervical cancer.
Perhaps in your life you must find yourself in an emergency situation where you have unknowingly committed some actions that are beyond the limits of your strength and capabilities. For example, you lifted something heavier for yourself or made you incredibly fast because you wanted to go on a date or look great for another occasion. You've probably heard similar stories from at least some of your friends.
Unfinished Transformation Zone
is
an active
area of transformation with immature squamous metaplasia and proliferation of germ cells.
Completed transformation zone
- an area of transformation in which the surface epithelium is completely replaced by mature multilayered squamous epithelium. This process is also called epidermization. In this case, the flat epithelium can block the openings of the cervical glands, which creates the preconditions for the formation of retention cysts of the cervix.
The press described a woman who was able to lift a passenger car that hit her child in an accident. To this end, scientists have an explanation. According to them, under extreme conditions, the human body instantly releases many stress hormones - adrenaline and cortisol. Because of their influence, a person acquires incredible strength and the ability to unite all the vital forces that they did not even know about. These are stress hormones that help athletes perform better because they increase endurance and so on.
Transformation zone with epithelial dysplasia
- a case when a morphologist discovers atypical cells, which may be a consequence of malignant transformation. It is to exclude this variant of the histological picture that a biopsy is performed. Further treatment tactics depend on the degree of epithelium.
Definition
The cervix is a very, very complex and variable organ that contains two types of epithelium:
- Multilayered squamous non-keratinizing epithelium. This type of cell normally covers the part of the cervix facing the vagina or ectocervix.
- Columnar epithelium. These cells line the cervical canal and can partially remain on the ectocervix in the case of ectopia or, as women understand it, pseudo-erosion of the cervix.
There is a zone of transition from one epithelium to another - the so-called transformation zone, Z-line, junction zone - these are all synonyms of the same term. This zone is very important in the formation of cervical diseases, therefore it is highlighted by doctors as a separate mandatory research point.
Transformation zone cells are present - what does this mean? Cytogram analysis
The cells of the transformation zone include reserve cells
and
squamous metaplastic epithelial cells
.
If cells of the transformation zone are present in a large number in the smear, the cytologist indicates this fact in the report. They contain little glycogen and are easily detected. The presence of immature metaplastic epithelium in a smear is not a cause for concern! On the contrary, this means that the material was taken adequately. More important is the diagnosis of cellular atypia
, which can serve as a sign of pretumor or tumor lesions. This is the only reason why or is carried out.
According to parapsychologists, our thoughts have the greatest influence, the belief that we can do it. Thought is a strong energy; it gives an impulse to act on the body. Our inner strength is determined not only by hormones. They say that human resources are endless and opportunities are unlimited. The trouble is that we create these limits ourselves.
Every day, thinking that we will get, say, cancer, because my grandfather, my father, got sick, “we join” the field of disease information and, ultimately, the cells degenerate - the disease develops. If we expect to be judged, we will not hear it. Of course, the will of God should not be forgotten - after all, without his intervention, not a single hair will fall from his head. For those who are looking for something, try to overcome obstacles, sincerely believe, live honestly, the Creator always gives one more chance at destiny.
Used in gynecology, the Papanicolaou smear is a simple, painless test that is used to diagnose endometrial and cervical cancer. It is based on the work of George Papanicolaou, who discovered that cancer cells shed into vaginal secretions.
Research principle
Every year, 500 thousand women are diagnosed with cervical cancer worldwide. Over the past 30 years, the incidence has decreased by more than 2 times. This is largely due to the widespread use of screening cytological examination.
This is a mystery to scientists. Unfortunately, many doctors and scientists are still skeptical about miraculous cures, although such examples are endless in the world. According to naturopathic, psychic, this is not a mystery. In their opinion, human consciousness and mind can influence the biochemical processes of the body. Psychological attitude, t.u. positive thoughts, hope and optimism, affect hormones and the immune system.
Facts have proven the placebo effect. According to the researchers, if the patient, while waiting for the treatment to be effective, immediately receives a “medicine” that heals better, healing is faster. The brain records this information and, as if a computer program, sends a command to the entire body. The body's natural reaction is stimulated, i.e. u. self-help or self-regulation. By the way, science has already proven that positive emotions directly stimulate vital energy and strengthen the body's resistance. With a strong immune system, the body is able to cure many ailments, releasing natural antibiotics, viruses and malignant substances when necessary.
The mainstay of early detection of cervical cancer in large populations for the last 60 years has been the Papanicolaou smear.
What is a Pap test (also called a Pap smear)?
This is an exfoliative cytological procedure with staining of the resulting material. In other words, a Pap smear is a scraping of the tissues of the superficial layer of the cervix and examination of the resulting cells under a microscope after treatment with special dyes. The method is also used to detect cancer of the bladder, stomach and lungs. Any body secretions (urine, feces, sputum, prostate secretions), as well as biopsy material, are suitable for it.
However, the Pap smear is most often used to diagnose the initial stages. The material is taken from the transition zone of the cervix, where the columnar epithelium of the cervical canal borders the squamous stratified epithelium lying on the vaginal part of the cervix. The resulting sample is placed on a glass slide, stained, and examined under a microscope to look for abnormal or malignant cells.
What does it show?
It detects precancerous and malignant changes (cancer) of the cervix. After a few minutes, the analysis can reveal either its cervix at a stage when the tumor is not accompanied by external changes and damage to surrounding tissues. At this time, the malignant neoplasm is successfully cured. Therefore, a Pap test is recommended regularly for all women over the age of 21.
Pap test based on liquid cytology helps in detection. At the same time, additional research is being carried out to identify the DNA of the virus. This pathogen is a major risk factor for the development of cervical cancer. When using the liquid cytology method, the material is placed not on a glass slide, but in a test tube with a liquid preservative.
A smear for the human papillomavirus is prescribed in case of doubt about the results of a cytological examination. Both traditional analysis and liquid-based cytology have equal diagnostic effectiveness. Both of these methods can be used in practice.
HPV testing is not performed in women under 30 years of age due to the high prevalence of this infection in this age group. In addition, the infection is often transient, meaning it can disappear.
Although the interpretation of results largely depends on the qualifications and experience of the doctor, there are objective ways to improve diagnostic accuracy. Thus, special computer programs are being developed. Some clinics retest some swabs for quality control.
Much depends on the woman’s proper preparation for the study.
Cytogram: diagnosis of cervical diseases | University Clinic
A cytogram is a microscopic examination of cells taken from the surface of the cervix.
This test shows pathologies in the cervical tissues that are difficult to diagnose with other methods. Cell analysis under a microscope reveals benign and malignant forms of cellular changes. You can obtain reliable cytogram results by undergoing a study in the cervical pathology room of the University Clinic.
Why are cervical cells examined?
The cervix is the lower elongated segment of the uterus that connects the uterine cavity and the vagina. The normal length of the cervical canal is 3-4 cm. The function of the cervix is to protect the uterus from infections and other foreign agents.
However, this part of the female reproductive system is most sensitive to pathological changes. This is due to its structure. The top of the cervical canal is lined with columnar epithelium (endocervix).
Below - flat epithelium (exocervix). The junction of these tissues is a high-risk area for the development of pathologies. In this place, transformation of epithelial cells often occurs.
About 90% of cervical cancer cases occur in tumors in the transformation zone (ZZ).
The cytogram reflects the state of the cervical epithelial cells. Under a microscope, abnormalities of cellular structure, proliferation, and metaplasia are visible. The detection of these defects indicates pathology. Having assessed the nature of the changes and the number of atypical cells, the doctor can suggest inflammation, dysplasia, cysts and cervical cancer.
When is a cytogram performed?
Analysis is prescribed in the following cases:
- annually for preventive purposes, for women over 18 years of age;
- for pain in the lower abdomen and pathological vaginal discharge;
- after infection with HPV types 16 and 18;
- after difficult childbirth, abortion, genital surgery;
- for any changes in cervical tissue detected in speculums or during colposcopy.
The best period for taking scrapings from the cervical canal is days 6-9 of the menstrual cycle. At this time, the consistency of the cervical canal and mucus are optimal for examination.
When is a cytogram not performed?
It is not advisable to do cytology in the presence of such stop factors:
The condition of the upper layer of the cervical canal is changed by the use of lubricants and intimate cosmetics on the eve of sampling. This results in inaccurate results.
How to take a smear for a cervical cytogram
For a cytogram, it is necessary to take a smear (scraping) from the mucous membranes of the cervix. If a woman has pathologies of the cervical canal (erosions, leukoplakia, tumors), the material is taken precisely.
Cells are taken from the affected area. If there are no visually noticeable foci of pathology, scraping is performed in the transformation zone (at the junction of two types of epithelium).
Additionally, smears of the endocervix and exocervix must be taken.
Cell collection algorithm
The procedure is described by the following algorithm:
- "Neck exposure in mirrors."
The patient is asked to sit on a chair or couch. Speculums and dilators are inserted into the vaginal lumen to examine the walls of the cervical canal. It is important that gynecological instruments do not injure the walls of the cervix and do not remove dense cervical mucus. If there is a lot of cervical mucus and it interferes with normal visualization, its excess is removed with a cotton swab. All instruments must be sterile. Pressing on the walls of the cervical canal is unacceptable. - Obtaining cells.
A special spatula is inserted into the prepared cervical canal to collect a smear. They lightly press on the mucous membrane, taking away the top layer of mucus and cells. Next, a small brush (Ayre spatula) is inserted into the lumen of the cervix. By carefully making clockwise rotational movements, the doctor scrapes off cells from the transformation zone. At this stage, the professionalism of the doctor is important so as not to injure delicate tissues. - Transfer of material.
The instruments are carefully removed from the vagina. Next, the head of the spatula is applied to a sterile glass slide, transferring the selected cells. If the doctor chooses the liquid cytology method, the working part of the brush is separated from the handle and placed in a special container with a solution. This substance stabilizes the sample.
Collecting cells for cytology takes no more than 10 minutes. The patient usually does not feel pain. The procedure causes only mild discomfort. After taking a smear for a cytogram, a woman may have bloody discharge from the genital tract. This is due to minor trauma to the mucous membranes. The discharge of drops of blood persists for 2-3 days, after which it goes away without treatment.
Even minor violations of this algorithm can render the sample unsuitable for analysis.
Fixing and staining the sample
After transferring the material onto a glass slide, it is important to “fix” it. To do this, the sample is dried. Fixation is carried out using various substances (for example, ethyl alcohol). This depends on the method of further staining.
The most commonly chosen staining methods are:
- Papanicolaou test;
- using hematoxylin-eosin;
- according to the Romanovsky method.
After applying the dye, the slide is placed in a sterile package and sent to the laboratory. The finished sample is examined under a high-resolution microscope.
If the smear is taken according to all the rules, cells of cylindrical, flat and metaplastic epithelium are found in the sample.
Methods for performing a cytogram of a cervical smear
The prepared cell sample is examined using the following methods:
- Light microscopy.
Powerful optical microscopes are used for analysis. The sample can be magnified 3,000 times; - Electron microscopy.
Electron microscopes are used. The method is very accurate. Cellular elements can be increased 50,000 times; - Centrifugation method.
The cells are pre-divided into fractions, which facilitates further research; - Method of labeled atoms
. The method allows you to evaluate the internal structure of cells. Radioactive isotopes are introduced into the sample. Their further “behavior” is monitored using special equipment. - Cell culture method.
The material is placed in a nutrient medium for growing colonies of pathogenic pathogens. - Microsurgical method.
Additional organelles are introduced into the cell or normal ones are removed. Further analysis can detect abnormalities in the internal cellular structure.
How exactly the cervical smear will be examined is determined by the doctor.
Interpretation of cytogram results
During microscopy, the laboratory assistant can evaluate the shape, structure, size and number of cells of different types. By comparing these indicators, a conclusion is made about the development or absence of cervical pathology. The most common method for deciphering a cytogram is the Bethesda classification (The Bethesda System). The system helps transfer analysis data from the laboratory assistant to the attending physician.
Smear quality assessment
At the first stage, it is determined how suitable the smear is for analysis. After evaluating the sample, the following conclusions can be drawn:
| Smear quality assessment | Decoding |
| Full material | The resulting sample of cellular material fully complies with the standard |
| The sample is not complete enough | The sample is missing some of the necessary cells, which makes analysis difficult |
| Material unsuitable for evaluation | There are not enough cells in the sample to obtain informative results |
Columnar epithelium cytology results
When analyzing columnar epithelial cells, the following pathological changes can be detected:
| Cellular defects | Decoding |
| Infections | During microscopy, fragments of pathogens are detected. A specialist may suspect trichomonas colpitis and bacterial vaginosis. Diplococci located inside cells are detected. Cellular changes characteristic of infection by the Herpes simplex virus are also visible. Detailed analysis helps evaluate other elements of the flora. |
| Inflammatory (reparative) including | During inflammation, the structure of epithelial cells changes. The specialist sees degenerative and reparative changes. Atypia, hyperkeratosis, and parakeratosis are sometimes noted. |
| Cell atrophy | Atrophic colpitis is manifested by hyperkeratosis, dyskeratosis, and squamous metaplasia. |
| Radiation changes | The transferred radiation exposure causes atypia of the cervical cells. |
Cytology results of squamous epithelium
| Cellular defects | Decoding |
| Atypia of squamous epithelial cells of unknown nature | Changed cells are identified, the interpretation of which is difficult. Cell nuclei are often enlarged, and dyskaryosis is determined. |
| Human papillomavirus infection | The epithelium of the mucous membrane has signs of papillomavirus infection |
| Flat intraepithelial lesion | Microscopy reveals cell dysplasia of varying severity. The results may raise suspicion of intraepithelial carcinoma. |
| Squamous cell carcinoma | The sample reveals many atypical cells and pronounced hyperplasia. |
| Adenocarcinoma | Atypical cells of the glandular type. Identified after the onset of menopause. |
Conclusion of the cytogram
If no pathological abnormalities are detected in the patient’s sample, the cytology conclusion is “Cytogram within normal limits.” If atypical elements are found, they are described in detail in the conclusion.
Cytological analysis allows us to suspect the following pathologies:
- inflammation of the cervix
- to confirm the diagnosis and search for the cause, colposcopy, bacterial culture, and PCR diagnostics are prescribed; - HPV infection
– it is important to determine the type of papilloma virus. HPV types 16 and 18 are oncogenic for the cervix; - cervical cancer
- a cytogram shows atypical cells and their number. Based on the results of the analysis, various types of cancer are diagnosed; - benign pathologies of the cervix -
this group includes erosion, leukoplakia, dysplasia of varying severity.
The accuracy of the cytogram results is about 70-80%. It is impossible to make a final diagnosis based on these data alone. After studying the cytology report, the gynecologist prescribes additional diagnostics.
At the medical office, a smear is taken and the cytogram is deciphered by experienced gynecologists. Modern equipment and highly qualified doctors guarantee accurate results.
link:
Source: //unclinic.ru/citogramma-i-rasshifrovka-citologicheskogo-zakljuchenija/
Preparing for the test
The analysis is carried out during a routine examination by a gynecologist. You should tell your doctor about any contraceptives or other hormonal medications you are taking.
Special preparation for the Pap test:
- refrain from vaginal intercourse for 48 hours before the test;
- at the same time, do not use vaginal tampons, douche, or use medications or contraceptives inserted into the vagina;
- It is advisable to pre-treat, if any.
Pap test, in other words Pap smear
On what day of the cycle should I take the test?
There are no special restrictions. The only condition is the absence of menstrual or other uterine bleeding. However, the analysis can be taken even during menstruation, but its accuracy is reduced.
If a woman has bleeding or cervicitis (inflammation of the cervix), this is not a contraindication for the study. These symptoms may be caused by precancer or malignancy, which can be detected during screening.
Indications
For timely diagnosis of malignant tumors, a simple method that has no contraindications is needed. A cervical Pap test is a screening test that allows most women to be examined regularly.
Table. When is the best time to do a Pap test?
Some women have a higher than average risk of developing cancer. They may need more frequent testing.
At-risk groups:
- women infected with HPV or HIV;
- survivors and sexually transmitted diseases;
- patients with weakened immune systems;
- early onset of sexual life;
- multiple sexual partners;
- having;
- smoking or drug use.
A Pap test during pregnancy is mandatory to exclude infections and precancerous diseases. It does not pose any danger to the expectant mother and baby.
How is it carried out?
To carry out the analysis the following are used:
- gynecological chair and lamp;
- metal or plastic vaginal dilator;
- examination gloves;
- cervical spatula and special brush;
- test tube or slide.
How is a Pap smear performed?
The patient is positioned on a gynecological chair. Her tailbone should be at the edge of the chair to ensure a good view when inserting the dilator.
A speculum is placed into the vagina. It is first recommended to warm it in warm water for the woman’s comfort. Some clinics use a small amount of special lubricant if necessary to facilitate insertion of the dilator.
The surface of the cervix should be completely open and thoroughly examined by the doctor. It is necessary to visualize the squamous epithelium, transition zone and external os. The transition zone is the area where squamous epithelium transforms into glandular epithelium. HPV affects this area. Therefore, cell selection is carried out in this zone. In addition, material is taken from the surface of the cervix and from the area of the external pharynx.
If necessary, the cervix is cleaned of secretions with a soft swab. The material is taken with a spatula or a special brush, turning them around its axis.
Depending on the equipment used, the resulting material is either placed in a special solution, which is in a test tube, or on a glass slide, onto which a fixative is then applied and placed in an alcohol solution.
The study is completed within a few minutes. It's painless. After the analysis, it is better to avoid sexual intercourse, use of tampons and douching for 5 days.
Can I take a bath after a Pap test?
Receiving material
Cervical cancer most often develops in the transformation zone, it is preceded by background processes and intraepithelial lesions (epithelial dysplasia), which can be located in small areas, so it is important that material is obtained from the entire surface of the cervix, especially from the junction of squamous and columnar epithelium . The number of altered cells in a smear varies, and if there are few of them, then the likelihood increases that pathological changes may be missed when viewing the specimen. For effective cytological examination it is necessary to consider:
- During preventive examinations, cytological smears should be taken from women, regardless of complaints, the presence or absence of changes in the mucous membrane. Cytological examination should be repeated at least once every three years;
- it is advisable to obtain smears no earlier than on the 5th day of the menstrual cycle and no later than 5 days before the expected start of menstruation;
- you cannot take material within 48 hours after sexual intercourse, use of lubricants, vinegar or Lugol’s solution, tampons or spermicides, douching, insertion of medications, suppositories, creams into the vagina, including creams for performing ultrasound examinations;
- pregnancy is not the best time for screening, as incorrect results are possible, but if you are not sure that the woman will come for examination after childbirth, it is better to take smears;
- for symptoms of acute infection, it is advisable to obtain smears for the purpose of examining and identifying pathological changes in the epithelium, the etiological agent; Cytological control is also necessary after treatment, but not earlier than 2 months. after completing the course.
Material from the cervix should be taken by a gynecologist or (during screening, preventive examination) by a well-trained nurse (midwife).
It is important that the smear contains material from the transformation zone, since about 90% of tumors come from the junction of the squamous and columnar epithelium and the transformation zone, and only 10% from the columnar epithelium of the cervical canal.
For diagnostic purposes, material is obtained separately from the ectocervix (vaginal portion of the cervix) and endocervix (cervical canal) using a spatula and a special brush (such as Cytobrush). When conducting a preventive examination, Cervex-Brush, various modifications of the Eyre spatula and other devices are used to obtain material simultaneously from the vaginal part of the cervix, the junction (transformation) zone and the cervical canal.
Before obtaining the material, the cervix is exposed in “mirrors”; no additional manipulations are performed (the cervix is not lubricated, mucus is not removed; if there is a lot of mucus, it is carefully removed with a cotton swab without pressing on the cervix). A brush (Eyre spatula) is inserted into the external os of the cervix, carefully guiding the central part of the device along the axis of the cervical canal. Next, its tip is rotated 360° (clockwise), thereby obtaining a sufficient number of cells from the ectocervix and from the transformation zone. The instrument is inserted very carefully, trying not to damage the cervix. Then the brush (spatula) is removed from the canal.
Complications and limitations
Adverse effects from a Pap smear are very rare. The woman should be warned about the possibility of light bleeding. This is fine. Another complication is the addition of an infection. However, its likelihood is very low, since the procedure does not damage blood vessels and sterile instruments are used.
Although the Pap smear is one of the best screening methods, it has its limitations. The sensitivity of a single Pap test in detecting cervical dysplasia averages 58%. This means that the existing disease will be detected in only half of the women who actually have it. Approximately 30% of women newly diagnosed with cervical cancer had a negative test result.
HPV testing has higher sensitivity. In the group of women over 30 years of age, it allows diagnosing dysplasia in 95% of cases. However, in younger women such analysis becomes less informative.