Not everyone knows why thrush does not go away. Meanwhile, the disease is very common. Thrush is vaginal candidiasis, a disease caused by the yeast-like fungus Candida. The fungus can also affect other organs, but much less frequently. Candidiasis does not only develop in women. In men, the disease is called balanoposthitis. The causative agent of the disease is a representative of the opportunistic microflora of the human body and is present in the mucous membrane of the mouth, intestines and genitals.
When conditions are favorable for fungal growth, the disease begins to develop. Due to the anatomical structure of the genital organs, milk fungus reproduces with difficulty in men and is much more often diagnosed in women.
Thrush is accompanied by itching and burning of the genitals, and a cheesy discharge. There may be pain during urination and sexual intercourse. Typically, an exacerbation of thrush is associated with a cycle of changes in the level of sex hormones in women a few days before the start of the next menstruation. In pregnant women, elevated levels of progesterone can trigger an exacerbation of thrush.
Often the disease becomes chronic and thrush does not go away for a long time. This often happens during self-medication. For treatment of pathology to be effective, it is necessary to identify the causes of the disease. Thrush is dangerous because it may hide another infectious disease that develops against the background of candidiasis.
The essence of the problem
The disease can be caused by:
- vaginal dysbiosis;
- uncontrolled use of antibiotics;
- hormonal changes;
- reduced immunity;
- concomitant infectious diseases;
- improper personal hygiene;
- metabolic disorders, for example, diabetes;
- poor nutrition with a predominance of large amounts of carbohydrates in the diet;
- wearing tight synthetic underwear that does not allow air to pass through and creates favorable conditions for the growth of fungi;
- HIV infection, which undermines the immune system;
- mental disorders, frequent stress.
A thorough examination is necessary for an accurate diagnosis. In laboratory conditions, a fungus is detected in a smear and the state of the microflora is determined.
Sexually transmitted infections must be excluded. The doctor prescribes PCR diagnostics to detect the DNA of a yeast-like fungus and its other subspecies. Using bacterial culture, the sensitivity of identified fungi to drugs used to treat thrush is determined.
With a correct diagnosis and appropriate treatment, recovery should occur. But what to do if thrush does not go away? Periodically occurring signs of the disease require consultation with a gynecologist. Only a specialist can determine why thrush does not go away. In this case, repeated diagnostics using complex test systems will be required.
It is necessary to make sure that it is thrush; sometimes the presence of a fungus does not indicate illness. The exact type of candida should be established; there are rare subspecies that require treatment with special drugs. If symptoms of thrush appear 3-5 times a year, this means that the disease has progressed to a chronic stage.
What to do if thrush does not go away? Advice from a gynecologist
It often happens that, after going through all the treatment methods, a woman notices that thrush does not disappear. Indeed, this is possible. Even if a doctor is treating you, it happens that he simply does not have enough time to tell you everything about thrush and the measures that need to be taken, except for the medication therapy itself.
Nevertheless, such recommendations exist. In order not to miss a single point in proper treatment, it is necessary to understand the disease completely - What kind of disease is this? Who's calling? Where does this microorganism live, and what living conditions are most favorable for it?
Causes of persistent thrush
Causes of persistent thrush:
- Candidiasis does not go away when the immune system is weakened for various reasons. This happens with frequent hypothermia and unbalanced nutrition.
- Herpes of the first or second type also reduces the body's defenses. Thrush will never go away if this virus is present in the body.
- Thrush does not go away for a long time due to improper treatment, which often occurs with self-medication. The wrong drug and dosage do not completely destroy the fungus. By self-medicating, you can be a carrier of thrush for several years.
- Disturbed microflora of the vagina and intestines can cause a relapse of the disease after treatment. The situation is possible when taking probiotics and prebiotics, as well as after an antibacterial course of treatment.
The use of drugs that do not cause the death of fungi. In cases where the fungus turns out to be insensitive to the chosen drug, persistent thrush occurs.
- Decreased thyroid function causes hormonal changes that cause thrush symptoms to recur.
- Changes in hormonal levels are present during pregnancy, as well as during climatic periods.
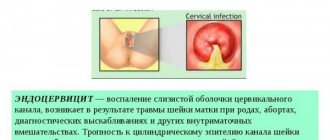
- Chronic thrush can be caused by an infection of the genital organs.
- An advanced form of thrush, characterized by severe fungal infection.
- Improper use of eobiotics, medicines that restore microflora, can also provoke a secondary manifestation of thrush.
- Diabetes mellitus, kidney failure, liver disease, and HIV can slow down the healing process.
Symptoms of the disease
If a woman is absolutely healthy and has good immunity, then candida fungi are present on the mucous membranes and epithelium in small quantities, but do not manifest themselves in any way. But for some reasons that were described above, thrush may develop. This disease is characterized by symptoms that include the following:
Treatment of persistent thrush
The chronic course of the disease is treated comprehensively and step by step. Treatment should be aimed at addressing the underlying cause of recurring symptoms. Anti-inflammatory and antifungal drugs are prescribed. External treatment includes the use of vaginal tablets, suppositories, ointments, and douching. After completing a course of antibiotic treatment, a course of microflora restoration follows. During treatment you should take a break from sexual relations. It is important to observe hygiene standards, avoid wearing synthetic underwear and using tampons during menstruation.
If necessary, seek the help of other doctors. So, if thrush does not go away due to hormonal disorders, an endocrinologist will deal with treatment. He will prescribe medications that eliminate hormonal imbalance.
In cases where herpes is detected, it is necessary to carry out antiviral drug therapy, only then will it be possible to stop the proliferation of candida. For the disease to go away completely, joint treatment of both sexual partners is required. Otherwise, re-infection will occur and it will be impossible to get rid of the disease.
Complicated candidiasis is diagnosed in older women, those who have been exposed to vaginal infections or have weak immunity. The complicated form of thrush is associated with rare varieties of Candida, the treatment of which requires special medications.
If you have HIV infection, lifelong use of antiviral and antifungal drugs will be necessary. To eliminate thrush in diabetes, you first need to lower your blood sugar levels. Then begin treatment of candidiasis. To strengthen the immune system, immunomodulatory drugs and mineral complexes are prescribed.
For the period of treatment, a diet is prescribed that abolishes flour products, fatty, spicy and sweet foods. The diet should contain a lot of vegetables, fruits, and dairy products.
Treatment of thrush in a pregnant woman involves restriction of medications, and therefore must be carried out under the strict supervision of a doctor. It is necessary to take the medications prescribed by the doctor, observing the dosage. External treatment excludes douching; ointments and vaginal suppositories are allowed. Candidiasis in pregnant women should be treated without fail, otherwise there is a risk of infection of the fetus and the threat of miscarriage.
Traditional medicine treatment can act as additional measures. Douching with decoctions of medicinal herbs such as chamomile, calendula, and oak bark is recommended. For washing, use a solution of herbs: string, lavender, nettle. Tampons with tea tree oil, used at night, are effective.
It is important to cure prolonged thrush, otherwise complications may arise in the form of:
- erosion and dysplasia of the cervix;
- genitourinary tract infections;
- inflammatory processes in the uterine cavity;
- infertility and involuntary termination of pregnancy.
Healing herbs
You can get rid of thrush with the help of folk advice and medicinal plants. My grandmother, for example, always said that for women’s diseases you need to mix chamomile and nettle at the rate of 1/3, respectively, brew and douche.
There are several more traditional medicine recipes for the treatment of female diseases, namely thrush:
- Recipe 1 . Pour 1 tbsp into a thermos. l. yarrow, sage, calendula, birch buds and chamomile. Add 2 tbsp. l. eucalyptus oil, pour one liter of boiling water and leave for 12 hours. Use for tampons or douching.
- Recipe 2 . Garlic tampons. We need 100 ml of ordinary odorless vegetable oil, add 1 tsp to it. grated or crushed garlic, mix and leave for half an hour. Then we filter and use as tampons. It is advisable to use such tampons at night. Place a cotton napkin so as not to stain your underwear with oil.
- Recipe 3 . Kefir tampons. We make a tampon from gauze or a bandage, soak it generously in low-fat kefir and insert it into the vagina, leaving a small edge outside so that it can be easily removed in the morning. In the morning, after removing the tampon, we douche with chamomile infusion.
The same recipes are used to treat thrush in men. Only instead of douching - baths and wiping.
ATTENTION. If you have an IUD (intrauterine device), using tampons is strictly prohibited! You can pull the “tendril” and the consequences will be very sad!
Prevention of chronic thrush
To avoid relapses of the disease, you should not self-medicate and neglect medical recommendations.
It is necessary to monitor the state of the immune system and take vitamin and mineral complexes. Do recreational gymnastics and hardening. You should give preference to underwear made from natural fabrics and maintain personal hygiene.
After treatment with antibacterial drugs, it is imperative to take an antifungal agent to restore healthy microflora in the mucous membranes. It is necessary to adhere to a balanced diet and avoid excessive consumption of carbohydrates.
Why can't you trust advertising?
Gynecologists don't like advertising. Because gynecologists have to explain to young girls that thrush is a disease that needs to be treated, but the capsule does not cure. Explain that the capsule is not salvation or a panacea.
That it removes the symptoms, drives them inside for a while, after which the thrush comes back again and again, comes with every stress, with every cold, with every course of antibiotics taken. And this endless return of the disease leads to despair.
Women go to the gynecologist only when they completely cease to cope even with suppressing symptoms. Sad statistics - most patients try to solve the problem of thrush on their own until the last minute, and, as a rule, without success.
Resistance of the fungus
Any drug from the list of popular antifungal drugs can be resistant to the pathogen that caused thrush.
Causes
Treatment of candidiasis with the same medicine over a long period, with or without intervals.
Mechanism for developing resilience
The process is based on the ability of the fungus to adapt to the action of the drug, “get used to it,” and produce a generation of cells that the drug cannot kill. As a result, an effective medication, selected after inoculating the biomaterial for sensitivity, relieves severe symptoms after a certain number of applications, but is not able to destroy the infection.
What to do
- submit biological material (scrapings from the mucous membrane, skin) for analysis to determine the sensitivity of the fungus to the recommended medications;
- With the results, contact your doctor, he will review the regimen and prescription.
Sowing a smear onto a nutrient medium
Disadvantages of personal hygiene
Lack of personal hygiene is a common cause of chronic thrush.
Causes
- Using antibacterial soap and frequent vaginal douching or mouth rinsing.
- Lack of personal hygiene skills.
Mechanism of the problem
- With aggressive treatment with bactericidal agents and frequent douching, rinsing, and washing, beneficial microflora is washed out from the external and internal mucous membranes, dysbiosis, dysbacteriosis, and local immunity disorders develop, creating optimal conditions for the proliferation of Candida.
- Lack of personal hygiene skills leads to other extremes - the amount of fungus that gets on the mucous membranes and skin always exceeds acceptable standards; with a combination of factors, the pathogen quickly becomes pathogenic.
What to do
- Please discuss any procedures and cosmetics for intimate hygiene with your doctor.
- Observe basic rules of personal hygiene.
Intimate hygiene products should have a pH level of 4−5
Symptoms
Thrush can be easily recognized if certain symptoms are present:
- white or grayish discharge that looks like cottage cheese grains;
- formation of white dense plaque in the folds of the mucous membranes;
- itching and burning in the area affected by the fungal infection;
- pain during sexual intercourse;
- a feeling of increased humidity in the perineum (with vaginal candidiasis);
- sour smell.
The danger is represented by the chronic form of candidiasis, when the symptoms are less noticeable and sometimes absent, and the disease occurs only accompanied by cheesy discharge.
In most cases (except for candidiasis), the disease is recognized quite simply by its clear symptoms. This:
- Discharge of a lumpy structure, similar to curdled milk (white, white-gray);
- Plaque on the genitals;
- Very strong swelling of mucous membranes affected by thrush;
- A burning sensation that causes particular discomfort when urine comes into contact with infected areas when urinating;
- Discomfort during sexual intercourse, painful sensations that may persist for some time after sex;
- Unpleasant sour smell.
When the first symptoms appear, it is important to rush to the doctor so that the thrush does not drag on.
The symptoms of the acute form of thrush, which we just talked about, persist even when it becomes recurrent in nature. In this case, the disease appears four times a year or more. In the case of chronic thrush, symptoms may become muted. Manifestations may not be as bright, and some symptoms may be completely absent.
Under the constant influence of pathogenic flora, the genital organs themselves are somewhat modified. In women, erosions of the cervix may occur, and in men, the foreskin gradually begins to narrow (phimosis), and exposure of the head becomes difficult. The mucous membranes of the genital organs gradually change their bright pink color to brown.