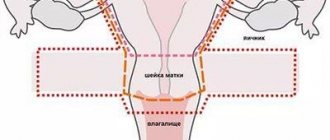
A mandatory stage of a gynecological examination is to assess the condition of the cervix. The cervix is the lower, narrow section of the uterus that connects its cavity to the vagina. Due to the peculiarities of the anatomical structure, pathologies especially often develop in this area. Many of them are dangerous to a woman’s life.
Cervical examination
To identify cervical diseases in the early stages and carry out effective treatment, it is necessary to regularly visit a gynecologist. Specialists at the Diana Clinic will conduct a comprehensive diagnosis of the cervical canal, make an accurate diagnosis and develop an effective treatment regimen.
Main objectives of the inspection
With regular visits to the gynecologist, diseases and pathologies of the development of the female reproductive organs can be detected at an early stage. Statistical data confirms that regular examinations reduce the risk of developing gynecological cancer pathologies.
The cervix is part of a woman's main reproductive organ, which is located in the vagina. It is shaped like a thick-walled cylinder with a small passage in the center. The passage is the cervical canal. During pregnancy, it closes and blocks the exit from the uterus. During childbirth, during contractions, its full opening is ensured, under the influence of the pregnancy hormone.
The cervix is also seen as a barrier that prevents bacteria from entering the uterus from the outside environment. The bacterial action is provided by the mucus formed in the cervical canal.
Attention! The cervix is an insensitive part of the organ, so diseases are often asymptomatic.
Girls often ignore the need to visit a doctor, arguing that various symptoms and pain are absent. At the same time, insidious women's diseases, including cancer, progress at lightning speed, leaving minimal chances for recovery and preservation of reproductive function.
How often should a woman visit a gynecologist?
A gynecological examination is necessary to prevent the development and control the course of female diseases. If there are no disturbing symptoms, the menstrual cycle is not disrupted, it is enough to undergo an examination once a year. If a patient is diagnosed with a disease, the doctor needs to monitor its progress, visiting the hospital at least once every six months, and more often if prescribed by the doctor.
The examination includes the following stages:
- Assessment of the condition of the external genitalia. The anus and labia are examined, the condition of the hair, skin, and mucous membranes is assessed.
- A bimanual examination is performed. The doctor inserts 2 fingers into the vagina and palpates the cervix through the anterior abdominal wall. This method allows you to detect tumors.
- The doctor conducts an examination in the mirrors.
Attention! Examinations during pregnancy are also carried out according to this scheme.
Indications for examination
A vaginal examination is carried out for the treatment and prevention of pathologies of the female reproductive system. If the patient has no complaints about her health, the event is carried out once a year; if pathologies are detected, the doctor may recommend going to the hospital more often.
The list of main indications for the examination includes:
- pregnancy – 38-40 weeks to control cervical dilatation;
- annual medical examination - the cervix does not have nerve endings, so pain during the development of diseases does not bother the patient, examination is the only available way to identify dangerous pathologies;
- constant disruption of the menstrual cycle is the main symptom indicating the development of serious disorders in the female genital organs;
- bleeding not associated with menstrual bleeding, changes in cycle length and abundance of discharge on menstrual days;
- impossibility of conception.
Gynecologists consider all women over the age of 30 to be at risk for developing cervical cancer. Achieving this milestone is a direct indication for an annual mirror examination. Women who have had cases of gynecological oncological pathologies in their family should pay special attention to the need for regular examination.
An unscheduled inspection is indicated in the following cases:
- spontaneous termination of pregnancy;
- abortion and medical termination of pregnancy;
- cauterization of erosion;
- natural birth or caesarean section.
In these cases, doctors recommend that the patient return for a consultation 2 months after the procedure.
How is the inspection carried out?
Many patients have a question: how does a gynecologist examine the cervix? This procedure is carried out according to the following algorithm:
- Stage 1 – Interview with the patient.
At the first stage, the gynecologist studies the woman’s medical record and records her complaints. The doctor asks questions about the nature of the menstrual cycle and sex life. The doctor must be informed about previous sexually transmitted infections and the presence of close relatives suffering from genital cancer. These are risk factors. - Stage 2 – Inspection of the cervix in the mirrors.
The initial examination of the cervical tissues is carried out using gynecological speculum. A sterile instrument is inserted into the vaginal lumen to visually inspect the walls of the cervical canal. At this stage, the doctor may suspect inflammation, erosion and pseudo-erosion, and detect tumors. - Stage 3 – Staining of the mucous membrane.
Next, the gynecologist applies Lugol’s solution to the mucous membranes of the cervix. This diagnostic method is called the Schiller test. Healthy cells absorb iodine well, acquiring a bright color. Pathological areas of tissue remain pale, since atypical cells do not absorb iodine. At this stage, the doctor can detect pathological areas even with the help of mirrors. - Stage 4 – Colposcopy.
Next, a special optical device – a colposcope – is inserted into the lumen of the cervical canal. This is a thin probe that allows you to visually examine the cervical walls for pathologies. The device magnifies the image several times so that the gynecologist can notice even minor changes in the mucous membrane. Carrying out colposcopy after the Schiller test is called extended colposcopy. - Stage 5 – Taking a smear for cytology.
A special spatula in the form of a brush is carefully inserted into the lumen of the cervical canal. This instrument is used to collect cervical epithelial cells. The resulting material is transferred to a glass slide and sent to the laboratory for microscopy. Cytological analysis reveals atypical cells. This is an important stage in the diagnosis of precancerous conditions and cancer. The smear also detects sexually transmitted infections. To do this, PCR diagnostics and bacterial culture are carried out. This is an important step in diagnosing HPV infection.
At all stages of diagnosis, the woman does not experience pain. If the doctor performs the manipulations carefully, the mucous membranes are not injured. However, after examination, the uterus may bleed for several days. This is considered a normal reaction to a smear test.
If pathological foci are determined based on the results of these studies, additional diagnostics may be prescribed:
- general and biochemical blood test;
- Ultrasound of the cervix;
- cervical biopsy.
Existing examination methods and technologies for their implementation
Annual preventive examination of the cervical canal and cervix includes the following activities:
- inspection in mirrors;
- bimanual examination;
- colposcopy.
Based on the results of the data obtained, the doctor can supplement the prescription. If oncology is suspected, a laboratory examination of the biopsy specimen is required. When identifying other diseases of the reproductive system, ultrasound is indicated.
Gynecological examination and procedure for conducting it
This method is a mandatory part of every gynecological examination. The method allows you to identify various changes occurring in the cervix. The inspection proceeds as follows:
- The woman takes off her clothes, puts a disposable diaper on the chair, takes a comfortable position and spreads her legs using supports.
- The gynecologist cleans your hands and puts on sterile gloves.
- The doctor spreads the labia and inserts a speculum into the vagina.
- After the dilator is inserted to the back wall of the vagina, it is opened and the cervix is examined.
- After the examination, the mirror is closed and removed.
The mucous membranes of the vagina are quite thin, so if the doctor does not follow the rules for working with a gynecological instrument, damage to its surface may occur, accompanied by bleeding. Mechanical injuries are not dangerous and do not pose a threat to women’s health; the healing period takes about 2-3 days. If the bleeding is severe, it is stopped by coagulation.
Attention! Injuries to the cervical canal and cervix can occur when using a rough brush to collect a smear.
Bimanual examination
Before the examination, the patient must empty her bladder. The assistant cleans the gynecological chair with a sterile rag, the woman takes off her clothes and lies down on a chair covered with a diaper. The legs are bent at the knee and hip joints and spread wide apart.
The doctor puts on sterile disposable gloves and inserts his right hand into the woman’s vagina, the left hand is placed on the stomach. The fingers of the doctor’s right hand are in the posterior fornix, and his left hand is in the direction of the sacrum. During the inspection, the following data is recorded:
- position of the uterus;
- sizes, shape;
- soreness;
- mobility and consistency of the cervix.
To examine the fallopian tubes and ovaries, the doctor moves the fingers of the right hand left and right (lateral fornix). The outer hand is placed in the ilioinguinal region. In the absence of pathologies, the appendages cannot be palpated.
The information obtained during the study is recorded by an assistant or nurse. After completing the examination, the doctor removes and throws away the gloves, washes his hands with soap and running water. The patient gets up from the chair, wipes the external genitalia with a napkin and gets dressed. After the examination, a conversation is held, during which the doctor gives an opinion on the state of health or prescribes additional examinations.
Attention! Bimanual examination techniques and speculum examination often complement each other during a full gynecological examination.
Colposcopy
Colposcopy is a method of examining the cervix and cervical canal using a special apparatus. The device allows you to detect the affected areas and displays an image on the screen. The doctor can evaluate the structure of the cervix and suggest the development of pathologies. The method provides differential diagnosis of neoplasms and allows you to take a smear or collect material for a biopsy.
In gynecological practice, there are 3 main types of colposcopy:
- Simple – indicative, carried out at the beginning of the examination. Allows you to evaluate the shape and size of the cervix, determines the condition of the external pharynx, color and structural features of the mucous membranes. Allows you to visualize the vascular pattern.
- Advanced - requires the use of special pharmacological solutions to assess structural changes in tissues at the cellular level. After treating the area with a special solution, swelling of the epithelial layer appears, the cells swell, and the intensity of the blood supply decreases due to contraction of the subepithelial vessels. Cells containing excess glycogen, after treatment with iodine-containing Lugol's solution, are painted a rich brown color; other tissues do not stain.
- Chromocolposcopy - upon examination, tissues are stained with hematoxylin solution.
Extended colposcopy and chromocolposcopy make it possible to distinguish normal mucous membranes from altered ones. The peculiarity of diagnostics is that pathologically altered cells are stained, but healthy ones are not. If a positive colposcopy result is obtained, the patient undergoes a biopsy. The advantage of the method is its safety and information content. Colposcopy is common because it has a limited method of contraindications.
Examination on a gynecological chair
Examination in a gynecological chair is a complex examination performed by a gynecologist to assess the condition of the external and internal genital organs.
The content of the article:
During the examination, the specialist assesses the condition of the vulva, anus, and perineum. The complex includes examination using mirrors, manual examination of the vagina (one-handed and two-manual), rectal, rectal-abdominal or rectal-vaginal in accordance with the indications.
The examination on the gynecological chair is carried out in a certain position: the patient assumes a reclining position, the buttocks are on the edge of the seat, the legs are bent at the knees and widely spread. In this case, the chair is equipped with special Hepel leg holders to fix the position of the patient, who should be in the most relaxed state.
The procedure requires sterility, so the specialist must use sterile gloves during the procedure. During the examination, smears are also taken for histological and cytological analyses. In the totality of all the manipulations performed, an examination on a gynecological chair, including taking smears, takes about 20 minutes.
The first stage of examination in a gynecological chair is a visual assessment of the condition of the external genitalia. The specialist evaluates the density of hair in the pubic area, the structure of the labia majora and minora, the condition of the glands of the vestibule, urethra, perineum of the inner femoral surface, and the anus area. Next, the specialist proceeds to examine the vestibule itself. To do this, the gynecologist separates the labia, examining the genital slit.
During the second stage of the examination, the specialist examines the vagina itself and the cervix. For this, the gynecologist needs to use specialized gynecological mirrors - self-supporting bicuspid Cusco mirrors and spoon-shaped mirrors, the size of which is selected individually.
The specialist spreads the labia with the thumb and index finger of the left hand. The speculum is inserted in a closed form longitudinally to approximately the middle of the vagina itself. For a detailed examination of the cervix, the mirror doors open. Thanks to this method, the gynecologist can examine the shape of the cervix (deformed, cylindrical, conical), examine the size of the uterus, and the color of the mucous tissues. Discharge from the cavity and mucous tissues is assessed. During such a study, the doctor can identify pathological processes of the uterus and cervix, for example, erosion, dysplasia, and so on.
In the third stage, the specialist conducts a one-handed examination. To do this, the doctor inserts the index and middle fingers of the right hand into the vagina. Sometimes only the index finger of the right hand can be used. This manual method is used to examine the perineum, urethra, vestibular gland, vaginal walls, cervix in the vaginal part, as well as the pelvic floor muscles.
Next, the specialist manually, using two hands, through the vaginal-abdominal or bimanual route, examines the uterus, appendages, tissue, and peritoneum of the pelvic area. During such a study, the position of the specialist’s hands and fingers is as follows: the fingers of the doctor’s right hand are in the vagina, while the left hand palpates the abdominal wall. During this process, the uterus is examined, its position, size, shape, mobility, pain, composition, then the uterine appendages are examined, the fingers are moved to the left and right walls of the pelvis. Palpation of the ovaries and fallopian tubes is not performed.
Vaginal examination is carried out in women who are sexually active. In order to preserve the integrity of the hymen, virgin patients are examined rectally or rectally-abdominally. Also, such methods of conducting research on a gynecological chair are used by a specialist for vaginal atresia, detection of tumor tumors or inflammatory processes in a patient. When examining the posterior wall of the vagina and the anterior wall of the rectum, the rectal-vaginal method is used (the index finger is inserted into the vagina, the middle finger of the right hand is inserted into the rectum).
As for the sensations that the patient may experience during the examination, they may be somewhat painful and cause some discomfort. An examination in a gynecological chair should be carried out at least twice a year during the prevention of various diseases, inflammatory processes and pathological phenomena, for example, neoplasms. Experts categorically do not recommend neglecting this examination, since many gynecological diseases may not manifest themselves in any way, reaching a critical stage.
In every clinic in Moscow and the Moscow region where there is a gynecologist’s office, the patient is examined using a gynecological chair. Contact details, location of the clinic, as well as the cost of this service can be found on our website.
What diseases are diagnosed during examination of the cervix
The list of pathologies detected during a gynecological examination includes:
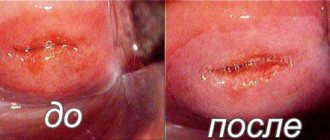
- Erosion is damage to the mucous membrane. When examined in the mirrors, the doctor sees areas of redness. The diagnosis is confirmed by colposcopy. Treatment is conservative.
- Cyanosis is the blueness of the cervix, which is the result of active production of progesterone.
- Polyps are detected on the surface during a gynecological examination and bimanual examination.
- Oncological neoplasm. During the initial examination, the doctor sees signs of damage, but other examinations are needed to confirm the diagnosis. If the disease is detected at an early stage, the patient has a chance of full recovery.
Attention! Periodic gynecological examination is the main link that ensures early diagnosis and effective treatment of various female diseases.
Features of examination during pregnancy
If there is a delay in menstrual bleeding, if its duration exceeds 1 week, the woman should consult a gynecologist. Such deviations, with a stable cycle, indicate a probable pregnancy.
The examination technique in this case does not differ from a regular preventive examination. The doctor pays attention to the color of the cervix - under the influence of the hormone it turns blue, takes smears and assesses the condition of the internal os. When inflammatory changes are detected, treatment of the disease is provided. Biopsy and other diagnostic methods are used if absolutely necessary.
At 38-40 weeks, the doctor conducts an examination to assess the dilatation of the cervix. This condition is the main point ensuring natural delivery. If the pharynx remains closed until 41 weeks, stimulation of labor is indicated due to the risk of post-term pregnancy.