Types of disease
Ovarian hypoplasia differs in the time of occurrence - congenital (appears together with disruption of the renal system and many other diseases) or acquired during life. Congenital ovarian disease can also be combined with uterine hypoplasia. Depending on the type of lesion, the disease can be: central (the connection between the hypothalamus and the pituitary gland is disrupted), peripheral (damage to the ovaries) and idiopathic. Over time, the disease develops, the ovaries decrease in size, the number of follicles decreases and the ability to reproduce is impaired.
Essence of the disease
In general, ovarian hypoplasia is the underdevelopment of the ovaries, which are the female sex glands. Such a defect may be expressed as an anatomical or functional abnormality caused by structural abnormalities. Pathology can occur during the period of intrauterine development of the fetus, in childhood during ontogenesis or during puberty.
Ovarian hypoplasia, as a rule, is accompanied by sexual infantilism, and quite often, underdevelopment of some other organs is simultaneously recorded: the uterus, vagina, and kidneys. This defect is expressed in the abnormal development of the follicular layer, up to a state where primary eggs and primordial follicles are not detected at all. Another common option is the presence of primary eggs, but their maturation is stopped at an early stage.
Cases have been recorded when hypoplasia is associated with gonadal genetic pathologies associated with a violation of the properties and number of sex chromosomes, for example Shereshevsky-Turner syndrome. With this development mechanism, ovarian tissue (parenchyma) is almost completely replaced by connective tissue.
We recommend learning: How ovarian massage is performed in women
Possible causes of the disease
The congenital form is a dysfunction of the pituitary gland and hypothalamus. The occurrence of the disease depends on the impact of negative factors on the female body in the womb. Therefore, when serious changes occur in the mother during pregnancy, the likelihood of a congenital form of the disease in the fetus increases. Congenital causes of hypoplasia:
- disruption of follicular development;
- chromosome abnormalities;
- genetic predisposition (for example, gonadal dysgenesis - a disease that is caused by chromosome pathology).
- infectious diseases of the genital organs;
- surgical operations, abortions;
- eating disorders (intoxications) causing anorexia;
- the presence of high levels of radiation in the place of residence;
- the presence of high levels of radiation in the place of residence;
- the occurrence of infections in children;
- disruption of the endocrine system;
- heredity;
- tumors;
- inflammation of the ovaries or uterus.
Causes
When talking about genital infantilism, doctors mean the underdevelopment of several organs of the female reproductive system. This clinical situation is usually congenital. The formation is usually based on chromosomal pathology. A striking example is Shereshevsky-Turner syndrome with hypoplasia of the appendages and uterus.
The ovaries are formed in a girl’s body during intrauterine development. This process is completed by the time of puberty. The following unfavorable factors can affect the formation and proper formation of a girl’s gonads in utero:
- Infectious diseases suffered by a mother or girl are already in the process of ontogenesis. Rubella is especially dangerous, since the causative agents of this infection are tropic to the epithelium of the internal genital organs.
- Eating disorder. For example, the occurrence of anorexia nervosa, bulimia, constitutional obesity.
- Toxic effects of alcohol, nicotine, medications.
- Inflammatory diseases of the ovaries, uterus, appendages in the mother.
Ovarian hypoplasia is often caused by thyroid dysfunction. In Russia, many regions and areas are endemic for thyroid goiter. The level of iodine intake is catastrophically low. As a result, the function of the gland suffers. This invariably affects all parts of the hypothalamic-pituitary system, including the appendages.
Important! That is why one of the important examinations for suspected ovarian pathology is to determine the thyroid profile.
Experienced emotional stress is discussed among the possible causes of structural or functional imperfection of the ovarian apparatus. This group of factors should include mental pathologies, organic pathology of the pituitary gland and hypothalamus, including various types of tumors.
Bad habits and unhealthy diet are important factors that can become key in the development of the described pathology. This applies to both the girl’s mother and the patient herself.
Symptoms of the disease
The pathology is very easy to notice because the disease occurs without symptoms for a short time. Unfortunately, it is impossible to detect the presence of the disease before the onset of puberty. Ovarian pathology is accompanied by symptoms:
- late onset of menstrual flow;
- inability to get pregnant;
- secondary sexual characteristics are poorly expressed.
This symptomatology most characterizes the disease before the onset of puberty (congenital form). An ultrasound scan will reveal elongated fallopian tubes and impaired uterine development in the girl.
With the acquired form of female hypoplasia, menstruation ceases. When examined on a gynecological chair, vaginal dryness can be detected, which is not normal.
Additional signs that indicate the presence of hypoplasia of the left or right ovary may appear as:
- narrowness of the vagina;
- increased thinness of the labia;
- disorders of genital plasticity.
Symptoms
Manifestations of structural or functional incomplete development of the ovaries depend on the form of the pathology. Congenital hypoplasia of the organ leaves its mark not only on the structure of the genitals, but also on the shape of the skeleton, physique, and characteristics of mental development.
Girls with underdeveloped ovaries are characterized by a female body type. But at the same time, some features of eunuchoidism can be traced:
- Flattened mammary glands with underdeveloped nipples.
- Male hair type.
- Narrow pelvis and wide shoulder girdle.
- Weak secondary sexual characteristics.
With congenital ovarian hypoplasia, one of the important symptoms of functional failure is primary amenorrhea. That is, during puberty, prepuberty and after it, the girl does not menstruate. Along with this, they have no sex drive.
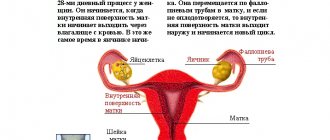
The structure of internal organs may differ. The uterus and ovaries decrease in size. The fallopian tubes are thinner and longer, which is also obvious during ultrasound examination.
When ovarian hypoplasia was not formed in utero, but in a later period, manifestations can manifest themselves already in reproductive age. Therefore, the first symptom is infertility. The second important complaint is changes in the menstrual cycle. This is most often secondary amenorrhea, when menstruation previously occurred on time, but has now stopped.
Attention! Any changes in the menstrual cycle are a reason to immediately consult a doctor.
Ovarian hypoplasia, like other reproductive pathologies, is progressive. Menstruation can be very painful. This condition is called algodismenorrhea. Hypomenstrual syndrome is manifested by a decrease in the volume of blood released and a decrease in the duration of menstruation.
Diagnosis
Diagnostic measures are carried out using a gynecological chair. The doctor pays attention to:
- examination of the genital organs;
- palpation. In girls, this method is performed through the rectum;
- examination for the presence of mucus.
If a disease is suspected, the doctor refers the woman for examination. It consists in:
- Ultrasound of the reproductive system.
- Blood test for hormones. If ovarian hypoplasia is found in a girl, it may be a congenital form.
- X-ray.
In the presence of a severe form, an ovarian biopsy or laparoscopic diagnosis may be necessary.
Preventive measures and prognosis
Factors that could negatively affect the development of pregnancy should be immediately eliminated. For the purpose of prevention, the child should be provided with a balanced diet and vaccinated against various infections on time. Avoid hypothermia.
Prognosis after undergoing ovarian hypoplasia
Many women are interested in the likelihood of conceiving after an illness. Statistics show that the chances of getting pregnant and having a child range from 30 to 60%. You need to plan conception under the supervision of doctors (usually a gynecologist and endocrinologist). Moreover, a woman or girl should prepare in advance for a possible termination of pregnancy. There is also a possibility of multiple pregnancy.
Ovarian hypoplasia that appears in a woman does not cause discomfort until she thinks about conceiving and having a child. Having a disease is not a death sentence for an impossible pregnancy. Well-chosen treatment restores the functioning of the genital organs and allows pregnancy to occur.
Ovarian hypoplasia
Ovarian hypoplasia is an anatomical and functional underdevelopment of the female gonads - the ovaries. With ovarian hypoplasia, hypomenstrual syndrome or amenorrhea, decreased libido, and infertility are observed. Ovarian hypoplasia is diagnosed through a general and gynecological examination, ultrasound results of the pelvic organs, hormonal studies, laparoscopic ovarian biopsy, and determination of the karyotype (chromosome set). Treatment of ovarian hypoplasia requires cyclic hormonal therapy.
Treatment of uterine hypoplasia
If an “accidental discovery” occurred at the very beginning of your journey to a baby, do not despair and do not rush, observe the dynamics of changes in the size of the uterus during the cycle, track the presence of ovulation, the correspondence of the size of the endometrium and its condition to the phase of the cycle. It is quite possible that there was a measurement error, or the small size of the uterus is your individual anatomical feature.
If you have previously been diagnosed with sexual genital infantilism or the size of the uterus and the condition of the endometrium does not meet the norm even after repeated examination, the doctor may prescribe hormonal therapy with estrogen and progesterone. The goal of this treatment is to enlarge the uterus to normal size and restore ovulatory cycles and normal cyclic changes in the endometrium.
If the diagnosis is confirmed, you should not refuse treatment. With uterine hypoplasia, the risk of ectopic pregnancy, early miscarriage, weak labor and atonic postpartum hemorrhage increases.
General information
Ovarian hypoplasia is more often observed against the background of general or sexual infantilism; can be combined with uterine hypoplasia, aplasia of the uterus and vagina (Rokitansky-Kustner syndrome), kidney hypoplasia, and underdevelopment of other organs. In addition, ovarian hypoplasia occurs with gonadal dysgenesis - genetic diseases caused by qualitative and (or) quantitative pathology of sex chromosomes (Shereshevsky-Turner syndrome, etc.). In these cases, the ovarian parenchyma is represented predominantly or exclusively by connective tissue.
Acquired ovarian hypoplasia is a consequence of adverse effects on the body during ontogenesis, especially in childhood or puberty. The development of ovarian hypoplasia can be promoted by inflammation of the gonads (oophoritis, adnexitis), abortion, nutritional disorders (hypovitaminosis, anorexia), chronic intoxication, childhood infections (mumps, rubella, measles, scarlet fever, etc.), tonsillitis, endocrinopathies (inflammatory lesions of the pituitary gland and hypothalamus, pituitary adenoma, prolactinoma, hypothyroidism, etc.), exposure to radioactive substances. Less commonly, ovarian hypoplasia is caused by intrauterine damage to the follicular apparatus due to pregnancy pathology in the mother.
In accordance with the etiology and level of damage, gynecology distinguishes ovarian hypoplasia of central (hypothalamic-pituitary) origin; peripheral (ovarian) genesis and idiopathic (unclear) origin. With hypoplasia in the ovaries, there is a decrease in the severity of the follicular layer. In hypoplastic ovaries, primary egg cells and primordial follicles may not be present at all or there may be a cessation of their maturation and growth, which determines the picture of clinical manifestations.
How to determine underdevelopment of the ovaries? Diagnostics and therapy
Ovarian hypoplasia is an anatomical and functional deviation that causes disturbances in the reproductive system and increases the risk of developing tumors. A specialized system of therapeutic measures in combination with prevention helps to cure and prevent severe complications.
What it is?
With ovarian hypoplasia in women, the gonads develop poorly. This deviation is formed in the womb, in infancy or during puberty. Often, hypoplasia indicates genital infantilism and is accompanied by insufficient development of the uterus, aplasia (complete or partial absence) of the vagina and changes in other organs of the genitourinary system.
As the pathology progresses, the size of the gonads decreases, the follicular layer becomes thinner (the follicles are transformed into connective tissue).
Types of ovarian underdevelopment
Hypoplasia can be acquired or congenital and is classified according to its forms into central (hypothalamic-pituitary), peripheral (ovarian) and idiopathic (of unknown origin).
A congenital disorder is caused by abnormalities of the sex chromosomes, the development of which is facilitated by negative environmental factors affecting the mother’s body. Acquired appears as a result of the harmful influence of external factors on the child.
Causes
The causes of acquired ovarian hypoplasia can be:
- infections suffered in childhood (rubella, mumps, scarlet fever, mumps, measles);
- intoxication of the body;
- radiation exposure;
- diseases of a hormonal nature (adenoma, hypothyroidism, etc.);
- infection in the pelvic organs;
- inflammation of the gonads (oophoritis, adnexitis);
- angina;
- a tumor located near the pituitary gland or hypothalamus, as well as inflammatory lesions in this area;
- unbalanced diet (diet, anorexia, hypovitaminosis, starvation, overeating).
Symptoms of the disease
The first alarming symptom of ovarian hypoplasia is considered to be hypomenstrual syndrome (small volumes of discharge, reduction and decrease in the duration of menstruation), as well as the absence of:
- menstrual flow for several cycles;
- menstruation until 15-16 years of age;
- ovulation during a normal menstrual cycle.
Another component of the clinical picture of the disease is eunuchoid syndrome.
This anomaly is characterized by a late onset of menstruation, lack of armpit and pubic hair, arrest in the development of the external genitalia, skeletal disproportion, narrowness of the vagina, decreased sexual desire, frigidity, weak pigmentation of the skin of the labia, insufficient expression of nipple areolas and other secondary sexual characteristics.
Treatment
Treatment of ovarian hypoplasia is aimed, first of all, at normalizing hormonal levels and restoring reproductive function for a further successful pregnancy. Hormone therapy takes place in 2 stages:
- At the first stage, the level of estrogen increases, due to which the menstrual cycle evens out and a menstrual-like reaction (bloody discharge) appears.
- At the second stage, the processes of the hypothalamic-pituitary connection are stabilized, the relationship between the uterus and appendages is restored, and the functioning of the pelvic organs is restored. At the same time, folliculometry (ultrasound of the ovaries) is performed. This allows you to track the dynamics of changes in the patient’s body.
If hormone therapy does not produce the desired results, a 10-day break is taken, and then treatment is resumed.
In addition to hormonal therapy, measures are taken that will help eliminate unpleasant symptoms and strengthen the immune system.
For this purpose, vitamin therapy is used (vitamins should be consumed in their natural form and in tablet form), physiotherapy, gynecological massage and balneotherapy (treatment with mineral waters).
Timely hormone therapy increases the chance of getting pregnant by 60%.
Physiotherapy
Physiotherapy is an integral part of the treatment process. Positive dynamics can be achieved by:
- ultraphonophoresis or electrophoresis;
- gynecological massage;
- magnetic therapy;
- laser therapy;
- Magnetic laser therapy.
Attention! These procedures must be carried out strictly as prescribed by the doctor!
Symptoms of ovarian hypoplasia
Patients with ovarian hypoplasia may experience various disorders of menstrual function - primary, sometimes secondary amenorrhea, algomenorrhea or hypomenstrual syndrome, anovulatory cycle. The listed disorders in ovarian hypoplasia are accompanied by infertility.
The patients are built according to the female type, but have slightly pronounced eunuchoid features. With ovarian hypoplasia, secondary sexual characteristics are usually weakly expressed - there is scanty hair on the pubis and in the armpits, flattening of the mammary glands, and lack of expression of the areolas and nipples. Characteristic is the absence of the first menstruation (menarche) by the age of 15-16 years. Sexual desire in women is reduced, and frigidity is often observed. Other signs of ovarian hypoplasia are detected during a comprehensive gynecological examination.
Ovarian hypoplasia: what it is, symptoms, treatment
Ovarian hypoplasia is an obstacle to conceiving a child, and there is also a risk of developing tumor formations, so women with this diagnosis should be under constant supervision of a gynecologist and endocrinologist.
Hypoplasia is underdevelopment of the female gonads. It manifests itself in prenatal development or during puberty. In some cases, it occurs in adulthood after gynecological diseases.
Types of disease
Depending on the time of occurrence, hypoplasia can be congenital or acquired. In congenital pathology, there is a combination of the disease with uterine aplasia, underdevelopment of the kidneys and other organs, Shereshevsky-Turner syndrome, etc. In these cases, the epithelial layer of the ovaries is represented mainly by connective tissue.
Depending on the type of lesion, hypoplasia is distinguished into central, peripheral and idiopathic forms. In central cases, the disorders are associated with the pituitary gland and hypothalamus; in peripheral cases, the lesion initially occurs in the ovaries themselves; in idiopathic cases, the origin of the disease is not clear.
Causes
| No. | Congenital | Purchased |
| 1. | Violation of the development of the follicular apparatus | Infectious and inflammatory diseases of the pelvic organs (adnexitis, salpingoophoritis) |
| 2. | Abnormal chromosome set | Surgical interventions, including artificial termination of pregnancy |
| 3. | Gonado-genetic pathologies | Eating disorders that cause anorexia, vitamin deficiency |
| 4. | Radiation exposure, living in areas with high levels of radiation | |
| 5. | Childhood infections (rubella, measles, scarlet fever) | |
| 6. | Endocrine pathologies (pituitary adenoma, inflammatory process in the hypothalamus, hypothyroidism, etc.) | |
| 7. | Hereditary factor |
Symptoms
Clinical manifestations of ovarian hypoplasia are quite striking, most often beginning during puberty:
- Lack of periods (amenorrhea) in adulthood. In girls during puberty, menstruation may not come until 16-17 years of age,
- absence of ovulation, when the dominant follicle matures, but no egg is released.
- decreased libido and frigidity,
- weakly expressed secondary sexual characteristics - sparse pubic and armpit hair, underdevelopment of the mammary glands,
- hypomenstrual syndrome - infrequent periods with scanty discharge.
Diagnostics
Diagnostic measures are carried out comprehensively and include the following studies:
- Collect symptoms and study anamnesis. Already based on the primary symptoms and appearance of the patient, an experienced doctor may suspect ovarian hypoplasia.
- An examination in a gynecological chair allows you to determine the small size of the vagina and its poor extensibility, the pale color of the skin of the labia.
- An ultrasound shows the infantility of the uterus and ovaries (their small size), thin and elongated fallopian tubes. Also, follicles are not visible on the appendages, even if an ultrasound examination is performed in the second half of the cycle.
- Blood test to determine the amount and ratio of hormones. As a rule, with this disease there is a decrease in the amount of FSH (follicle-stimulating hormone), progesterone, and estrogen.
- Magnetic resonance imaging of the brain to exclude or confirm abnormalities in the pituitary gland and hypothalamus.
After excluding other diseases and making an accurate diagnosis, the doctor prescribes treatment.
How to eliminate ovarian hypoplasia
Treatment of pathology is aimed primarily at restoring hormonal levels, ovulation and normalizing menstruation. A woman is prescribed hormones to create an estrogen level. When the menstrual cycle becomes regular, the drugs are replaced with medications that normalize ovarian function and endocrine processes.
Cyclic vitamin therapy is often used: B, A, E, C. You need to take them in a course of 3 months with an interval of 1 month. The exact dosage is determined only by a gynecologist, taking into account the patient’s age, the course of the disease and the individual characteristics of the body.
When taking hormonal drugs and vitamins, patients not only restore menstruation, but also develop secondary sexual characteristics, and the figure takes on a more feminine shape.
In addition to drug treatment, physiotherapy has proven itself well. Thus, a magnet, laser, ultraphonophoresis, electrophoresis and other procedures are prescribed that trigger metabolic processes and restore impaired ovarian function.
Among the non-traditional methods used are gynecological massage, acupuncture, balneotherapy (sea water treatment), and mud therapy.
Prevention and prognosis
Preventive measures are used only for secondary acquired hypoplasia, since in the case of a congenital anomaly, prevention is meaningless.
Measures to prevent the disease include timely treatment of infectious and inflammatory pathologies, a healthy balanced diet and regular exercise to prevent the occurrence of stagnation in the pelvis.
The probability of pregnancy in women with congenital or acquired hypoplasia ranges from 30% to 60%, i.e. this disease is reversible and only in exceptional cases causes persistent infertility. The response to hormonal therapy is usually high.
In case of a negative result of treatment, in vitro fertilization (IVF) is possible. Unfortunately, with this disease, even with a possible pregnancy, there is a high risk of miscarriage and frozen pregnancy.
In this case, they resort to surrogacy.
Loading…
Source: https://kazandoctor.ru/ginekologiya/zabolevaniya/simptomy-i-lechenie-gipoplazii-yaichnikov
Diagnosis of ovarian hypoplasia
During a gynecological examination, attention is drawn to the hypoplastic structure of the external genitalia, thin, non-pigmented labia minora, the presence of a narrow, inextensible and short vagina, and the infantility of the uterus. When performing an ultrasound, ultrasound hysterosalpingoscopy or hysterosalpingography, a decrease in the size of the ovaries and uterus is confirmed, tortuous, thin, elongated fallopian tubes are determined.
Basal temperature is monophasic. Examination of cervical mucus in ovarian hypoplasia reveals signs of hypoestrogenism - a negative or mild “pupil” symptom. Low levels of estrogen (in some cases, gonadotropic hormones) are confirmed by laboratory blood tests. A progesterone test for ovarian hypoplasia usually gives a negative result, indicating severe estrogen deficiency. The combined estrogen-gestagen test is positive, which indicates the functional safety of the endometrium.
To identify the central form of ovarian hypoplasia, they resort to pharmacological tests with menopausal human gonadotropin, human chorionic gonadotropin, clomiphene, luliberin; performing radiography of the sella turcica, MRI of the brain. If necessary, diagnostic laparoscopy and ovarian biopsy are performed.
Diagnostics
Diagnostic measures are carried out comprehensively and include the following studies:
- Collect symptoms and study anamnesis. Already based on the primary symptoms and appearance of the patient, an experienced doctor may suspect ovarian hypoplasia.
- An examination in a gynecological chair allows you to determine the small size of the vagina and its poor extensibility, the pale color of the skin of the labia.
- An ultrasound shows the infantility of the uterus and ovaries (their small size), thin and elongated fallopian tubes. Also, follicles are not visible on the appendages, even if an ultrasound examination is performed in the second half of the cycle.
- Blood test to determine the amount and ratio of hormones. As a rule, with this disease there is a decrease in the amount of FSH (follicle-stimulating hormone), progesterone, and estrogen.
- Magnetic resonance imaging of the brain to exclude or confirm abnormalities in the pituitary gland and hypothalamus.
After excluding other diseases and making an accurate diagnosis, the doctor prescribes treatment.
Treatment and prognosis of ovarian hypoplasia
For ovarian hypoplasia, treatment aims to restore hormonal and reproductive functions. The basis of therapy for ovarian hypoplasia is cyclic hormone therapy. At the first stage, hormone therapy is aimed at creating an estrogen background, and after the appearance of a menstrual-like reaction, at normalizing the cyclic hypothalamic-pituitary-ovarian-uterine processes. Hormone therapy is carried out under the control of folliculometry. At the same time, for ovarian hypoplasia, vitamin therapy, physiotherapy (magnetic therapy, magnetic laser therapy, laser therapy, ultraphonophoresis, etc.), gynecological massage, and balneotherapy are prescribed.
Under the influence of hormone therapy, characteristic female sexual characteristics develop. Women with ovarian hypoplasia should be observed by a gynecologist-endocrinologist for timely detection of hypothalamic-pituitary tumor processes and hyperplastic disorders in the reproductive system under the influence of hormone therapy.
When inducing a two-phase menstrual cycle in patients with ovarian hypoplasia, the chances of pregnancy range from 30 to 60%; However, the possibility of developing a multiple pregnancy cannot be excluded. With deep ovarian hypoplasia, motherhood is possible thanks to assisted reproductive technologies - IVF using a donor egg. Embryos obtained through artificial insemination (by ICSI, PIXI or IMSI) are frozen (embryo cryopreservation), and then cryopreservation is carried out and the embryos are implanted into the uterus. If necessary, a donor embryo can be used. The course and management of pregnancy in patients with ovarian hypoplasia is associated with risks of miscarriage. In such cases, they resort to surrogacy.
How to eliminate ovarian hypoplasia
Treatment of pathology is aimed primarily at restoring hormonal levels, ovulation and normalizing menstruation. A woman is prescribed hormones to create an estrogen level. When the menstrual cycle becomes regular, the drugs are replaced with medications that normalize ovarian function and endocrine processes.
Cyclic vitamin therapy is often used: B, A, E, C. You need to take them in a course of 3 months with an interval of 1 month. The exact dosage is determined only by a gynecologist, taking into account the patient’s age, the course of the disease and the individual characteristics of the body.
When taking hormonal drugs and vitamins, patients not only restore menstruation, but also develop secondary sexual characteristics, and the figure takes on a more feminine shape.
In addition to drug treatment, physiotherapy has proven itself well. Thus, a magnet, laser, ultraphonophoresis, electrophoresis and other procedures are prescribed that trigger metabolic processes and restore impaired ovarian function.
Among the non-traditional methods used are gynecological massage, acupuncture, balneotherapy (sea water treatment), and mud therapy.
Ovarian hypoplasia
Ovarian hypoplasia is a pathology that is represented by a violation of the structure of the female reproductive organs - the ovaries. With this anomaly, functional or structural underdevelopment of the ovaries is observed. Often this disorder is an expression of genital infantilism. It is for this reason that pathology is often associated with such disorders as vaginal aplasia, endometrial hypoplasia, uterine hypoplasia, polycystic ovaries and other types of underdevelopment of the genital organs. In addition, the disorder is a consequence of various genetic pathologies that are directly related to sex chromosomes.
How does ovarian hypoplasia manifest in women?
Regardless of the type of ovarian damage and the causes of the pathology (hypoplasia of peripheral, central or idiopathic origin), the main sign of underdevelopment of the reproductive glands is menstrual dysfunction.
Disorders of the menstrual cycle can be manifested by the following pathological abnormalities:
- amenorrhea (depending on the nature of the damage to the glands, the absence of menstruation can be primary or secondary);
- anovulatory cycle (lack of ovulation);
- hypomenstrual syndrome (reduced duration, decreased menstruation, decreased amount of menstrual flow).
In addition, in patients suffering from ovarian hypoplasia, a number of eunuchoid manifestations are observed:
- disproportionate skeletal structure;
- delay in the formation of genitals;
- later menarche (first menstruation);
- complete absence or presence of mild secondary sexual characteristics.
During a gynecological examination, the doctor may detect the following internal manifestations of ovarian hypoplasia:
- narrowness of the vagina;
- thinness of the labia minora;
- hypoplasticity of the external genitalia;
- lack of pigmentation on the labia.
If hypoplasia of multifollicular ovaries occurs in combination with hypoplasia of the uterus, a decrease in estrogen production (hypoestrogenism) and underdevelopment or non-standard structure of the uterus are observed: the fallopian tubes are elongated, the size of the uterine body is reduced. Also, the combination of these pathologies is accompanied by the absence of an increase in mucus in the cervical canal before ovulation (negative “pupil” symptom).
Predictions for this violation
Women who have even been diagnosed with hypoplasia of the right or left ovary are interested in what the chance of successful conception is after treatment. The chances are small, but still there: from thirty to sixty percent. However, in order for the outcome to be favorable, it is necessary to promote the establishment of a two-phase menstrual cycle.
Pregnancy should be planned following medical recommendations. Ideally, you need to be observed by a gynecologist and endocrinologist. Among the main risks are miscarriage and multiple pregnancies.
A woman may be recommended to use assisted reproduction technologies.
Manifestations of ovarian hypoplasia
Before we begin to describe the symptoms, it is worth defining their forms:
- Unexplained genesis;
- Hypothalamic-pituitary or central origin.
Hypoplasia of any type manifests itself primarily in the form of disruption of the regular menstrual cycle:
- Amenorrhea (based on the type of lesion, primary or secondary is distinguished);
- Hypomenstrual syndrome;
- Anovulatory cycle.
In patients with this pathology, eunuchoid signs are clearly expressed:
- Late onset of menstruation;
- Weakly expressed or completely unexpressed secondary sexual characteristics;
- Incorrect skeletal proportions;
- Developmental disorders of the reproductive organs.
Among the internal characteristic signs of ovarian hypoplasia that are identified during an examination by a gynecologist are:
- Low plasticity of the external genitalia;
- Narrow vagina;
- Thin labia minora with no pronounced pigmentation.
With a combination of uterine and ovarian hypoplasia, the patient experiences abnormal uterine structure and hypoestrogenism:
- Fallopian tubes are too long;
- Reduced body volume;
- No increase in mucus in the cervical canal of the uterus immediately before ovulation. This pathology is also called negative pupil syndrome.
In general, the uterus may be underdeveloped.
Ovarian hypoplasia | University Clinic
Hypoplasia of the ovaries is a reduction in their size, which often disrupts the production of sex hormones. Pathology that occurs in the prenatal period, childhood and adolescence accompanies a woman throughout her life.
Signs of the disease most often appear during puberty or later. The patient notices menstrual irregularities, decreased libido and infertility.
Congenital hypoplasia - why intrauterine ovarian underdevelopment occurs
Ovarian hypoplasia
Such a pathology that arose before birth is called primary. The ovaries are formed in the second month of pregnancy, so any illness of the mother during this period can negatively affect the development of the unborn girl. Most often, the cause of fetal ovarian hypoplasia is various infections that the pregnant woman has suffered.
The second stage of development of a girl’s ovaries occurs at 20 weeks. During this period, interstitial tissue is laid, which will become the basis of future organs, and follicles in which the eggs necessary for fertilization and pregnancy will mature.
This process is affected by maternal illnesses, poisoning, infections, increased background radiation and unfavorable ecology in the place of residence.
Primary hypoplasia can be caused by chromosomal abnormalities. In this case, gonadal dysgenesis develops - a condition in which a connective tissue gonadal cord is formed instead of the ovaries. As an adult, such a woman does not have primary sexual characteristics, she does not have menstruation and experiences primary infertility.
A distinctive feature of congenital pathology is its complex nature. Ovarian hypoplasia is often combined with impaired development of the uterus, oviducts, bladder, and external genitalia.
Ovarian underdevelopment that occurs in utero is unilateral. With this pathology, only hypoplasia of the left or right ovary is observed. In this case, it is possible to maintain menstrual function and achieve pregnancy.
Incorrect development of a girl’s genital organs, initiated in utero, will affect sexual and reproductive function in adulthood. Fortunately, modern medicine can correct many forms of this disease.
Types of ovarian hypoplasia
Acquired hypoplasia - the dangers of childhood infections and teenage anorexia
Violation of ovarian development can also occur after the birth of a girl. This often occurs between 5 and 8 years of age, when the next phase of ovarian formation begins. Hypoplasia can occur due to a lack of vitamins, poor nutrition, metabolic disorders, hormonal imbalances, and severe concomitant diseases.
The girl has mumps
Ovarian development is negatively affected by childhood infections, especially mumps (mumps), which affects various glands, including the ovaries. Therefore, the opinion that mumps is dangerous only for boys is completely wrong. In girls, the disease causes no less serious consequences.
The formation of the ovaries can also be disrupted during adolescence. The reason is the inflammatory process in them and the girl’s passion for strict diets, which deprive the teenager’s body of vitamins and microelements. In this case, the ovaries stop in their development and their hypoplasia occurs.
Underdevelopment can occur due to traumatic brain injuries, accompanied by damage to parts of the brain - the hypothalamus and pituitary gland, which are responsible for hormonal function. In this case, hormones that stimulate the development of ovarian tissue cease to be produced, and this pathology is formed.
Therefore, for a woman who comes in adulthood with complaints of infertility, sexual and menstrual dysfunction, the doctor must clarify the characteristics of childhood and adolescent development, past illnesses and injuries. The cause of adult problems can be banal mumps or teenage anorexia.
Symptoms of hypoplasia
This disease is almost never registered in childhood, since outwardly a girl with this disorder does not differ from her peers. The exception is severe hereditary pathologies, in which, in addition to impaired ovarian development, other external anomalies are observed.
The disease is first registered more often in adolescence. The girl has no menstrual cycle or has infrequent, short, scanty menstruation. With significant hormonal imbalances, the growth of the mammary glands may be disrupted and typical female pubic and axillary hair may be absent.
In most cases, the disease manifests itself during the reproductive period, when a woman consults a gynecologist with complaints of infertility. Sometimes there are habitual miscarriages caused by a lack of hormones.
The disease is often accompanied by menstrual irregularities. Patients experience rare, scanty, painful menstruation. When ovarian hypoplasia and endometrium, the inner layer of the uterus, are combined, amenorrhea occurs—the absence of menstrual periods.
Unilateral ovarian damage may be asymptomatic. Pathology is detected during a routine ultrasound of the ovaries.
Diagnosis of ovarian hypoplasia
Ultrasound of the ovaries
Severe forms of the disease, leading to pronounced hormonal imbalance, are detected during a gynecological examination. A woman experiences underdevelopment of the external genitalia, and sometimes the mammary glands.
Milder forms of pathology are diagnosed only during a pelvic ultrasound. An ultrasound examination reveals underdeveloped ovaries, the sizes of which differ from the norm.
Normal ovarian parameters:
- Length – from 2 – 3.8 cm.
- Height – 1.8 – 3.0 cm.
- Depth –1.5 – 2.2 cm.
The smaller the size of the ovaries, the brighter the manifestations of the disease and the worse the prognosis in terms of pregnancy and childbirth.
Often, parallel underdevelopment of the uterus, fallopian tubes, bladder, kidneys and ureters is recorded. In this case, an ultrasound examination of the genitourinary system will be required.
An examination is carried out for the patency of the fallopian tubes, which may be thin, tortuous and obstructed. For this purpose, UZGSS is used. Liquid is pumped into the tube lumen, the movement of which is recorded using ultrasound.
It shows keeping a graph of basal temperature measured in the morning with a rectal thermometer. With ovarian hypoplasia, ovulation does not occur, so the graph is monotonous. There is no drop in temperature in the middle of the cycle and no rise after the egg leaves the ovary.
With folliculometry - ultrasound monitoring of follicle maturation - it is discovered that during the menstrual cycle they do not mature and ovulation does not occur.
Along with uterine hypoplasia in women with this pathology, multifollicular ovaries are recorded, inside of which there are a large number of follicles with immature eggs.
Hormonal imbalances are confirmed by tests. The parameters of estradiol, estrone, estriol, pregnanediol and progesterone are studied.
Normal levels of ovarian hormones (estrogens) in the urine
| Hormone concentration, mcg/day | ||||
| Hormone | First phase of the menstrual cycle (before ovulation) | Ovulation period (13-15 days) | After ovulation | Menopause |
| Estradiol | 1 – 23 | 4 – 45 | 1,4 – 12,2 | Up to 4 |
| Estrone | 2 – 39 | 11 – 46 | 3,3 – 44,6 | 1 – 7 |
| Estriol | 3 – 48 | 20 – 130 | 6,1 – 32,4 | 0 – 30 |
Concentration of pregnanediol in urine, mg/day
| First phase of the menstrual cycle (before ovulation) | Ovulation period (13-15 days) | Pregnancy | ||
| Up to 13 weeks | 13-28 weeks | After 28 weeks | ||
| 0 – 2,6 | 2,6 – 10,6 | 10 – 35 | 35 – 70 | 70 – 100 |
Progesterone concentration in blood, nmol/l
| First phase of the menstrual cycle (before ovulation) | Ovulation period (13-15 days) | After ovulation | Menopause | Pregnancy | |
| 1st trimester | 2nd trimester | 3rd trimester | |||
| 0,181 – 2,84 | 0,385 – 38,1 | 5,82 – 75,9 | 35,0 – 141,0 | 80,8 – 264,0 | 187,0 – 681,0 |
Estradiol concentration in blood, pg/ml
| First phase of the menstrual cycle (before ovulation) | Ovulation period (13-15 days) | After ovulation | Menopause | Pregnancy | |
| 1st trimester | 2nd trimester | 3rd trimester | |||
| 12,4 – 233,0 | 41,0 – 398,0 | 22,3 – 341 | 155 – 3245 | 1560 – 21280 | 8520 – 30000 |
Analysis of these indicators allows us to determine the usefulness of ovarian function. Based on the results obtained, one can judge the degree of their underdevelopment - the stronger the deviations from the norm, the more pronounced the pathology.
Treatment of ovarian hypoplasia
Treatment of ovarian hypoplasia
Since the disease is caused by a violation of organ development, it cannot be completely cured. However, modern medicine, with the help of hormone replacement therapy, helps to normalize the menstrual cycle, get pregnant, bear and give birth to children.
Such a woman will need more careful preparation for pregnancy. Before conception, a full examination and folliculometry is carried out. In the absence of ovulation, it is stimulated with the help of special drugs.
If the ovaries are underdeveloped, accompanied by improper formation of the fallopian tubes, pregnancy can occur after IVF, during which a mature egg is taken from the ovary, fertilized and implanted in the uterus. In severe cases, it is necessary to resort to IVF with donor embryos or surrogacy.
Unilateral ovarian hypoplasia, as a rule, is not an obstacle to pregnancy and childbirth.
Such a woman needs to carefully monitor her health, since with pathologies affecting the only ovary, the woman may completely lose reproductive function.
Contraceptives are selected for her - termination of pregnancy with this feature can lead to persistent secondary infertility.
At the University Clinic, you can undergo diagnostics of various forms of ovarian hypoplasia and, together with your doctor, select adequate hormonal therapy. A gynecologist-endocrinologist will help women with this feature properly prepare for pregnancy.
link:
Source: https://unclinic.ru/gipoplazija-jaichnikov-vzroslaja-problema-rodom-iz-detstva/
How is ovarian hypoplasia diagnosed?
In order to identify ovarian hypoplasia, if there is suspicion, the patient must undergo the following series of procedures:
- An examination by a gynecologist, during which the doctor will identify defects in the external genitalia.
- Ultrasound examination and hysterosalpingoscopy, which will reveal uterine underdevelopment.
- Examination of uterine mucus.
- Hormonal screening designed to determine the exact level of estrogen in the blood.
- Tomography of the brain.
- Pituitary examination (radiography of the so-called sella turcica).
If the case is more severe, the doctor may prescribe an ovarian biopsy or diagnostic laparoscopy.