What is myometrium and what should it be like?
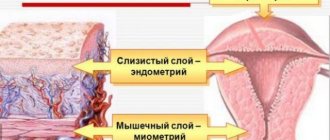
The myometrium is the middle muscular layer of the uterine wall. It is formed by bundles of smooth muscle cells (myocytes) with layers of connective tissue. In the myometrium, three vaguely demarcated layers are distinguished, differing mainly in the location of the main number of cells:
- Submucosal layer underlying the basal part of the endometrium. Formed by oblique longitudinal thin muscle bundles.
- Vascular (middle) layer with a circular or circular arrangement of myocytes. It is the thickest and most powerful. This layer is richly vascularized and contains a significant number of medium and small vessels.
- The supravascular or subserous layer borders the outer serous membrane of the uterus and is formed by longitudinal and partially circular muscle bundles.
Normally, in a woman of reproductive age outside of pregnancy, the myometrium on ultrasound has a fairly homogeneous echostructure without obvious differentiation of layers, visible connective tissue layers and clearly visualized vessels. Its thickness is slightly different in the area of the fundus, middle part and isthmus, which is not a pathology and ensures the functional usefulness of uterine contractions during labor.
The echogenicity of the myometrium of the non-pregnant uterus approaches the density of the main parenchymal organs: kidneys (their cortex), liver, pancreas. During pregnancy, the muscle layer thickens significantly due to hypertrophy of myocytes and their hyperplasia (increase in the number of cells). In postmenopause, the opposite condition is observed with atrophy of all layers of the uterus, including the myometrium.
Myometrial heterogeneity
Myometrial heterogeneity is an exclusively echographic term. That is, such a condition can be detected in a woman during her lifetime and without removing the organ (uterus) only with the help of an ultrasound scan performed using a vaginal or transabdominal sensor. Moreover, it is not always possible to determine unambiguous clinical signs corresponding to a certain type of a given pathology.
The appearance in the myometrium of hyperechoic and hypoechoic inclusions of various sizes, origins and shapes, uneven thickenings, changes in the ratio of stromal (connective tissue) cells and myocytes - all this is a deviation from the norm. In such cases, the ultrasound report indicates that the structure of the myometrium is heterogeneous. And this is the basis for obtaining a consultation with a gynecologist, since only a doctor can evaluate the results of the study and determine the need for treatment.
The fact is that sometimes the heterogeneity of the muscular layer of the uterus detected on ultrasound is not considered as a condition in need of correction. This is possible in the following cases:
- Age-related changes in the female reproductive system in the postmenopausal period, caused by a natural progressive decrease in the level of sex hormones and activity. At the same time, the entire myometrium is diffusely heterogeneous due to uneven fibrosis - atrophy with the replacement of myocytes by connective tissue.
- Consequences of damage to the uterine wall. The reason for this may be difficult childbirth, surgical interventions (including delivery by cesarean section), medical abortions with curettage, or insufficiently careful invasive examinations of the endometrium.
- Degenerative changes in the myometrium against the background of long-term, uncorrectable endocrine disorders.
But most often, heterogeneity detected on ultrasound is a pathological sign and becomes the basis for diagnosing a number of diseases.
Diffuse changes in the myometrium: signs, causes, treatment
What are diffuse changes in the myometrium and what does it mean? First of all, the concept of “diffuse changes” in medicine does not mean a disease as such, but only a diagnostic sign that is detected by ultrasound.
The myometrium is the middle layer of the uterus, consisting of muscles permeated with blood vessels that allow the organ to contract. It is vital for the rejection of the surface layer of the endometrium, which is removed from the uterus along with menstrual blood, and, of course, for pushing out the baby during childbirth.
Features of the structure of the layers of the uterus
At any age, the normal structure of the myometrial layer should be homogeneous, without pathological inclusions.
At the beginning of the female cycle, the mucous layer (endometrium) is thin, usually 1 - 2 mm, before monthly bleeding it can reach a thickness of 12 - 15 mm.
After 45–50 years, both layers gradually become thinner.
Since mucous and muscle tissue are interconnected, abnormal processes and pathological changes in tissue structure usually affect both layers.
In a normal pregnancy, if the patient did not show signs of adenomyosis before conception, the muscle layer is homogeneous and does not have echo signs of diffuse changes.
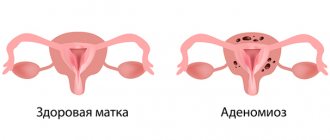
Thus, diffuse changes in the myometrium are heterogeneities in the tissue structure evenly distributed throughout the muscle thickness, which are visible during ultrasound examination and indicate the development of adenomyosis.
Adenomyosis and endometriosis - what's the difference?
If on an ultrasound the doctor discovers that the myometrial tissue is diffusely heterogeneous due to focal changes, this means that the likelihood of endometriosis or adenomyosis is high.
What is the difference between these two conditions?
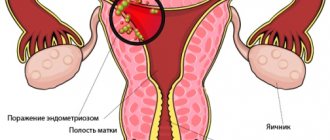
With endometriosis, elements of the endometrium (the mucous membrane of the uterine body) at different stages are able to grow into all layers of the organ, up to the peritoneal layer, and even spread beyond the uterus, penetrating the ovaries and peritoneum (ectopic endometriosis).
With adenomyosis, mucosal cells penetrate only into the muscle tissue of the myometrium, without going beyond its boundaries. That is, adenomyosis is considered the first phase of endometriosis.
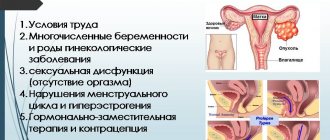
Causes
Doctors try to identify the exact cause of the development of abnormal diffuse changes in the myometrium through various types of research - theoretical and clinical.
But at the moment there is certain confirmation from specialists that the causes of significant or moderate diffuse changes in the myometrium, and therefore endometriosis, can be:
- medical interventions affecting uterine tissue, including abortion, childbirth, caesarean section;
- diagnostic curettage, removal of cysts, uterine polyps, fibroids;
- endocrine pathologies - thyroid diseases, diabetes mellitus, autoimmune processes, obesity;
- disorders of the function of the gonads, leading to hormonal disorders that provoke pathological growth of the endometrium;
- hereditary predisposition;
- severe and prolonged stress causing neurogenic disorders;
- sexual infections of any nature;
- inflammatory diseases of the reproductive organs;
- prolonged and frequent sun exposure.
Sonographic changes
Echo signs of diffuse changes recorded during the ultrasound procedure are the main indicator of myometrial heterogeneity.
Echogenicity - what is it? First of all, this is an important parameter in ultrasound diagnostics.
Why does this happen?
The main causes of heterogeneous myometrium:
- Endometriosis and its internal genital type, also called uterine adenomyosis.
- Myometritis. In the vast majority of cases, it is a consequence of complicated endometritis, so in fact we are talking about endomyometritis.
- Uterine fibroids. It can lead to local nodular changes or almost total thickening of the myometrium (in the diffuse form of the disease).
Each of these diseases not only has special symptoms, but also leads to characteristic changes in the myometrium. They can be differentiated using ultrasound; in the protocol of the study, the specialist describes the echographic picture of the detected pathology and indicates its type.
Adenomyosis is the most common cause of myometrial changes
Endometriosis is the pathological growth of endometrial cells outside the lining of the uterus. When the myometrium is predominantly affected, we speak of adenomyosis, which can be of diffuse and nodular type, and of varying degrees of severity.
This disease is classified as benign hyperplasia of a hormonal-dependent nature. So it is typical for women of reproductive age, and in the postmenopausal period and against the background of adequately selected hormonal therapy, the activity of the process subsides.
With adenomyosis, growths of endometrioid tissue appear in the myometrium. They can be of two types:
- In the form of blind branched deepening pockets communicating with the endometrial layer of the uterus. In such cases, the ultrasound report usually indicates that the echostructure of the myometrium is heterogeneous and cellular. In severe degrees of the disease, germination of the entire thickness of the myometrium is noted, which is accompanied by the formation of fistula-like formations between the uterine cavity and other structures of the small pelvis.
- In the form of nodes - closed round lesions with an uneven central cavity filled with blood or a chocolate-colored liquid mass. They are usually multiple, of varying sizes, with an uneven distribution in the uterine wall. With this variant of the disease, the conclusion of an echographic examination usually notes that the myometrium is heterogeneous with signs of adenomyosis.
Any endometriotic formations undergo repeated changes in accordance with a woman’s ovarian-menstrual cycle and lead to an inflammatory process. Under the influence of sex hormones, cells of the abnormally located endometrium grow and are rejected in the same way as in the uterine mucosa. This leads to the appearance of clinical symptoms of the disease.
Adenomyosis is characterized by cyclic uterine bleeding, which is more profuse and painful compared to normal menstruation. And the emptying of stagnant cavities and endometrioid pockets leads to the appearance of chocolate-colored discharge from the genital tract. They are actually menstrual blood that has accumulated and undergone incomplete decomposition.
Myometrial changes during pregnancy
Heterogeneous myometrium during pregnancy is quite rarely the primary diagnostic finding. In most cases, the disease is detected at the planning stage or in the previous life period. And ultrasound during pregnancy is used not only for dynamic assessment of fetal development, but also to monitor the condition of the uterine wall.
This is necessary not only to determine the tactics of current treatment, but also to draw up a prognostic assessment. After all, such tactics make it possible to timely identify signs of incompetence of the uterine wall in areas of damage to the myometrium and the threat of its rupture during childbirth, and resolve the issue of the feasibility and admissibility of natural delivery.
It should be remembered that only a doctor can interpret ultrasound data. Diagnosed changes in the myometrium in themselves are not grounds for immediate initiation of therapy. Therapeutic tactics are determined individually, taking into account the dynamics of the clinical and echographic picture of the disease, etiology and severity of the identified pathology.
With previous adenomyosis, a pregnant woman is considered to be at risk for miscarriage and the development of chronic placental insufficiency. Myoma increases the likelihood of an abnormal course of the labor period and is a risk factor for insufficient uterine contraction in the postpartum period with the development of pathological bleeding. And fibrosis and scar changes in the myometrium can cause ruptures of the birth canal during the pushing period of labor or insufficient productivity of contractions.
After undergoing a medical examination by a gynecologist, a woman begins to become more interested in the structure of her body. For example, the myometrium: what is it, what function does it perform, what is it needed for?
Myometrium and its structure
The middle muscular layer of the uterine lining is called the myometrium. On the inside it is covered with endometrium. A calm, relaxed state of the myometrium is considered normal. Under the influence of various factors, its muscles tense (contract), and a condition of the uterus occurs, which is called hypertonicity.
Uterine hypertonicity is not a pathological process in all cases. Sometimes this is necessary (during childbirth or during menstruation). In other cases, hypertonicity indicates an unfavorable state of women's health. As a result, uterine bleeding may begin (including during menopause), a miscarriage may occur during pregnancy, or premature labor may begin.
The state of the myometrium is significantly influenced by hormonal balance, especially the amount of estrogen and oxytocin.
The myometrium has a complex structure. It consists of 3 layers, each of which is smooth muscle fibers:
- the longitudinal layer, which includes circular and longitudinal muscle fibers, is the adjacent perimetric layer;
- circular layer (or vascular), consisting of rings of pipes, it includes many vessels;
- the submucosal layer, consisting of longitudinal fibers, is the most fragile of all layers.
The uterus has its ability to contract due to the fact that the myometrium consists of so many different layers. This quality is necessary for pushing blood out during menstruation.
All women are well aware of such a disease of the female genital area as fibroids. This name comes from the word “myometrium”. Myoma is a tumor that is retained by the myometrial layer. In some cases, this tumor reaches a significant size up to 20 weeks of pregnancy (this is how this tumor is measured). Patients are often deceived into thinking that pregnancy has occurred.
When the doctor says that the uterus is hypertonic, this means that the myometrium has thickened. In this case, its stimulation is required so that the hypertonicity disappears.
The healthy state of the uterus is associated with a homogeneous myometrium. During normal pregnancy it is the same. During the postmenopausal period, both the myometrium and endometrium gradually atrophy. These same two layers also change during infectious inflammation, since they are interconnected. This is well observed with ultrasound.
What is homogeneous myometrium
The myometrium of the uterus is the middle membrane of the reproductive organ, bordering the endometrium and perimeter. The structure of the myometrium may change depending on the number of births, surgical interventions, and pathological formations. Its condition can be assessed and a detailed description can be given during ultrasound diagnostics. During the examination, it is important to pay attention to the condition of other components: the endometrium, ovaries, and the size of the uterus. The obtained indicators are correlated with the woman’s age and medical history and a conclusion is made.
Structure
In a normal state, during an ultrasound scan, the myometrium is homogeneous, without diffuse changes and any neoplasms. The muscle tissue of the uterus includes several powerful layers:
- the subserous area consists of circular and longitudinal muscle fibers - it is in contact with the connective tissue of the lining of the uterus;
- the middle section includes many vessels, circular fibers - this zone of the muscle layer is the most pronounced;
- the submucosal area is considered the most fragile and includes longitudinal fibers - it is closely connected with the endometrium, lining the inner surface of the muscular organ.
In a healthy woman, the myometrium is always homogeneous and has a constant thickness - 1.5-2.5 cm - regardless of the influence of internal factors.
The thickness changes only after childbirth and during menopause. By conducting regular ultrasound monitoring, one can note the intensity of changes during the prenatal and postpartum period. In girls and young nulliparous healthy women, the myometrium is homogeneous and does not have any inclusions. A woman who has a history of two or more births has diffuse changes in the myometrium and this is considered normal. During menopause, the muscle layer may become thinner and contain hyperechoic inclusions. The peculiarity of the structure of the area under consideration is that near the isthmus, fundus of the uterus and the middle part it is slightly larger than in other zones. This is not a pathological condition if there are no inclusions of heterogeneous foci. Homogeneous myometrium is an echogenic structure that does not have a clear distinction between layers and visible layers connecting zonal areas. The most favorable time for ultrasound diagnostics is from 5 to 10 days of the menstrual cycle. During this period, it is possible to visualize various pathological formations that are located in the endometrium involving the myometrium. But some pathologies require research at the end of the cycle. The muscle layer does not change throughout the monthly cycle, however, doctors carry out comprehensive diagnostics and a number of formations can affect both layers, so the gynecologist prescribes the day of the examination.
Changes in the myometrium in some diseases
You can find out which changes are completely normal and which cause pathology by looking at the size of the layers. The structure of the myometrium is normally homogeneous (that is, homogeneous). At the beginning of the menstrual cycle, the layer is no more than 2 millimeters in size, in the second half it reaches 14 millimeters.
With endometriosis, the myometrium changes, which is not always noticeable on ultrasound. This disease is quite common among women of any age. It is characterized by pathology in the membranes of the uterine wall. Cells of the endometrial layer grow into the body of the uterus, and passages are formed, which look like cells during ultrasound examination.
An ultrasound will show that the myometrium with endometriosis appears normal. But this is not evidence that there are no changes. Those inclusions that are characteristic of this disease are too small and therefore not visible during examination. The structure of the myometrium becomes heterogeneous.
The structure of the myometrium in a healthy woman and in diseases
The myometrium is the muscular layer of the uterus, which consists of smooth muscle cells - myocytes. The myometrium is lined with a mucous membrane - the endometrium, this is the inner layer of the uterus. The structure of the uterine myometrium is complex; it consists of three layers of smooth muscle fibers: subserosal, middle and submucosal. This structure allows the uterus to contract well during childbirth and expel fluid during menstruation. In the subserous layer, the muscle fibers are located longitudinally and are closely fused with the outer serous cover of the uterus - the perimeter, which consists of longitudinal and circular fibers.
The middle layer of the myometrium is formed by muscle fibers running in a circle. This is the largest and strongest layer of the uterus. There are a lot of vessels located in the circular layer, and in inflammatory diseases, hypervascularization of the myometrium is observed mainly in the middle layer. The submucosal layer is the thinnest, it consists of longitudinal fibers and is closely connected to the mucous membrane.
The mucous membrane undergoes physiological changes during the menstrual cycle, and is rejected with the onset of menstruation. During a pregnancy that proceeds without abnormalities, the myometrium should be homogeneous, without pathological foci. After menopause, gradual atrophy of the myometrium and endometrium is observed. Pathological processes caused by infection usually affect both layers, because they are very closely related to each other, and pathological changes, accordingly, are observed in both the myometrium and the endometrium. This is clearly visible during ultrasound examination. To know which changes are a sign of a disease and which are absolutely harmless, you need to have an idea of the normal size of the layers of the uterus. For the myometrial layer, the norm is homogeneity, without pathological foci. At the beginning of the cycle, the normal endometrium should be thin and only 1-2 mm; in the second phase of the cycle it can grow up to 14 mm.
Changes in the uterus with adenomyosis
Adenomyosis or endometriosis is a common disease that occurs in women of all ages and is characterized by damage to the muscular and serous lining of the uterine walls. Endometrial cells grow into the thickness of the uterus and form peculiar passages, which is determined by ultrasound as a cellular structure.
There are diffuse and local forms of the disease. In the diffuse form, the uterus acquires a spherical shape and has the same size as at 5-9 weeks of pregnancy. Moreover, during and before menstruation, the uterus enlarges. The structure of the myometrium may look normal on ultrasound, but this does not mean that there are no changes, just small inclusions characteristic of endometriosis are not visible. In the presence of linear or point inclusions, an inhomogeneous heterogeneous structure is observed.
An important parameter in the ultrasound diagnosis of uterine diseases is echogenicity. Normally it is low. Its increase indicates the presence of pathological foci. With endometriosis, hyperechoic inclusions are determined in the myometrium, which range in size from 1 to 5 mm and are located diffusely in the thickness of the uterus.
The border between the endometrium and myometrium is tortuous, and the thickness of the myometrium of the posterior wall of the uterus is greater than the anterior one. A decrease in echogenicity occurs before menstruation due to vasodilation or tissue swelling. If an inflammatory process occurs, the average echogenicity is determined during diagnosis. Main symptoms of the disease:
- Long and heavy menstruation
- Bloody discharge of varying intensity, not associated with menstruation
- Painful pulling and aching sensations in the lower abdomen
- Menstrual irregularities.
The causes of adenomyosis can be frequent stress, complicated abortions and childbirth, constant sun exposure (occurs in women who visit solariums). Adenomyosis is dangerous for the development of infertility, especially for severe cases of the disease. The fact is that with endometriosis, adhesions often form, which interferes with the implantation of a fertilized egg. Many women who have suffered from this disease are forced to resort to in vitro fertilization (IVF).
If an ultrasound reveals heterogeneous variegated myometrium, this means that the woman suffered an inflammatory disease of the uterus and developed endometriosis. There are two types of treatment for this disease: hormone therapy and surgery. Hormonal drugs are toxic and somewhat dangerous, and they are not highly effective for endometriosis. The operation is justified only in the event of external endometriosis - extragenital. Endometriotic tissue is cauterized using special devices. Herbal preparations are used to restore hormonal levels and improve the body's immune defense, as well as prevent inflammatory diseases.
More information about uterine fibroids is described in this video:
Fibroids are a benign tumor that is found in 20% of women over the age of 35. This disease is characterized by an enlarged uterus. Most often, the nodes are located in the body of the uterus. The main localizations of myomatous nodes: submucosal (submucosal), interstitial, subserous. There may also be intermediate types: interstitiosubmucous and interstitiosubserosal. The echostructure of the myometrium changes; the myomatous node itself is detected on ultrasound as an oval or round formation with clear boundaries. If there are many vessels in the node and muscle tissue predominates, it will be hypoechoic.
Also, with fibroids, calcification of the myometrium, or rather myomatous nodes, can occur. A more accurate diagnosis of uterine fibroids is possible using intrauterine ultrasound; now this method has not yet become widespread. Diagnosis is carried out with special sensors on the expanded uterine cavity. This method provides objective information about the size of the intramural part of the submucous node even before surgery. At the moment, three-dimensional echography is used in gynecology, which is more informative than conventional ultrasound.
Endometrial hyperplasia is a benign growth of the uterine lining. In this case, the endometrium has a thickness of more than 16 mm, and it itself is homogeneous or heterogeneous.
Myometritis is an inflammation of the myometrium, often developing as a result of an infectious lesion of the uterine mucosa. Clinical manifestations are very similar to those of endometriosis, so ultrasound is used for accurate diagnosis. In the uterus, signs of inflammation are detected, an increase in the thickness of the endometrium and the size of the uterus; fluid can be detected in the cavity.
If an ultrasound shows adhesions in the uterine cavity, a diagnosis of chronic myometritis is made. Myometritis and endomyometritis are often asymptomatic, so early diagnosis can be difficult. Very often, this disease is detected accidentally during a general examination, pregnancy or infertility. Untreated endometritis is dangerous for the development of complications and the formation of adhesions. If you have been diagnosed with this, do not refuse treatment. According to statistics, it is known that this disease is one of the main causes of infertility.
Heterogeneous myometrium
Changes developing in the myometrium cause diseases not only of the uterus. Other genitals may also be affected. For example, endometriosis has a genital form. There is another one - extragenital, in which damage to the urinary system and intestines occurs.
Until a certain stage, myometrial heterogeneity does not manifest symptoms. That’s why you can often hear advice that you should visit a gynecologist annually. This is the only way to identify various pathologies of the female genital area.
Gradually, symptoms begin to manifest themselves as severe pain in the lumbar region, during menstruation, during sexual intercourse, and when urinating. Bleeding often occurs on days other than your period.
There are several reasons for myometrial heterogeneity. One of the main ones is heredity. This condition can be provoked by childbirth that traumatizes the uterus (for example, caesarean section). Abortion, any intervention that affects the inner uterine layer (including during a diagnostic study), stress, and abnormal functioning of the thyroid gland also lead to heterogeneity of the myometrium.
The disease is diagnosed in various ways. At a medical appointment, the doctor interviews the patient, identifies symptoms that are troubling her, and examines the uterus using special instruments.
Blood biochemistry is carried out, which will show the amount of sex hormones.
Ultrasound is also used, which will show the myometric echostructure.
Individual treatment regimens are selected for each patient. Many factors are taken into account: previous illnesses, the age of the patient, the course of past pregnancies, whether organs are affected or not.
When treating, it is imperative to take into account that the consequences are the least dangerous.
Treatment is carried out in three ways:
- medicinal;
- surgical (doctors try to preserve all organs if possible);
- uterus removal.
For prevention purposes, you should pay attention to your health from an early age. If a girl complains to her mother about pain during menstruation, then she should be shown to a pediatric gynecologist. In the future, you need to develop the habit of visiting your doctor regularly. And if any operations affecting the genital area have been performed, then consultations with a doctor should be carried out at least 2 times a year or as prescribed by the doctor. You should not delay the treatment of inflammatory processes in the genital organs.
If a woman has chosen intrauterine devices as contraceptives, then at the slightest suspicion of pathology, consultation with a gynecologist is necessary.
Every girl in our time may face various problems that relate to women's health. One of them is heterogeneous myometrium. Before you are afraid of incomprehensible terms, you should still figure out what it means, how to treat it, and why such a diagnosis is dangerous.
Indications for prescribing ultrasound of the cervix
The content of the article
As a rule, an ultrasound of this organ of the woman’s reproductive system is performed in conjunction with an examination of the uterus and appendages. Ultrasound of the cervix allows you to assess the size, structure, blood supply of organ tissue and identify many pathologies at an early stage of development.
It is necessary to prepare for the procedure in advance, but it has no age restrictions, no contraindications, does not depend on the menstrual cycle and can be performed even during pregnancy.
Ultrasound of the cervix is prescribed for the following indications:
- heavy vaginal discharge (leucorrhoea, with blood clots), blood discharge outside of menstruation, spotting, pink discharge, bloody or pink discharge during and after sexual intercourse;
- irregular menstrual cycle, heavy menstrual bleeding (changing hygiene products more than once an hour), absence of menstruation;
- pain in the lower abdomen, especially acute, pain during sexual intercourse;
- female infertility;
- swelling of the legs;
- problems with urination;
- confirmation of gynecological diagnosis;
- suspicion of oncology (at the same time you need to take tests for tumor markers);
- routine examination during pregnancy.
What is uterine myometrium, its structure and norms
The myometrium is one of the muscular layers of the uterus, which is located in the middle of the uterine cavity. The inside side is covered with endometrium. The main role of the myometrium is rhythmic contractions, due to which the baby is pushed out through the birth canal. The normal state for the myometrium is rest, but under the influence of some moments the muscle layer can begin to contract and become hypertonic.
The myometrium consists of three layers:
- Longitudinal layer consisting of longitudinal and circular muscle fibers. This layer is strongly connected to the serous covering of the uterus;
- The circular layer, which includes the vessels and tubular rings, is the strongest of all the layers. The highest density of this layer falls on the cervix. Due to the fact that this layer contains many small vessels, it is also sometimes called vascular;
- Submucosal layer consisting only of longitudinal fibers. The structure of this layer is very fragile and thin.
The norm for a healthy myometrium is homogeneity. Due to a number of reasons, its structure may be damaged, and then the myometrium no longer has such a uniform structure. The most basic diagnostic method, which allows you to immediately identify various pathologies in the uterine area, is ultrasound. Hysteroscopy is also a good way to get a complete picture of the appearance of the uterine myometrium.
What is myometrial heterogeneity
Diffuse heterogeneous myometrium is a benign formation that occurs due to abnormal functioning of the endometrium. The main diagnostic method for this diagnosis is ultrasound. The main determining parameter on ultrasound is the echostructure of the myometrium. In normal condition, it has low indicators. Moreover, in some cases it is very difficult to diagnose the signs that correspond to this diagnosis.
The appearance in the muscle layer of hypoechoic and hyperechoic features of different sizes, shapes and origins, uneven compactions, changes in the proportion of stromal cells and myocytes - all this is a deviation from the normal structure of the myometrium. This means that the ultrasound report will indicate the heterogeneous structure of the myometrium. This means that you need to consult a gynecologist. Because only a specialist can correctly assess the examination results and prescribe the correct treatment.
Signs of cervical pathologies on ultrasound
| Pathology | Sign on ultrasound |
| Cervical erosion | superficial violation of the cervical epithelium, not extending deep into the tissue |
| Cervical cancer | formation in the form of “plus-tissue” with medium echogenicity, having an unclear silhouette and structure |
| polyps | formation with clear boundaries and uniform density that does not extend deep into the tissue (“plus tissue”) |
| Cystic disease | a clear formation of a round shape with a homogeneous structure inside in the form of a liquid |
| Carcinomas and adenocarcinomas | formation with unclear boundaries, deeply penetrating into the thickness of the cervix |
| Cervical pregnancy | endometrium with high echogenicity; the cervical canal is dilated and contains the fertilized egg; Placental tissue was found in the cervical canal |
| Cervical endometriosis | round hypoechoic cysts of the cervix with heterogeneous hyperechoic contents; the wall is thickened |
Why does it occur
A number of main reasons for the heterogeneous muscle layer:
- Endometriosis and its genital internal type, also called adenomyosis of the uterus;
- Myometritis is a consequence of severe endometritis, so we are practically talking about endometritis.
- Uterine fibroids. May lead to total thickening of the muscle layer or local nodular changes.
All these diseases not only have unique symptoms, but also lead to various changes in the myometrium. They can only be distinguished using ultrasound; in the conclusion, the specialist must write down the reasons for the heterogeneous structure of the myometrium.
Adenomyosis
Abnormal growth of endometrial cells beyond the lining of the uterus is called endometriosis. Adenomyosis of the uterus is a multifaceted lesion of the myometrium, which can be nodular or diffuse, and can also manifest itself differently as it progresses.
This diagnosis refers to benign hyperplasia of hormone-dependent organs. It is typical for women of childbearing age, and in the postmenopausal stage and if hormonal therapy is chosen correctly, a decrease in the development of the process is visible.
In the myometrium with adenomyosis, growths of endometriotic tissue begin to appear. They come in only 2 types:
- In the form of deepening blind branched pockets connecting to the endometrial lining of the uterus. In this case, the ultrasound content indicates that the echostructure of muscle tissue is cellular and heterogeneous. With a complex degree of the disease, thickening of the entire myometrium is noted, which usually accompanies the formation of fistula-like bases between the uterine cavity and other forms of the small pelvis;
- In the form of rounded nodules with an uneven cavity, which are filled with a bloody or brownish substance. As a rule, a large number of neoplasms of this type are formed in the uterine cavity, which differ from each other in diameter and location. After an echographic diagnosis, in this case, the doctor’s conclusion states that the heterogeneous myometrium with adenomyotic signs is progressing.
Adnexitis (inflammation) is associated with the formation of endometrioid cysts and menstrual irregularities. In this regard, the cellular tissue of the incorrectly placed endometrium due to the action of the gonads grows and is rejected. This is the main provocateur of unpleasant symptoms.
Compared to the course of normal menstruation, with adenomyosis stronger and more frequent discharge occurs with pronounced painful sensations. The appearance of brown discharge indicates that this is a consequence of the passage of remnants of undecomposed menstrual blood during the emptying of stagnant channels and endometrioid pockets.
Adenomyosis can cause chronic iron deficiency anemia and persistent pelvic pain. This may result in the woman being unable to have children in the future. Therefore, even if there are no obvious signs of endometriosis, before planning a pregnancy you should still first be examined and have an ultrasound scan.
Myoma
Myoma is a benign formation in the uterine cavity. This disease is common mainly in females over the age of 40 years. This happens due to the fact that a woman experiences changes in her reproductive system due to age-related changes.
Typically, a fibroid resembles a nodule in its likeness, which was formed as a result of thickening and hypertrophy of the muscular layers of the uterus. Basically, such a neoplasm is located inside the myometrium or protrudes towards the serous or mucous layers. Myomatous formations can be located in different locations and be of different sizes. Diffuse myamatosis is one of the rare forms of this disease.
During pregnancy
Usually, it is quite difficult to detect heterogeneous meometrium during pregnancy, therefore, before planning conception, it is necessary to first undergo an examination. During the period of bearing a baby, an ultrasound examination must be done in order to monitor the normal development of the embryo, as well as to monitor all kinds of processes occurring in the uterine cavities.
At the same time, the specialist must determine the tactics of subsequent treatment, as well as make a prognostic assessment. After all, this will allow a timely assessment of the state of the heterogeneous myometrium and its further development (whether it will rupture during childbirth), which directly depends on whether the woman will give birth naturally.
How to treat
When myometrial heterogeneity is treated, the treating doctor must select an individual course based on the patient’s characteristics: general health, degree of uterine damage, age, as well as past previous diseases.
There are three main ways to treat this disease:
- Drug treatment;
- Surgical intervention during which the uterus is preserved;
- Removal of the uterus.
Drug treatment involves taking a certain type of drug that reduces the growth of endometrial cell mass. In order to eliminate pain, a specialist can prescribe tablets with antispasmodic and analgesic spectrums of action, and to treat the disease itself, hormonal medications are prescribed.
When the drug treatment method does not give the desired effect, then it is worth resorting to a method such as hysteroscopy, which involves curettage of the uterus. Sometimes after this, relapses occur, and the meometrium again becomes heterogeneous.
Cauterization of the uterine walls is a subsequent method of aligning the myometrium. The way the doctor straightens the myometrium is called coagulation. The chances of a relapse are extremely low; moreover, this process is completely reliable and harmless.
In the event that this disease is advanced and the heterogeneous myometrium provokes a host of other diseases, complete removal of the uterus is possible. After such an operation, the patient will have a chance to continue her normal life without problems with women’s health.
It is worth remembering that the absence of abortions, regular consultations with a gynecologist, as well as timely prevention of infection - all this is the prevention of this disease.
How to prepare for a cervical examination
The reliability and quality of the results directly depends on the quality of preparation for the study. Therefore, it is necessary to first clarify with the doctor exactly which ultrasound method he will use so that the preparatory measures are carried out correctly.
Transabdominal ultrasound
The patient must follow a special slag-free diet the day before the procedure, the main goal of which is to reduce gas formation in the intestines. Therefore, it is necessary to exclude legumes, carbonated drinks, yeast and dairy products, fresh vegetables and fruits, and sweets from consumption.
The study is carried out with a full bladder, so 1 hour before the test, the woman should drink 1 liter of liquid (non-dairy and non-carbonated) and not urinate.
Transvaginal ultrasound
THIS research method does not require preliminary preparation. The only thing you need to do is empty your bladder immediately before the procedure. Also, as an additional recommendation, take medications that reduce flatulence (smecta, espumizan, activated carbon, etc.) the day before the ultrasound.
Transrectal ultrasound
A woman, 7–9 hours before the procedure, needs to cleanse the rectum of feces using a cleansing enema with water (1–1.5 liters), microenemas, rectal glycerin suppository or laxative. All this can be bought at the pharmacy, explaining the purpose of use.
Through the skin of the perineum
There is no need to prepare for the procedure.
As for pregnant women, they do not need to prepare, since amniotic fluid plays the role of fluid.