Size of the uterus during menopause: changes, ultrasound norms and pathological conditions
The onset of hormonal changes in the female body leads to a number of anatomical and physiological changes in many systems and organs. To a greater extent, women's reproductive organs, namely the ovaries and uterus, undergo changes during menopause. Let's take a closer look at what changes the female uterine organ undergoes with the onset of menopause.
Reasons for reducing parameters
Age-related changes
In women over 50 years of age, ovarian function decreases. Therefore, atrophy of the genital organs is naturally observed. Size reduction occurs gradually and is the norm. An increase or maintenance of previous parameters in dynamics should cause caution.
Developmental disorder
A small uterus during reproductive age may be a consequence of underdevelopment of the organ. Depending on the stage when unfavorable factors acted, the organ may have structural abnormalities or differ only in uniformly reduced parameters:
- during embryogenesis, the process of fusion of the Müllerian ducts is disrupted, an organ with a septum, bicornuate or saddle-shaped is formed;
- from 2 to 8 years of age – the small size may remain.
Insufficient development, or infantilism of the genital organs, occurs when sexual development is delayed. But other symptoms are added to the morphometric deviations. A girl aged 12-13 years has no signs of puberty:
- no pubic and axillary hair growth;
- the chest remains in the Ma0 state;
- menstruation does not begin;
- There are no changes in the figure according to the female type.
Infantilism may be a consequence of congenital genetic abnormalities, in which the formation of reproductive organs is disrupted or the synthesis of sex hormones is disrupted.
Uterus during menopause
The main phases of menopause are premenopause and menopause, after going through which a woman begins a long period of postmenopause, which accompanies her throughout her entire subsequent life.
The premenopausal period is quite long: from 3 to 10 years. This period is characterized by changes in almost all organs and systems in the female body. They can appear in a more vivid form or, with timely treatment, in a smoothed form:
- psychological disorders;
- changes in thermoregulatory processes in the body;
- hormonal imbalance, accompanied by a deficient level of production of sex hormones;
- disturbances in the menstrual cycle, until its completion.
The menopausal period begins immediately after the last menstrual period and continues throughout the next year. It is believed that the end of menopause occurs after 12 months of absence of menstruation. During this period, involutional changes in the genital organs occur in the female body. Almost all reproductive organs begin to decrease in size, and even the uterus decreases in size during menopause. Not only the size of the genital organs decreases, but also the amount of cervical mucus, which subsequently has an important impact on the state of the microflora.
Moreover, during menopause, the overall level of resistance of the body to the effects of pathogenic factors decreases. Some organ systems begin to function less well, which leads to a decrease in the body's immune defense system.
Therefore, many women who have entered the threshold of menopausal changes are faced with various diseases, especially those related to the reproductive system.
Thus, in most cases, the occurrence of tumor-like processes in the area of the mammary glands and uterus is noted during menopause. Therefore, with the onset of menopause, it is necessary to regularly visit a gynecologist and undergo an annual examination. The main most dangerous pathological changes include:
- Inflammation of the uterus.
- Development of benign neoplasms in the uterine cavity.
- Development of a tumor-like neoplasm of oncological nature of the uterine organ.
- Breast cancer.
- Salpingitis or inflammation of the fallopian tubes.
- Endometritis.
- Vaginitis.
- Carcinoma.
- Fibroma, etc.
All these pathological changes in the reproductive system of a woman during menopause are very dangerous, and in the absence of timely treatment, many of them pose a serious threat to a woman’s life.
To prevent the development of serious pathologies, regular examinations in the gynecological office and timely ultrasound are necessary.
Why does the size increase?
Deviations in the size of the genital organs can be detected at any age. If they are within acceptable parameters, this should not be a cause for concern. In cases where the uterus is larger than normal, and an in-depth examination does not determine the pathology, dynamic observation is necessary. An ultrasound performed again after 6-12 months will allow you to compare the data with previous ones. Sometimes this time is enough for the first signs of pathology to appear.
An increase in parameters, confirmed by ultrasound, suggests pregnancy. In a period of up to 3 weeks, which corresponds to several days of delay, the fertilized egg is not visualized on ultrasound, but the indicators of length, width and thickness have already changed upward.
By palpation, an increase in size is determined by fibroids. Small nodes, a few millimeters in diameter, may not affect the parameters, but with significant pathology, the uterus can take on the shape of a ball or be completely distorted. A relatively uniform increase occurs with submucosal nodes, which grow into the organ cavity and expand it. With interstitial myoma, multiple nodes, the myometrium becomes tuberous. The size is determined by correlating the volume of the organ with the same period of pregnancy.
- Endometriosis and adenomyosis
The greater the degree of damage, the larger and rounder the uterus becomes. But its size never reaches the gigantic size that is possible with fibroids.
Changes are possible under the following conditions:
- endometritis, myometritis - due to inflammatory infiltration and tissue swelling;
- endometrial cancer – tissue swelling, tumor growth into the uterine wall.
With endometrial hyperplasia and polyps, the length and width of the uterine body most often fit into the age norm.
Ultrasonography
Ultrasound of the uterus during menopause is prescribed as a standard examination of the pelvic organs and diagnosis of pathologies with symptoms similar to menopausal syndrome.
The ultrasound research method provides a fairly high level of information content, is safe and does not cause hostility.
Despite the fact that menopause is a natural process, for most representatives of the fair half of humanity it can cause a number of unpleasant symptoms and discomfort, expressed as follows:
- disruption of the regularity of the menstrual cycle, up to its cessation;
- occurrence of dizziness and headaches;
- sleep disturbances with the development of insomnia;
- hot flashes;
- dryness in the vaginal area;
- frequent urge to urinate;
- pain during sexual intercourse.
Sometimes women cope with these manifestations on their own, but most often the help of hormone replacement therapy is needed. To assess the condition of the woman's reproductive system, an ultrasound examination is performed using a transvaginal sensor.
During menopause, the norm of changes in the uterus, revealed by ultrasound, is as follows:
- Increased echogenicity (or density) of the uterus.
- Its anteroposterior size decreases.
- Severe atrophy of the endometrial layer.
- Formation of adhesions and synechiae.
During the menopausal period, ultrasound examination may also reveal the presence of fluid in the uterine cavity. This is sometimes perceived by specialists as the development of a polyp or hyperplasia of the endometrial layer, although in fact this is not the case.
The formation of this fluid may normally be a consequence of the process of overgrowth of the cervical canal associated with the aging of the female body. But this condition requires a mandatory additional research method by hysteroscopy, which will help to more accurately assess the benign quality of the processes occurring.
A diagnostic examination using ultrasound examination of the pelvic organs is of great importance for a woman’s life, as it helps to identify serious pathologies in the initial stages of development.
Especially considering the fact that mature women are more susceptible to pathological changes in the uterus, such as its enlargement during the development of oncology during menopause. The process of enlargement of an oncological tumor is sluggish and does not cause specific symptoms. And the appearance of uterine bleeding and pain in the lower abdomen are observed in later stages of the disease.
Uterine fibroids
The uterus is a muscular organ and consists of three layers, the thickest of which is the myometrium (muscular layer).
Uterine fibroids are a benign, hormone-dependent tumor that is characterized by the development of nodes in the muscle layer. Uterine fibroids often occur in women aged 35-50 years, but recently there has been a trend towards younger age of the disease (in women 25 years and younger).
Based on the location of myomatous nodes, they are distinguished:
- subserous myoma (the node grows towards the abdominal cavity and is located under the subserous membrane);
- interstitial myoma (the node grows in the thickness of the myometrium);
- submucous or submucosal myoma (the node grows into the uterine cavity and is located under the mucous membrane);
- cervical fibroids (the node is located in the cervix).
Depending on the size of the myomatous nodes, which are compared with the duration of pregnancy, there are
- small fibroids (5-6 weeks),
- medium (7-11 weeks),
- large sizes (over 12 weeks).
According to the nature of the growth of uterine fibroids, false growth of the node/nodes, which increase with swelling and poor circulation in the formation (necrosis of the node) and true growth (proliferation of muscle cells), are distinguished.
Based on the number of nodes, fibroids with a single node and multiple fibroids are distinguished.
According to the severity of clinical manifestations, uterine fibroids can be asymptomatic or symptomatic.
Based on the histological structure and predominance of a particular tissue in myomatous nodes, they are distinguished:
- uterine fibroids (contains only muscle elements);
- uterine fibroids (contains connective tissue);
- uterine fibroids (equally connective and muscle tissue).
Predisposing factors for the occurrence of fibroids include hormonal imbalance, in particular excess estrogen in the body.
Also, provoking factors of the disease include mechanical trauma to the uterus and genetic predisposition:
- heredity (the presence of uterine fibroids in relatives of the first and second generations);
- menstrual irregularities, starting from the very first cycle (menarche), including those combined with sexual infantilism;
- disorders of menstrual function that cannot be cured, especially with metabolic disorders (diabetes mellitus, obesity);
- chronic gynecological and extragenital (not related to the reproductive system) diseases;
- abortions and uterine curettage;
- physical inactivity (low mobility);
- irregular sex life (rare or sexual intercourse that does not end in orgasm);
- stress, heavy physical labor;
- long-term insolation;
- no history of childbirth or breastfeeding.
Often, uterine fibroids are an accidental discovery during a routine examination by a gynecologist. Many women with uterine fibroids do not complain or do not attach importance to the signs of the disease.
The main symptom is menstrual irregularity. As a rule, menstruation becomes long and heavy (especially with submucous fibroids), and intermenstrual bleeding appears. Constant blood loss leads to anemia in the patient (weakness, malaise, fatigue, pale skin, etc.).
In addition, patients may be bothered by pain in the lower abdomen of a pulling or aching nature. The pain can be constant or appear only during menstruation. With necrosis of the myomatous node or birth (submucous myoma), the pain becomes sharp and cramping.
With large sizes of uterine fibroids, compression syndrome of neighboring organs will occur. In this case, frequent urination or chronic constipation is often observed.
Pathological changes in the uterine organ
During hormonal changes in the body, especially in premenopause, exacerbation of existing chronic gynecological pathologies may occur, as well as the formation of new ailments that can cause painful symptoms and uterine hemorrhages.
Let's consider the most dangerous pathological changes in the uterus during menopause.
Development of fibroids
This neoplasm itself has a benign course. Typically, fibroids appear during the fertile period, and with the onset of menopause it becomes more acute and begins to increase in size.
Fibroids can form in the form of one or several nodes localized in any part of the uterine cavity. Growing fibroids increase the standard size of the uterus several times, which leads to compression of nearby organs and the appearance of pain symptoms. Enormous growth of this neoplasm can lead to an enlarged abdomen. Moreover, fibroids also cause the following symptoms:
- Uterine bleeding.
- Pain in the lower abdomen.
- Frequent urge to urinate.
- If fibroids grow towards the rectum, stool disturbances and constipation are observed.
Painful sensations may appear during intimacy with a partner.
Treatment for this pathology is prescribed after a full examination, taking into account the individual characteristics of each woman.
Endometriosis
This pathological change in the uterus during the menopausal period is characterized by the growth of the endometrial layer with pathological penetration into the muscular layers of the uterus. Most often it occurs in premenopause, when the menstrual cycle has not yet completely subsided.
Causes symptoms such as:
- painful sensations in the lower abdomen of an aching nature, as well as pain during sexual intercourse;
- prolonged menstruation, when the uterus does not contract for 10-14 days, which is the reason for diagnostic curettage;
- against the background of prolonged menstruation, a disturbance in the psycho-emotional state occurs;
- Infertility may develop.
If one of the presented symptoms appears, you must immediately contact a medical specialist to prevent complications and the development of a more serious pathology.
Chronic form of salpingitis
Salpingitis is an inflammatory process in the fallopian tubes and appendages, which can occur long before the onset of menopause, and with the onset of hormonal changes it can become an aggravated form of the disease. Typically, salpingitis causes symptoms such as:
- Sharp pain in the lower abdomen.
- Increased body temperature.
- Formation of purulent discharge.
In the absence of timely treatment, it can become complicated and lead to the development of pathology requiring immediate removal of the uterus.
Development of the adhesive process
Numerous surgical interventions in the structures of the organs of the reproductive system of the body, as well as inflammatory processes together lead to the formation of adhesions or the spread of connective tissue. With the onset of menopause, a woman’s body experiences a decrease in the toning of muscle fibers.
This leads to anatomical displacement of organs in the pelvis, which causes nagging pain from stretching of the adhesions.
Depending on what kind of disorder occurs in the uterus, appropriate treatment is prescribed. In most cases, if the pathology is not associated with an oncological process, hormone replacement therapy is prescribed. But the dosage and course duration should only be determined by a qualified specialist. Self-medication of any pathology during menopause can result in irreversible consequences.
Useful video on this topic:
What does an enlarged uterus mean?
The most common cause of uterine enlargement is pregnancy. It is also worth considering that with age, the size of the uterus also becomes larger. If the process of change is observed within acceptable limits, then this is normal, but in most cases it is a sign of a pathological condition.
Signs of an enlarged uterus include:
- Constant, aching pain.
- Fluid incontinence appears.
- Discomfort during sexual intercourse.
- Painful sensations during menstruation, as well as the presence of large blood clots.
- Bloating in the lower abdomen.
- Feeling of fullness in the abdomen.
- Lower back pain.
- Migraine.
- Bleeding between periods.
- Loss of weight.
- Changes in the mammary glands.
- A sharp decrease in hemoglobin.
The size of the uterus is normal - the main indicators and causes of deviations
For women's health, you need to take care of your body. This especially applies to the uterus. This organ is responsible for bearing a child, and if abnormalities, infections or pathologies occur, it is necessary to undergo timely treatment.
A woman needs to know about her body, and what sizes of the uterus are normal, and what sizes indicate problems with the health of the reproductive organ.
What happens during pregnancy
During the gestation period, the parameters of the reproductive organs increase due to myocyte hypertrophy. Changes are noticeable from 5-6 weeks. By week 8, the uterus becomes 2 times larger than it was originally. It enters the pelvic cavity only from the 12th week. From 13-14 you can palpate the uterine fundus through the anterior wall of the abdomen.
From the beginning of the 2nd trimester, the doctor determines the height of the uterine fundus and abdominal circumference at each visit to the pregnant woman. These indicators allow us to judge the speed of fetal development in accordance with the term. The distance from the pubic bone to the uterine fundus varies as follows:
A decrease in the height of the uterine fundus in the last stages indicates the body’s preparation for childbirth. In other cases, a discrepancy between the parameters of term and fundal height indicates a violation of fetal development, possible feto-placental insufficiency.
The size of the uterus after childbirth returns to normal gradually. During the first day, the bottom is determined above the navel. Involution accelerates during breastfeeding. It stimulates the release of oxytocin, which leads to myometrial contractions. After a day or two, the bottom reaches the navel, and after another day it descends 2 transverse fingers below. Then every day it decreases by 1-2 fingers. After a week, the uterus is palpated slightly above the womb or begins to hide behind it. If this does not happen, the discharge increases and examination and treatment are necessary. It is likely that a spasm of the cervix has occurred or remains of the fetal membrane remain in the cavity.
Full recovery occurs within a month. During this time, the discharge stops, the volume and parameters of length and width correspond to the norm for women who have given birth. For control, some doctors recommend performing an ultrasound during this period.
Its structure and main functions
The uterus is shaped like a pear. Its peculiarity is compression in the front and back.
Structure of the uterus:
- At the back it is adjacent to the rectum. The front is covered by the bladder. It is held between these organs by strong flexible ligaments. They are penetrated by a network of blood vessels and nerve endings.
- The uterus has three openings or exits. From below, the cervix passes into the vagina. At the location of the bottom of the organ there are exits to the right and left fallopian tubes.
- The bottom of the reproductive organ is located above the line where the fallopian tubes exit. The body itself has the outline of a triangle. They taper as they become the round cervix. It is an extension of the body.
- The cervix has a third of the length of the entire organ . The outer end exits into the upper part of the vagina. This segment is called the supravaginal part. There are edges on the back and front walls. They separate them from each other.
- The visible part of the cervix in the vagina is covered with epithelium . This part contains an important zone in which inflammation processes can occur. The ecclesiastical canal has a mucus plug. A secret comes out of it. It prevents viruses and infections from entering the uterine cavity.
How much does the uterus and appendages weigh?
Diagnosis and treatment
The uterus is an organ of the female reproductive system designed for the development of the embryo and gestation.
Like other internal organs, it has certain sizes, which depend on hormonal levels and will differ in girls, adults and postmenopausal women. Each of these categories has its own standards.
Deviations from them indicate pathology. There are some regularities in changes in the size of the uterus during pregnancy and the postpartum period.
1
Structure of the uterus, dimensions
The uterus is located in the pelvic cavity and is a hollow muscular organ. In girls under 3 years of age, it has a cylindrical shape and is flattened in the anteroposterior direction, then becomes more rounded. In adolescents and adult women, the reproductive organ becomes pear-shaped.
It consists of a body, neck and bottom. The upper convex part is called the fundus, the middle part is the body, which passes downwards into a rounded area - the cervix.
The wall of the uterus has three layers:
- 1. superficial - perimetry (serous membrane);
- 2. middle - the thickest muscle layer, which is called the myometrium;
- 3. internal - endometrium (mucous membrane).
The thickness of the inner layer changes during pregnancy and at different phases of the cycle. During the menstrual phase, if fertilization of the egg does not occur, the superficial part of the endometrium is rejected. Menstruation begins.
From 5 to 14-15 days of the cycle, under the influence of estrogens, restoration of the mucous membrane begins. From 15 to 28 days from the beginning of the cycle, the endometrium thickens to 8 mm.
This occurs under the influence of the hormone progesterone and is necessary for the implantation of a fertilized egg.
The length of the body of the uterus in a newborn girl is 1 cm. By the age of 10, it increases to 3 cm, and in adolescence it reaches 5-5.5 cm. In adult women, this figure averages 7-8 cm.
The width of the uterus at reproductive age is about 4 cm, and the thickness is 2-3 cm. The volume of the cavity is from 4 to 6 cm.
At birth, the reproductive organ weighs only 3.5 g. At the age of 12-15 years - about 6.5 g, and at 16-20 years - approximately 25-30 g. In nulliparous women, the weight of the uterus is about 40-50 g, and in mothers - up to 80-90 g. After menopause, its weight gradually decreases.
In clinical practice, the size of the uterus is calculated using ultrasound (ultrasound), since it is completely located behind the pubic symphysis. Its boundaries can be determined through the anterior wall of the abdomen only after the 12th week of pregnancy or with large fibroids.
Ultrasound of the pelvic organs is a safe and effective diagnostic method, often used in gynecology. Using it, you can examine the structure and size of the female genital organs (ovaries, uterus, appendages), as well as judge the functional state of the reproductive system
During the examination, the doctor evaluates the parameters of the uterus:
- body length;
- anteroposterior size;
- width;
- M-echo;
- myometrial structure;
- condition of the cervix.
Determining the length, width and anteroposterior size gives an idea of the general structure of the organ, the presence or absence of its deformation, developmental defects, and the correspondence of the indicators to the woman’s age.
M-echo is a calculation of endometrial thickness. This parameter has different meanings depending on the phase of the menstrual cycle. It should be homogeneous in structure, anechoic in the first phase, and hyperechoic at the end of the second. M-echo can change under pathological conditions.
Studying the structure of the myometrium allows for the timely identification of myomatous nodes. With fibroids, a tumor-like formation with a smooth, almost always clear contour is determined. If the tumor is located submucosally (under the mucous membrane), a pronounced deformation of the M-echo will be observed, especially in the second phase of the monthly cycle.
3
Women of reproductive age
Healthy women in this group have a regular menstrual cycle. The body produces a sufficient amount of estrogen and progesterone, under the influence of which secretory changes occur in the endometrium. When the egg is fertilized and attaches to the mucous membrane, pregnancy develops. After childbirth, each size of the uterus increases by 0.7-1.2 cm from the original.
Normal sizes of the uterus in adult women (cm):
| Length | 3,6-5,9 |
| Anteroposterior size | 2,8-4,2 |
| Width | 4,6-6,2 |
Endometrial thickness (M-echo) depending on the phase of the cycle, the presence of pathology (mm):
| Start of the first phase | 5-7 |
| End of the first phase | 9-12 |
| End of the second phase | 10-14 |
| Endometrial hyperplasia | 15-20 |
| Endometrial adenocarcinoma | >20 |
4
Postmenopausal women
In postmenopause, the amount of sex hormones produced decreases. A woman can no longer conceive and bear a child. The size of the uterus decreases during this period.
Norms for uterine size after 60 years (cm):
| Length | ≤3,5 |
| Anteroposterior size | ≤2,2 |
| Width | ≤1,3 |
The size of the M-echo during menopause for more than 3 years is less than 5 mm.
5
Changes during pregnancy
During pregnancy, the reproductive organ increases significantly in size, mainly due to stretching of the upper part, which begins to protrude beyond the pubic symphysis.
When examining a pregnant woman, the obstetrician-gynecologist assesses the height of the uterine fundus (UF). This is its upper limit, which can be determined through the abdominal wall.
Measuring the distance from the pubic bone to the UMR allows us to predict the duration of pregnancy and assess the correspondence of the enlargement of the uterus to this period.
Correspondence of VDM to gestational age:
| 8-9 weeks | 8-9 cm | 24-27 weeks | 23-28 cm |
| 10-13 weeks | 10-11 cm | 28-29 weeks | 26-31 cm |
| 14-15 weeks | 12-13 cm | 30-33 weeks | 29-33 cm |
| 16-19 weeks | 14-21 cm | 34-37 weeks | 32-37 cm |
| 20-23 weeks | 18-25 cm | 38-39 weeks | 35-38 cm |
| 40-41 weeks | 34-35 cm |
Deviation of the VDM from the average parameters is possible when
- polyhydramnios;
- oligohydramnios;
- multiple pregnancy;
- delay in fetal development.
Also, during a routine examination, the abdominal circumference is measured. The value of this indicator can be used to judge the intrauterine development of the child and the amount of amniotic fluid.
At 36 weeks, the uterus is maximally enlarged, its upper edge can be felt under the costal arches. The weight of the organ at this time is approximately 900 g.
Restoration of the uterus begins in the early postpartum period. A decrease in its value to the original is facilitated by a drop in the levels of progesterone and estrogens, which were produced by the placenta. A significant role is played by the hormone oxytocin, which is released into the blood when a baby is attached to the breast.
After childbirth, the fundus of the uterus is located between the pubic symphysis and the navel.
The next day, due to muscle relaxation, the upper border rises a little higher - to the level of the navel or 1 cross finger below it.
Then the uterus continues to contract, its size decreases, and after 10 days it becomes inaccessible to external examination. Full recovery occurs individually and takes an average of 2 months.
Ultrasound during pregnancy evaluates the walls and cervix.
Source: https://worldwantedperfume.com/skolko-vesit-matka-s-pridatkami/
Types of examinations for women
A woman seeks help from a gynecologist when unusual abnormalities appear in the menstrual cycle or when planning pregnancy.
When diagnosing a problem, a specialist may resort to the following examinations:
- Manual examination;
- Examination using a gynecological speculum;
- Smear analysis for vaginal microflora;
- Analysis of material to identify viruses and infections;
- Colposcopy;
- Ultrasound examination;
- Hysteroscopy and laparoscopy;
- Taking blood for hormone analysis.
The female uterus - how is the organ structured, what are its sizes and functions at different periods of life?
The female uterus is the central organ of the reproductive system. It is where the birth of a new life, development and maturation of the fetus occurs. The uterus, together with its appendages, forms a unique complex that regulates the functioning of other organs and systems of the body and determines the overall well-being of a woman.
Oncological diseases of the uterus
Women's diseases of the uterus, accompanied by tumor-like processes, are separate from all pathologies of the reproductive system.
In most cases, the provoking factor for their development is chronic inflammatory and infectious processes, hormonal imbalances.
The difficulty of diagnosing these pathologies lies in the absence of an obvious clinical picture, sluggish, latent course. Often a tumor is discovered during a random examination. Among the possible tumor-like diseases of the uterus, it is necessary to highlight:
- fibroids;
- fibroma;
- endometrial cancer;
- polycystic disease
Prolapse of the female uterus
With age, the female genital organs and the uterus may change their location. Often in older women, uterine prolapse is recorded, caused by a violation of the ligamentous apparatus and age-related changes. In most cases, the organ moves downwards, towards the vagina. The disease is accompanied by specific symptoms:
- feeling of pressure;
- discomfort in the groin area;
- pain in the lower abdomen;
- urination disorder (frequent urination, urinary incontinence).
The danger of the pathology lies in the possibility of complications by prolapse of the uterus from the vagina. This situation requires emergency medical care, so you should consult a doctor when the first symptoms appear. Treatment consists of surgical restoration of the integrity of the ligamentous apparatus of the pelvic floor and suturing of the vaginal muscles.
The size of the uterus is normal according to ultrasound during reproductive age
The normal uterine size indicators for each nulliparous woman look different. It is individual in nature. It all depends on the size of the organ. This is considered a third of the length of the uterus.
Basic indicators
The following factors can influence the indicators:
- Endocrine system disorders;
- Number of times of conception, pregnancy and past births;
- Individual indicators of a woman’s body;
- Phases of the menstrual cycle.
Indicators during menstruation can fluctuate from the beginning of the cycle to the end. The minimum values may be on the first day, and the maximum on the last. Normal condition during ultrasound examination of the uterus, the thickness of the mucous membrane depends on the menstrual cycle. On days 5 or 7 this figure does not exceed 6 mm. After two weeks it increases from 7 to 14 mm.
Normal size of ovaries on ultrasound
If a woman has constant pain in the lower abdomen on the right or left side, discomfort during sexual intercourse, or ovulation is painful, then this is a reason to contact a gynecologist for a referral for an ultrasound of the ovaries. First, the doctor conducts an examination.
The parameters of the ovaries should be in the following norm: width – 2.5 cm, length – 3 cm, thickness – 1.5 cm. The volume of one ovary ranges from 2 to 8 cubic cm. If the size, volume, thickness of the ovaries is higher than normal, this may indicate a cyst or oophoritis. With normal performance, functioning and the absence of pathologies of the ovaries, the outlines should be clear and with small tubercles. The echostructure is homogeneous. In healthy ovaries, you can identify follicles of about 0.4-0.6 cm and a dominant follicle - 2.5 cm. If the thickness of the dominant is greater than the norm, it is an ovarian cyst. It is recognized by ultrasound as the formation of liquid, the thickness of which is more than 2.5 cm.
Size of ovaries during reproductive age
| Neck length(cm) | Thickness (mm) | Width (mm) | Volume (cm³) | |
| (M+-SD) | 30+-8 | 19+-6 | 27+-6 | 7,8+-2,6 |
| Individual fluctuations | 20-37 | 16-22 | 18-29 | 3,0-10,0 |
| Fluctuations during the cycle (ovulating ovary) | 25-40 | 25-40 | 15-30 | 4,0-15,0 |
Size of ovaries in postmenopause
| Neck length(cm) | Thickness (mm) | Width (mm) | Volume (cm³) | |
| Postmenopause | 25+-9 | 12+-5 | 15+-6 | 4,5+-0,9 |
| Postmenopause | 23+-9 | 11+-4 | 14+-4 | 3,5+-0,8 |
| Postmenopause | 22+-7 | 10+-4 | 13+-5 | 2,5+-0,8 |
| Postmenopause | 10+-6 | 9+-3 | 12+-4 | 1,5+-0,7 |
At the first alarming signs appearing in the lower abdomen, you must urgently seek advice from a specialist and undergo an ultrasound examination of the uterus, cervix, and ovaries.
The uterus is a hollow muscular organ that performs the reproductive function. Due to the ability of smooth muscles to stretch, the normal size of the uterus fluctuates throughout life. But according to statistical studies, approximate parameters have been determined, deviations beyond which make it possible to judge the pathology. The shape, length and width parameters correlate not only with the woman’s age, but also with her life history. Body type has almost no effect on morphometric parameters.
How does the endometrium change during menopause?
The endometrium is a constantly renewing tissue. In different parts of the cycle, the thickness of the endometrium changes under the influence of certain hormonal changes.
But during menopause, due to significant hormonal disruptions, the cyclical renewal and growth of the functional membrane is disrupted. This leads first to a disruption of cyclicity, and then to the complete disappearance of menstrual flow.
The endometrium during menopause goes through several stages of change, tied to the stages of inhibition of reproductive ability.
- Premenopause. During this period, an anovulatory cycle is established, which is characterized by the absence of ovulation and the phase of formation of the corpus luteum. A transitional form of the endometrium is formed in premenopause, characterized by a slight proliferation of mucous tissue. If the tissue grows slowly and not very quickly, then there is no need to worry. Sometimes cysts appear during this period.
- Menopause. This is the name of the stage of life during which the last menstruation occurs. Before menstruation, the endometrium becomes slightly thicker, but after the last menstruation the layer thins. This is followed by the development of functional hypoplasia.
- Postmenopause. At this stage, for the first 3 to 5 years, the transitional form of the endometrium, formed during premenopause, functions. Over the years, non-pathological atrophy of the layer forms, in which the mucous tissues cease to function.
All of the above changes in the endometrium are natural and not associated with pathologies. But you still need to visit a doctor during menopause to prevent the development of serious pathologies of the uterus and appendages.
Reasons for deviations from the correct dimensions
Changes in the normal size of the uterus, not associated with hormonal changes or age-related characteristics, indicate the development of pathologies.
Why is the size of the uterus reduced?
The main reason for small size is hypoplasia, otherwise underdevelopment of the organ. Pathology occurs due to abnormal formation of the organ or insufficient ovarian function.
There are 3 degrees:
- abnormal anatomical development in the womb - fetal (embryo) uterus, up to 30 mm long;
- children's or infantile, when the length does not exceed 55 mm;
- teenage
Pathology can be diagnosed based on the results of ultrasound or probing.
Why are the sizes increased?
Abnormally enlarged size of the reproductive organ according to ultrasound diagnostics may accompany:
- change in shape (from pear-shaped to spherical);
- growth of the uterine body in length and width;
- expansion of the cavity;
- enlarged ovaries;
- heterogeneous structure;
- thickening of the endometrium and myometrium.
The reasons for the deviations are the presence of hormonal and oncological diseases of the female reproductive system.
The main diseases in which indicators increase include:
- benign neoplasm - fibroids;
- benign tumor of the uterine wall - fibroma;
- multiple cystic formations of paired sex glands - polycystic ovary syndrome;
- displacement of the fundus and cervix – prolapse of the uterus;
- malignant lesion of the uterine body - carcinoma (cancer) of the epithelial layer;
- changes in endometrioid tissue - adenomyosis.
Endometrial norms during menopause
Every change in the condition of the uterine mucosa during menopause should be carefully monitored to prevent the formation of polyps, cancer and other serious pathologies.
The simplest, most convenient and accurate way to detect deviations in endometrial thickness during menopause from its natural value is the ultrasound method.
The normal thickness of the uterine mucosa during menopause should not exceed 5 mm. In some patients, the endometrial lining of the uterus is normal during menopause and is 6–7 mm. In this case, patients should go for ultrasound monitoring every 3 months so that the doctor can monitor the dynamics of changes in thickness indicators and be able to detect endometrial pathologies in a timely manner.
If the thickness of the uterine lining during menopause is more than 7 mm, then we should definitely talk about the disease. To establish a diagnosis, the doctor sends the patient for diagnostic curettage of the tissues of the uterine wall.
If the thickness of the membrane reaches 12 mm or more, then each layer of the mucosa is scraped out separately. The scraped biological material is examined in a histological laboratory. Studying the material is necessary to establish a reliable diagnosis and determine the optimal method of therapy.
Normal sizes of the uterus and ovaries in women of different ages
The size of the uterus depends not only on age, but also on the number of pregnancies.
For nulliparous girls 45-30 years old, the norm is considered to be a neck length from 24 to 34 cm, a body length from 38 to 50 cm. The width of the neck varies from 22 to 32 cm, the body length from 37 to 49 cm. The thickness of the neck is 22-30 cm, body - 28-37 cm.
The organ of women who have only had abortions but never given birth will be larger. The uterus enlarges even more in girls who have given birth once. If there were 2 or more births, the size will increase more.
Forms of endometrial hyperplasia
Endometrial hyperplasia is divided into several forms, depending on which cells of the layer grow pathologically.
- Glandular hyperplasia
. A benign pathology in which glandular cells grow and are improperly located. In this form of the disease, the basal and functional layers are not differentiated, but the secretory ability of the glands is normal. Glandular pathology can turn into glandular-cystic, a severe form characterized by the formation of cysts in the glandular layer. The glandular cystic form is precancerous. - Basal hyperplasia
. A rarely diagnosed variant of the pathology. With this form of development of hyperplasia, there is a proliferation of tissues of the basal (located on the myometrium) layer. - Polypoid hyperplasia
. Also called focal. With this form of pathology, endometrial tissue grows unevenly, which causes the formation of polyps - benign growths on a thin stalk. These tumors come in different sizes. One large polyp may form, or several small tumors may grow. It should be borne in mind that polypoid pathology is also precancerous. - Atypical hyperplasia
. This form of the disease is characterized by intense and heterogeneous pathological changes in the functional layer, often accompanied by tissue degeneration. 10% of patients with this form of hyperplasia develop cancer.
How much does a woman's uterus weigh?
The female uterus is the central organ of the reproductive system. It is where the birth of a new life, development and maturation of the fetus occurs. The uterus, together with its appendages, forms a unique complex that regulates the functioning of other organs and systems of the body and determines the overall well-being of a woman.
How does the female uterus work?
The internal structure of the female uterus is unique. With the onset of puberty, the organ undergoes cyclical changes every month. According to the histological structure, the organ contains three types of tissue:
- The top layer is the perimeter.
It covers the organ from the outside, preventing injury. - The middle layer is the myometrium.
It is represented by bundles of muscle and connective fibers that are highly elastic.This property explains the ability of the reproductive organ to significantly increase in size during the period of bearing a child. Physiologists say that myometrial fibers are the strongest muscles in the female body, capable of withstanding heavy loads.
- The inner layer is endometrial (functional).
This layer itself plays a crucial role during pregnancy - the fertilized egg is implanted into it and grows in it.If pregnancy does not occur, endometrial cells begin to die and leave the uterine cavity along with menstruation.
Where is a woman's uterus?
It should be noted that the female reproductive organs, including the uterus, have some mobility. Taking this into account, the topography of the organ may vary somewhat and depends on the specific stage of life (childbirth, pregnancy).
Normally, the uterus is located in the pelvic cavity, between the rectum and the bladder. It is slightly tilted forward, and on both sides it is supported by ligaments that prevent the organ from descending and ensure the mobility of the organ.
Thanks to the ligamentous apparatus, the female uterus is able to slightly change its location. So, when the bladder is full, the organ tilts backward, and when the rectum is full, it tilts forward.
A significant change in the location of the uterus is observed during pregnancy.
The growth of the embryo leads not only to an increase in the volume of the reproductive organ, but also causes it to extend beyond the pelvic cavity.
What does a woman's uterus look like?
Having briefly examined the structure of the uterus in women, it should be noted that the organ itself externally resembles an inverted pear. In the structure of the organ it is customary to distinguish:
The bottom is the upper part of the organ, convex in shape, located above the line where the fallopian tubes enter the uterus. The body has a cone shape and is the middle large part of the organ.
The lower part of the uterus - the cervix - is divided into 2 sections: the vaginal part - it protrudes into the vaginal cavity, and the supravaginal part - the upper section located above the vaginal cavity. At the junction of the body and the neck there is a narrowing called the isthmus.
On the vaginal part there is an opening of the cervical canal.
Functions of the uterus
The main function of the uterus is reproductive. This organ is continuously connected with the process of procreation. Directly in it the development of a small organism from two germ cells occurs. In addition, there are a number of other functions that the uterus performs:
- Protective. The organ is a barrier to the spread of pathogenic microorganisms and viruses from the vagina to the appendages.
- Cleansing – monthly, along with menstruation, self-cleaning of the cervical canal and vagina occurs during menstrual flow.
- Participation in the process of fertilization is a connecting link on the path of sperm from the vaginal cavity to the fallopian tube.
- Participates in the implantation process.
- Strengthens the pelvic floor along with its own ligamentous apparatus.
Woman's uterus - dimensions
It should be noted that such a parameter as the size of the female uterus has a special diagnostic value. Thus, based on an increase in the volume of an organ, the doctor can make the first assumptions about pathology or pregnancy already at the first stage of the examination, without the use of equipment. The size of the uterus can vary and depends on several factors:
- the presence of pathologies and diseases of the reproductive system;
- presence of pregnancy and childbirth;
- woman's age.
Normal size of the uterus of a nulliparous woman
Diagnosis of diseases of the uterus and determination of the size of the organ is carried out using ultrasound. This hardware method helps to accurately determine structural changes in an organ and establish its exact location. The normal dimensions of the uterus in a woman who does not have children are as follows:
- length – 7–8 cm;
- maximum width – 5 cm;
- weight – about 50 g.
Sizes of the uterus at different stages of pregnancy
Pregnancy is a complex and lengthy process, accompanied by the growth and development of the fetus. The immediate increase in the size of the unborn baby causes the growth of the uterus and its volume.
At the same time, structural changes in the composition of the walls of the organ are observed: not only a qualitative, but also a quantitative increase in muscle fibers occurs.
At the same time, the female uterus increases throughout the entire period of pregnancy.
In the first weeks of gestation, the reproductive organ retains its pear-shaped shape and practically does not change in size, since the embryo is still small.
However, by the second month the organ acquires a rounded shape, and the size of the uterus during pregnancy by this time increases several times.
The weight of the uterus itself also increases, and by the end of the gestation period it reaches almost 1 kg! At each examination of a pregnant woman, the doctor determines the height of the uterine fundus. The change in this parameter by week of pregnancy is shown in the table below.
Dimensions of the uterus after childbirth
After delivery, the female uterus begins to gradually recover. It decreases in size and its weight decreases. This process takes on average 6-8 weeks.
At the same time, the process is proceeding at a rapid pace. So, by the end of the first week, on days 6–7 after birth, the uterus weighs approximately 500–600 g, and already on the 10th day after the baby is born – 300–400 g.
Normally, at the end of the third week, the organ already weighs 200 g.
It should be noted that the process of involution has an individual character. By diagnosing the size of the uterus by ultrasound, the norm of which is given below, doctors draw conclusions regarding the speed of restoration of the reproductive system. Doctors call the determining factors:
Size of the uterus at menopause
Menopause is a period of cessation of menstrual flow, accompanied by functional and structural changes in the uterus. The hormonal system produces fewer sex hormones, which is why the endometrium stops maturing and new cells are no longer formed. This leads to a decrease in the volume and size of the reproductive organ. This is confirmed by the smaller size of the uterus on ultrasound.
Thus, in the first 5 years from the onset of menopause, according to experts, the volume of the female uterus becomes 35% smaller. At the same time, its size decreases in length and width by 1–2 cm. The reduction in the size of the reproductive organ stops 20–25 years after the onset of menopause (at 70–80 years). By this time, the organ is only 3–4 cm long.
Uterine diseases - list
Uterine diseases in women can occur at any age. However, according to the observations of doctors, hormonal changes in the body are often the trigger for their development.
This confirms the high frequency of development of pathologies of the reproductive system during puberty, after childbirth and during menopause. Most pathologies of the uterus are inflammatory and infectious processes in the reproductive organ.
Among the common diseases of this organ are:
- Inflammatory processes: metritis, endometritis, adnexitis.
- Pathologies of the uterine cervix: erosion, ectopia, dysplasia, cervical cancer.
- Acute conditions associated with the uterus: ectopic pregnancy, ovarian apoplexy, spontaneous abortion.
- Tumor-like processes: myoma, fibroma.
Congenital pathologies of the uterus
Diseases of the uterus that occur during the embryonic development of the reproductive system and the formation of the genital organs are called congenital. Among the common pathologies of this kind, the following should be noted:
- Bicornuate uterus - formed as a result of non-fusion of parts of the Müllerian canals. There are different types of pathology:
- Saddle-shaped - a case when only the bottom of the organ is divided.
- A uterus with an incomplete or complete septum - the shape does not change externally, but a septum appears in the cavity, partially or completely separating it.
- Separate body with a common neck - formed by the fusion of the Müllerian ducts in the neck area.
- Duplication of the uterus - not only the body of the uterus is divided, but also the cervix.
Infectious diseases of the uterus
Infectious female diseases of the uterus are the most common type of pathology of this organ. They can arise due to banal non-compliance with the rules of intimate hygiene.
Often the spread of an infectious agent occurs through sexual contact, so women of reproductive age are more often exposed to diseases.
Pathology is almost always accompanied by changes in microflora, so additional symptoms appear that make it possible to identify the disorder (itching, burning in the perineal area, hyperemia). Common infections in women include:
Source: https://prodyhanie.ru/skolko-vesit-matka-zhenshhiny/
Diagnosis of pathological changes in endometrial thickness
It is extremely difficult to calculate the signs of pathological uterine growth; endometrial hyperplasia in postmenopause practically does not make itself felt for quite a long time. The first obvious sign of pathology is bleeding, which appears when the lining of the uterus becomes too thick. If this symptom appears, you should immediately go to the doctor. Other symptoms of endometrial hyperplasia during menopause appear extremely rarely.
Some patients experience slight grayish-white vaginal discharge. There are no pain or other signs of deviation of endometrial thickness from normal.
In most cases, women learn about their diagnosis during a routine examination with a gynecologist. In patients who regularly visit the gynecological office during age-related changes in hormonal levels, pathological processes in the ovaries, uterine cavity and fallopian tubes are detected in a timely manner. Using a gynecological speculum, glandular-cystic and polypoid hyperplasia can be clearly seen.
The main task of the doctor is to determine whether the patient has normal uterine endometrium during menopause. The thickness of the mucous membrane is determined through an ultrasound procedure. Typically, ultrasound monitoring is carried out transvaginally, but in advanced and complicated forms of pathology, the diagnostic procedure is carried out using radioactive phosphorus isotopes.
Based on the results of diagnostic studies, the medical specialist prescribes the most appropriate therapy for the patient.
How much does the uterus with appendages and ovaries weigh?
Women who have been diagnosed with a condition that requires removal of the uterus and appendages feel like their world is collapsing. Depression sets in and fears appear. How will life change? What will happen to the appearance? How will the operation affect your sex life? Let's try to understand this situation.
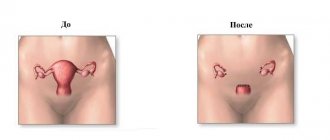
What is hysterectomy
In gynecology, such surgical intervention is prescribed to save a woman’s life when serious diagnoses are made. Before making a decision, doctors weigh the pros and cons.
Hysterectomy with appendages is an operation to remove the uterus along with the cervix, fallopian tubes and ovaries. After it, a hormonal imbalance occurs, the woman is deprived of childbearing function.
She receives psychological trauma, which she cannot always cope with.
Indications for removal of the uterus and appendages
Gynecologists, when prescribing an operation, pay close attention to the woman. Removal of the uterus after 50 years, from a psychological point of view, is less traumatic. The woman is past childbearing age. Until menopause has occurred, they try not to remove the ovaries. Operation is necessary when its cost is life. The indications are:
- prolonged uterine bleeding;
- cancer of the female genital organs;
- endometriosis;
- large uterine fibroids;
- uterine injuries;
- prolapse, loss of genitalia;
- active growth of fibroids during menopause.
Preparing for uterine amputation surgery
It all starts with collecting tests and examinations. When planning to remove the ovaries and uterus, they do:
- general tests;
- checking blood for the presence of venous diseases;
- colonoscopy – examination of the cervix and vaginal walls for the presence of tumors and cysts;
- biopsy and smear taken;
- cytological and biopsy examination of tissues;
- examinations to rule out inflammation in the body.
After it becomes clear that the woman is ready for extirpation of the uterus and appendages, the following procedures are performed:
- prepare donor blood;
- give an enema to cleanse the intestines;
- install a catheter to remove urine;
- consult a vascular surgeon;
- if there is a likelihood of blood clots forming in the veins of the lower extremities, apply a tight bandage with an elastic bandage;
- give medications.
How is hysterectomy performed and how long does it last?
Surgery is performed using full anesthesia. The process is complex and takes several hours to complete. Depending on the volume of intervention, they differ:
- extirpation - removal of the uterus and cervix;
- supravaginal amputation of the uterus - removal without the cervix;
- panhysterectomy – removal of the uterus and appendages;
- extended operation of extirpation of the uterus with appendages - lymph nodes and pelvic tissue are additionally removed.
Depending on the complexity of the situation and diagnosis, the operation is performed in various ways. There are different types of surgical intervention:
- Laparoscopic extirpation. It is performed for small fibroids. Removal of the uterus using the laparoscopic method is carried out using special equipment. Several holes are made in the abdominal wall through which instruments are inserted. Laparoscopy allows for quick recovery after surgery.
- Vaginal hysterectomy is performed externally, through the vagina.
- Laparotomy - abdominal surgery - is performed in difficult cases. The cause may be a large fibroid or a cancerous tumor. It is indicated in situations where it is necessary to remove not only the uterus, adnexal organs, but also lymph nodes. The operation is performed through an incision in the anterior abdominal wall. This gives you a complete overview of the organs. This is important for cancer symptoms to find out the area affected. Look at the photo to see how the female reproductive organs are located.
Consequences
The operation of removing the uterus leads to hormonal imbalance in the body. Young women are especially sensitive to it, because menopause occurs abruptly.
The post-castration period is characterized by symptoms:
- change of mood;
- increased fatigue;
- chronic fatigue syndrome;
- tides;
- anxiety;
- suspiciousness;
- depression.
After extirpation of the uterus, menstruation ceases and reproductive function is excluded. For young women this is a huge psychological problem; they begin to feel inferior.
There is a decrease in sexual desire, pain appears during sex. In the absence of psychological support, serious problems in relationships are possible.
After operations related to cancerous lesions, disability is not excluded.
The operation is very serious, so complications are likely to occur in the post-hysterectomy period. Problems with blood vessels arise - blood clots may form. In addition, there may be:
- bleeding;
- suppuration;
- peritonitis;
- formation of hematomas;
- adhesions after surgery;
- sepsis;
- injuries to neighboring organs during surgery.
Life after hysterectomy
To prevent a woman from feeling depressed, she needs the support of loved ones. Sometimes you need to see a psychologist. It is important to remember that life does not end after amputation of the uterus.
The recovery period will pass, it is necessary to undergo periodic examinations by a gynecologist. To eliminate problems associated with menopause, he will prescribe hormone replacement therapy (HRT).
These may be new generation products - a gel or patch containing estradiol. The cost of the drugs is reasonable.
Postoperative period
It is very important to begin treatment immediately after surgery. Prescribe pain relief, use of vaginal suppositories, infusion therapy - droppers with special solutions. In addition, there are recommendations:
- start early activation;
- treat seams daily;
- be sure to wear a bandage;
- perform physical therapy exercises.
Discharge
Often after surgery, discharge is observed for several weeks. These phenomena are not dangerous and are considered normal. Inflammatory processes may be occurring. You should consult a doctor if the discharge:
- with pus, have an unpleasant odor;
- profuse, as with menstruation, bright red in color;
- bloody, with clots;
- Brown color.
What can you eat after surgery?
Immediately after surgery, a diet is prescribed that starts bowel function. After the operation, hormonal levels change, and women begin to gain excess weight. You need to watch your diet:
- eat more fruits and vegetables;
- main meal before lunch;
- exclude flour and sweets;
- spend fasting days;
- drink more water.
Rehabilitation
To recover faster after surgery, you should take a number of measures. You need to rest more and not overload yourself with work. Long sleep and walks in the air are encouraged. In addition, rehabilitation includes:
Source: https://o-kak.ru/skolko-vesit-matka-s-pridatkami-i-jaichnikami/
Treatment of endometrial hyperplasia
Since gynecological diseases during menopause are caused primarily by hormonal changes, treatment of hyperplasia and other pathologies of the uterus is carried out using hormonal medications. In advanced situations, surgical intervention is prescribed.
The pathological process that occurs with the mucous membranes of the uterus at the stage of menopause is eliminated with the help of the following medications.
- Gestagens
. Preparations based on female steroid sex hormones (Duphaston, Dydrogesterone, Gestrinone). The course of therapy lasts from 3 to 6 months, after which control ultrasound monitoring is done. These medications are indicated for all patients whose endometrium grows during menopause. - Gonadotropin-releasing hormone agonists
(Zoladex, Sinarel, Diferelin, Buserelin). Prescribed to patients over 50 years of age. Used to treat hyperplasia, endometriosis, fibroids, and infertility. Treatment with these drugs should not last longer than six months, since their active components cause deterioration in women's health and increase menopausal symptoms. - Intrauterine devices
. They affect only the mucous membrane of the uterus and do not affect other tissues and organs of the reproductive system. In the first 6 months of wearing the IUD, there is a high risk of uterine bleeding. The device should be worn for 5 years.
Surgical intervention involves scraping out the entire overgrown layer and sending the biological material for study to a histological laboratory. After the operation, the patient is prescribed maintenance hormonal medications.
Causes of fibroids
The causes of benign uterine tumors are still not fully known. Uterine fibroids are a disease that is regulated by hormonal levels. Based on this, the main cause of uterine fibroids is hormonal imbalance. Factors that provoke the appearance of fibroids also include:
- Poor nutrition . Excessive consumption of sweet, flour, and fatty foods leads to excess weight gain and hormonal disorder, which causes the formation of myomatous tumor.
- Surgical and gynecological interventions : frequent abortions, installation of spirals, difficult childbirth - all of these factors cause the formation of cracks, which during the healing process become overgrown with layers of dense muscle tissue, which over time can grow into a tumor.
- Irregular sex life . Rare sexual intercourse causes stagnation of venous blood, which can lead to hormonal instability and, as a result, the development of a uterine tumor.
- Diseases of hypertension and diabetes . With these diseases, metabolism is disrupted, which can lead to obesity or hormonal imbalance, which in turn provokes the development of a tumor.
- Genetic predisposition . There is a high probability that uterine fibroids can appear from generation to generation.
Reviews
Zoya, 53 years old: With the onset of menopause, fibroids began to grow at tremendous speed. All this was accompanied by bleeding, hemoglobin dropped significantly - I felt disgusting. When the surgery was scheduled, I calmed down that everything would be over soon. The recovery was very fast, without complications. My children and husband supported me. Women, don't be afraid of surgery!
Anastasia, 35 years old: When they told me that I had cancer and needed to have my uterus removed, it seemed like my life was over. She cried for a week. I was afraid that my husband would find out and our family life would end. He was very upset, especially since our daughter is still small. He just said that we will fight together. I went through chemotherapy, my hair fell out, but I’m alive. Surgery is a necessity!
Anna, 42 years old: I can’t describe what I experienced; a year ago, I was diagnosed with uterine fibroids and amputation surgery was recommended. Am I no longer a woman? Will I become an old woman? My husband is young - so there won’t be any more sex? Thank you, the gynecologist explained everything. It's all over now. She recovered after the operation. With sex, everything became even cooler. Take the operation more calmly.
The female uterus is the central organ of the reproductive system. It is where the birth of a new life, development and maturation of the fetus occurs. The uterus, together with its appendages, forms a unique complex that regulates the functioning of other organs and systems of the body and determines the overall well-being of a woman.
Life after hysterectomy
Even more interesting:
Ulcers due to thrush in women
Pits on fingernails reasons photo
To prevent a woman from feeling depressed, she needs the support of loved ones. Sometimes you need to see a psychologist. It is important to remember that life does not end after amputation of the uterus. The recovery period will pass, it is necessary to undergo periodic examinations by a gynecologist. To eliminate problems associated with menopause, he will prescribe hormone replacement therapy (HRT). These may be new generation products - a gel or patch containing estradiol. The cost of the drugs is reasonable.
Postoperative period
It is very important to begin treatment immediately after surgery. Prescribe pain relief, use of vaginal suppositories, infusion therapy - droppers with special solutions. In addition, there are recommendations:
- start early activation;
- treat seams daily;
- be sure to wear a bandage;
- perform physical therapy exercises.
Discharge
Often after surgery, discharge is observed for several weeks. These phenomena are not dangerous and are considered normal. Inflammatory processes may be occurring. You should consult a doctor if the discharge:
- with pus, have an unpleasant odor;
- profuse, as with menstruation, bright red in color;
- bloody, with clots;
- Brown color.
What can you eat after surgery?
Immediately after surgery, a diet is prescribed that starts bowel function. After the operation, hormonal levels change, and women begin to gain excess weight. You need to watch your diet:
- eat more fruits and vegetables;
- main meal before lunch;
- exclude flour and sweets;
- spend fasting days;
- drink more water.
Rehabilitation
To recover faster after surgery, you should take a number of measures. You need to rest more and not overload yourself with work. Long sleep and walks in the air are encouraged. In addition, rehabilitation includes: