Cervical fluid is a secretion produced by glands located in the cervix. Thanks to this secretion, it is possible to study changes in the level of estrogen in the blood. Based on the analysis of cervical fluid, you can get a complete picture of the processes occurring in the reproductive system.
For example, at the very beginning of the cycle, cervical fluid is produced in a small volume. The secretion itself has a thick consistency, which is why sperm cannot move freely through the cervical canal.
If cervical fluid gets on your fingers before ovulation, they may stick together. Such a secret is an insurmountable obstacle for sperm. At this time, the color of the secretion is either whitish or yellow. The environment of this liquid is acidic.
Thus, nature itself creates a barrier to sperm, since this period of the cycle is not suitable for conception. Although a slight possibility of conception remains. Therefore, a plug created by cervical fluid is not an absolute protection against pregnancy.
Causes
In addition to the mentioned cases, which are natural moments in the life of every woman and are periodically repeated, the appearance of fluid in the retrouterine space can also occur due to illness. It is possible that there is an inflammatory process in the woman’s genitals that is progressing. In this case, it is very likely that inflammatory exudate occurs behind the uterus.
If acute endometritis has developed, and this is especially true for the period after an abortion, then free fluid often collects in the pelvis. When performing an ultrasound scan, such fluid can be detected in a number of diseases. For example, if there is peritonitis, purulent salpingitis, ascites, hemoperetonium. With endometriosis and pelvioperitonitis, as well as a number of other pathological conditions, such fluid is also found.
Thus, with the formation of endometriotic cysts, abdominal pain becomes more pronounced and irritation of the peritoneum occurs. As a result, microperforation of the cysts occurs, so the contents leak into the abdominal cavity, so a certain amount of free water forms behind the uterus. If there is heavy bleeding in the abdominal cavity, then in this case, fluid accumulates in the retrouterine space.
If purulent salpingitis has developed, often the accumulated pus breaks through and ends up in the peritoneum. This condition leads to diffuse peritonitis, and then immediate surgical intervention is necessary. You should know that such a development of events is quite rare for pus coming out of the fallopian tube to enter the uterus or pelvic area.
An ultrasound echogram can reveal pelvioperitonitis in the abdominal area. In this case, peritoneal fluid can also enter the place behind the uterus. Moreover, the quantity is always different. Sometimes this is very small, sometimes the volume of liquid is quite significant.
What else could fluid collected in the pelvic cavity indicate? It is possible that the patient suffers from an oncological disease that occurs secretly. Something similar is observed with ovarian tumors. In addition, the development of oncology can be supplemented by ascites, that is, the accumulation of transudate in the abdominal cavity.
If an ultrasound is performed on a patient of childbearing age, and free fluid is found in the pelvis, and a fertilized egg surrounded by blood clots is detected outside the uterus, the doctor will most likely diagnose an ectopic pregnancy. Accumulation of water is also caused by other reasons, in particular, diseases of various organs of the abdominal cavity, for example, similar symptoms can accompany liver disease.
As a rule, a woman learns about the presence of fluid in the retrouterine space when an ultrasound is performed. And if the disease has a hidden course, then this diagnosis is of particular value, since it immediately indicates the presence of serious health problems.
This allows the doctor to make an accurate diagnosis and determine what type of therapy is optimal. If an ultrasound showed that there is fluid in the retrouterine space, but there are no other signs of the disease, then there is no need to worry about this; most likely, everything is in order with the patient’s health.
Contributing Factors
Today, doctors name factors that may explain why fluid accumulates in the retrouterine space. Although they are indirect, they should not be ignored. Here we are talking about the notorious bad habits, promiscuity in women, leading to complications in the sexual sphere and many diseases.
Alcohol abuse also falls into the category of bad habits. Surgeries on the uterus are also a contributing factor. Particular attention should be paid to a sedentary lifestyle, a meager diet lacking the necessary set of vitamins and microelements. All this is an essential prerequisite for the accumulation of fluid behind the uterus.
Still, most often, a complication occurs when there is a hormonal change before menopause, when the patient is prescribed hormonal therapy. In some cases, the presence of fluid is diagnosed even without special studies. The fact is that the uterus sometimes greatly enlarges, causing deformation of the abdominal cavity, which is noticeable during a routine gynecological examination.
In addition to the increase, other symptoms also occur. For example, pain of varying intensity, copious watery discharge, impaired urination. It may be rapid or defined as difficult.
The condition is often accompanied by an increase in temperature. You need to monitor your health and regularly visit a doctor for preventive purposes.
2015 - 2021, . All rights reserved.
Regular visits to the gynecologist are not a whim of the doctors themselves. All representatives of the fair sex should visit a doctor several times a year. Often women neglect this instruction and come for examination only when any signs appear. However, one should not lose sight of the fact that some pathologies in the reproductive organs may not appear for a long time. This is how the fluid behind the uterus behaves, the detection of which most often comes as a surprise to the woman.
What discharge is considered normal?
The structure of the mucus helps sperm move into the fallopian tube, where they will meet the egg. It becomes transparent, viscous and no longer so liquid.
The color of the discharge is considered normal, ranging from milky white to light yellow. They should not have any admixture of pus or a large amount of blood.
Vaginal mucus after ovulation - visual table:
| Discharge color | What they look like | Cause |
| Whitish | Scarce. May acquire a creamy or jelly-like structure | Increasing concentration of progesterone with decreasing estrogen levels |
| Transparent | Slight, sticky, stretchy. Reminds me of snot | The ovaries activate the formation of secretion, which contains epithelial cells, mucus from the work of the sweat and sebaceous glands |
| Mixed with blood | Minor smear of pinkish, red or brown color, disappearing after 2-3 days | Implantation of the fertilized egg into the uterine wall with damage to small vessels |
| Yellowish | Scanty, not causing burning or discomfort to the woman. Do not have a strong odor | Presence of epithelial cells in mucus |
| Thick white | Light and not causing discomfort | Completed conception: such a secret closes the cervix, preventing the penetration of microbes to the fetus |
The following video details the variations of normal vaginal fluid after ovulation:
Liquid formations: natural process or pathology?
The presence of free water in the Douglas space is not a disease, but may be a symptom of pathology. Fluid behind the reproductive organ or in the paraovarian areas accumulates in the middle of the menstrual cycle, after the onset of the ovulation process. This is a normal phenomenon and does not require specific treatment. It means the release of the egg from the follicle and the possible occurrence of pregnancy.
Quite often, free fluid behind the uterus is a sign of pathology of a woman’s internal organs. It is extremely difficult to determine the exact volume of such a formation on ultrasound, because it spreads between the reproductive organs. Doctors have developed certain criteria to assess the condition of the fluid in the retrouterine space (the length of the vertical level of the formation is measured):
- accumulation of water up to 10 mm is considered insignificant;
- from 10 mm to 50 mm - moderate stage;
- more than 50 mm - significant.
The volume of water behind the uterus is compared with the woman’s menstrual cycle. If the doctor has suspicions about the cause of the presence of a large amount of water behind the uterus, he may order additional instrumental tests.
Discharge as a sign of ovulation in a woman
The type, consistency and amount of discharge provide an additional opportunity for a young woman to determine the best time to conceive a baby. By the quality of mucus secreted from the cervical canal at any stage of the monthly cycle, hormonal problems can be identified.
It is important to know: analyzing discharge is not the most reliable and revealing method for a beginner. It works better in combination with other signs and methods of calculating ovulation. It is better to purchase tests for LH - they determine fertility with a high accuracy of 99%, or measure fluctuations in basal temperature for at least three cycles in a row to determine the day the egg is released.
Discharge during ovulation, before and after it
Vaginal secretion in the first half of the cycle
Before the onset of the ovulatory period, the level of estrogen in the body increases, peaking approximately two weeks before the end of the cycle (the peak can be detected by the nature of the discharge - it is liquid mucous and stretches well).
About 3-7 days before the release of the egg, clear or translucent white cervical mucus is viscous and sticky, with a creamy texture and is secreted in small quantities. This consistency makes it difficult for sperm to move (infertile period of the cycle).
How many days before the release of the egg does secretion (egg white) begin?
During the preovulatory period, some women do not notice any changes in their cervical mucus at all. Basically, vaginal discharge with the consistency of raw protein is a clear signal of imminent ovulation (within a day or two). Both options are normal, for some the method is suitable, for others it is not.
Any bloody or brownish discharge after the end of menstruation and before the onset of the ovulatory period should be alarming and require consultation with a doctor.
Discharge before and after ovulation by day in a 28-day cycle*
*Data are averaged and are based on a cycle length of 28 days. CI is assessed subjectively, so individual deviations are possible.
Ovulation process as one of the reasons
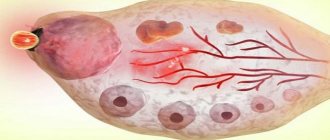
Ovulation is a natural process in which water accumulates in the pouch of Douglas. It does not cause serious problems, since a small amount of liquid is formed. The ovulation process occurs as follows:
- follicles are formed first;
- one of the vesicles outstrips the growth of the others, and the formation of an egg occurs in it;
- liquid formation reaches up to 20-25 mm in diameter;
- then the follicle ruptures so that the egg leaves the membrane and begins to move towards the reproductive organ.
In a healthy woman, the ovulation process occurs monthly. When a cell is released from the follicle and travels to the uterus, this is ovulation. There is fluid in the follicle, but it is very small. If the bubble ruptures, water can enter the abdominal cavity. On an ultrasound, the doctor will see a small amount of it, which is normal. The liquid resolves after a few days and does not cause any discomfort to the woman. In addition to ovulation, the formation of water in the retrouterine space can occur for such natural reasons as early puberty, menstruation.
How many days is mucus secreted during ovulation?
The method of observing cervical mucus allows you to determine the fertile phase by changes in the nature of the cervical mucus.
A woman's cervix produces a specific fluid - cervical mucus, which is necessary, in particular, to maintain the life of sperm located in the female genital tract. Since the environment in the vagina is acidic, cervical mucus has an alkaline environment, protecting sperm from death. Cervical mucus is also necessary for sperm movement. That is, its functions resemble those of male seminal fluid. The cervical mucus itself changes during the menstrual cycle under the influence of hormones (estrogen): long before ovulation, no mucus is produced or very little is produced, then production increases, and closer to ovulation, that is, during the greatest possibility of conception, the mucus becomes more liquid, reminiscent of egg protein. If there is not enough mucus, or it is not the right consistency, fertilization will not occur, since the sperm will either die or will not be able to reach the fallopian tubes, where fertilization occurs.
Immediately after menstruation, there is no or very little mucus. The vagina feels dry or feels slightly wet. These days there is no ability to conceive. These days are called dry days.
After a few days, the nature of the mucus changes: it becomes a glue-like consistency. Sperm cannot exist in such mucus, but the likelihood increases, especially if such mucus is observed very shortly before ovulation.
Next, the mucus continues to liquefy and becomes like a thick cream. This mucus may be cloudy, white or yellowish. During this period, a feeling of moisture appears in the vagina, and marks appear on the underwear. Such mucus is already suitable for the life of sperm and their advancement. During these days you should refrain from
Source
Formation of hemorrhage in the pouch of Douglas
The fluid behind the uterus may be bloody. This kind of education is not the norm. The occurrence of bloody discharge in the pouch of Douglas means the presence of a pathology that can lead to the formation of apoplexy. Causes of hemorrhage:
- vessel rupture;
- the presence of a follicle cyst;
- ovarian cyst or stroma.
After the integrity of the ovarian tissue is broken, water is released into the abdominal cavity. The formation of bloody fluid in the retrouterine space causes pain, weakness, and dizziness. In this case, the woman experiences discharge of a characteristic color - red or dark brown.
Liquid in the space of Douglas may turn into clots. The main reasons for this phenomenon are:
- permanent injuries;
- hard sex;
- lifting weights;
- hyperemia;
- inflammatory process;
- dilated vessels.
Such pathologies cannot be allowed to occur. If a girl knows about the presence of diseases in the female part, then she should visit a gynecologist and be treated to prevent apoplexy and subsequent penetration of fluid into the retrouterine space.
Changes in mucus during pregnancy
In early pregnancy, cervical mucus thickens. It forms a dense plug that prevents infection from entering the uterus. This protects the fetus from environmental influences and infectious agents.
When the body prepares for childbirth, the plug comes out. This may happen several weeks before or just before delivery.
Liquefaction of the plug means the appearance of pathological reactions. There are several possible reasons:
- the appearance of an infection that is mixed with the mucous component.
Both conditions are dangerous for the fetus and require immediate medical attention.
Other conditions for the formation of pathology
The formation of water in the Douglas space is often the cause of some pathological process occurring in the internal reproductive organs of a woman. Doctors identify many diseases that can lead to fluid accumulation. These include the following pathologies:
- inflammatory process in the surface layer of the endometrium (endometritis);
- inflammation in the kidneys, liver, heart failure lead to the formation of ascites, as a result of which free fluid flows into the pelvic organs;
- benign formations characterized by limited growth of the endometrium in the form of a tubercle on a thin stalk;
- an infectious disease accompanied by unilateral or bilateral inflammation of the fallopian tubes (salpingitis);
- adnexitis (inflammation of the ovaries and fallopian tubes);
- oophoritis.
The formation of fluid in the pouch of Douglas may indicate the presence of an ectopic pregnancy, in which a pregnancy test will show a positive result. In addition, this phenomenon causes endometriosis, the appearance of endometrioid cysts on the ovaries, and a condition after an abortion. If you find an accumulation of fluid behind the uterus on an ultrasound, you should not panic. A competent doctor will prescribe appropriate treatment, consult the patient and give recommendations on tactics for the woman’s further actions.
Free fluid in a woman's abdomen, behind the uterus, is often found on ultrasound. If there is little fluid, its presence is not considered a pathology. Often fluid accumulates after menstruation or during ovulation. But in some cases, fluid behind the uterus on ultrasound data should be a cause for concern.
There is fluid, but no problem
Nothing “like that” should be found in the cavity of Douglas. However, there are a few cases where a small amount of fluid may still be present in the retrouterine space, and this is completely normal and does not require treatment. The natural processes that occur in a woman’s body are to blame for its accumulation, namely:
- throwing in a small portion of blood during menstruation (which is completely safe). During menstruation, the endometrium, along with menstrual blood, penetrates into the abdominal cavity;
- ovulation. When the capsule of the follicle bursts and the mature egg comes out to meet the sperm, a small part of the fluid that is released can also enter the space behind the uterus. After a couple of days it is absorbed;
- period of puberty in girls and young girls.
If the diagnostician saw fluid in the retrouterine space (in a small amount) during an ultrasound examination of the patient, then he does not immediately make a final diagnosis. The doctor watches for some time to see how the situation develops further. If a subsequent ultrasound reveals that the fluid has resolved, this indicates that everything is “going according to plan”: ovulation has completed normally.
Causes of fluid accumulation
Sometimes fluid behind the uterus appears due to an ectopic pregnancy; in this case, an ultrasound does not detect a fertilized egg in the uterine cavity. However, the patient's pregnancy test will show a positive result.
Also, fluid in the cavity behind the uterus is diagnosed on ultrasound due to endometriosis. The disease is characterized by the growth of endometrial tissue outside the uterus. Endometrial cells bleed during menstruation, which causes blood to appear in the abdominal cavity.
In addition, fluid behind the uterus is detected on ultrasound with purulent salpingitis, endometritis, rupture of the ovary or its cyst. A large volume of fluid indicates more serious diseases, such as malignant ovarian tumors and a number of other pathologies (heart or kidney failure, cirrhosis of the liver), as well as heavy internal bleeding due to injuries in the abdominal area.
Fluid behind the uterus during ovulation
When the dominant follicle ruptures, its contents enter the retroperitoneal space. In this case, the specialist may detect some fluid around the uterus on the ultrasound image. Soon after ovulation it will resolve without treatment or health consequences.
Fluid behind the uterus with inflammation
Sometimes inflammatory processes cause the appearance of exudative fluid in the abdominal cavity and behind the uterus; ultrasound can reliably diagnose it. As a rule, this occurs due to rupture of the pyosalpinx, an accumulation of pus in the lumen of the fallopian tubes. If an ultrasound showed fluid in the uterus, inflammation of the genitourinary organs is possible.
The inflammatory process is accompanied by fever and pain in the lower abdomen. If the diagnosis is confirmed, the specialist may prescribe medication (antibiotics) or recommend surgery.
How does cervical mucus change in different phases of the menstrual cycle?
There are some descriptions of discharge characteristics that can help determine the different phases of your menstrual cycle.
| Cycle phase | Characteristics of cervical mucus |
| Before ovulation | In the first few days after your period, you may experience very little or no discharge. The area around the vulva can often be dry and the chance of getting pregnant is close to zero. |
| Ovulation approaching | There is a sticky and moist secretion that is usually creamy or white in color. Usually the discharge does not stretch much between the fingers when the cervical mucus stretching symptom is checked. Its volume increases as it approaches the release of the egg, and the color becomes less transparent. |
| During ovulation | At this stage, the CS looks more like egg white, and it is mostly liquid and pronounced - there is a lot of it. It stretches over a longer distance before breaking. The volume peaks sharply during ovulation, when the possibility of conception is high. |
| After ovulation | The discharge returns to its previous state, breaks easily when stretched between the fingers and its volume decreases. The vulva area also becomes dry. |
*Days are based on an average (28 day cycle)
It is possible to misindicate the phase of the cycle if cervical mucus is confused with sperm, and therefore care should be taken when checking for the symptom of stretched cervical mucus. Additionally, there are other factors that can lead to misinterpretation, such as medical conditions, vaginal infections, and birth control methods.
After tracking changes in cervical mucus, you may find that most of the time during ovulation it is not promoting fertility (not as described). In addition, it may be sticky and thick rather than elastic and liquid. This can be caused by stress, diet, hormonal factors or even medications. You can follow these tips if you encounter these problems:
- Drink plenty of water to avoid dehydration.
- Use FertileCM, which is a dietary supplement that increases cervical mucus production.
- Finally, you can use a special lubricant that will help sperm, such as Pre-Seed. It has a consistency and pH similar to cervical mucus. This can help sperm survive and reach the egg to fertilize it.
Decoding the result
Determining the exact volume of fluid behind the uterus using ultrasound data can be difficult due to the two-dimensional nature of the image. In addition, the fluid spreads between the organs, which also makes it difficult to determine its exact volume. In modern medicine, it is customary to distinguish the height of the formation, correlating the volume of liquid with it. With a height of up to 10 mm, the volume of liquid is considered insignificant, from 10 to 50 mm - moderate. At a height of more than 50 mm, the volume of fluid behind the uterus, diagnosed by ultrasound, is considered significant.
The appearance of fluid behind the uterus can be caused by a serious illness. One of which is pelvic inflammation, which often requires hospitalization.
Sometimes during an ultrasound, the doctor detects free fluid in the retrouterine space. Normally there should be no fluid, so it may be evidence of a disease.
Determination of fluid in the uterus using ultrasound
Inspection of the anatomical depression in front of the rectum is carried out with a longitudinal scan, when the body and cervix are completely removed. The doctor can indirectly determine the fluid level or volume. In the latter case, it is necessary to use two projections to obtain three mutually perpendicular dimensions, the product of which should then be multiplied by a special coefficient - 0.523.
In most cases, the diagnostician at the conclusion of the study simply indicates the conditional volume of the contents of the pocket: in small, moderate or large quantities
.
Ovulation
The only cause of fluid accumulation without an accompanying disease. During the release of a mature egg, the follicle reaches a large size and ruptures to release the mature egg. At this time, it becomes possible for fluid to enter the peritoneum. What causes its accumulation behind the uterus. However, a qualified specialist will distinguish this case (indicating that ovulation has occurred) from the disease, since the amount of fluid is very small - the norm. After 2 - 3 days it will resolve.
Method of contraception
To protect against unplanned pregnancy, it is possible to use a natural contraception method by monitoring the quantity and quality of your discharge. To do this, you need to be careful, write down all the phases of the cycle, calculate the days when it becomes possible to use interrupted sexual intercourse.
The secretion changes when you change your diet or take medications (antibiotics, hormones, corticosteroids). These circumstances are taken into account when using this method of contraception.
How cervical mucus changes in different phases of the menstrual cycle and determining fertility by the nature of the secretion
To determine the consistency of the discharge, you need to take a sample from the vagina with your fingers and spread them apart. If they stretch several centimeters, the mucus has become viscous, the pores in it have expanded to allow male reproductive cells to pass through. If the vagina is dry or the discharge is thin, there is no ovulation.
Important!
Protection against unwanted pregnancy by counting infertile days of the cycle is not always safe.
Inflammatory process
The presence of fluid not due to ovulation is associated with inflammation of the following organs:
- fallopian tube;
- ovaries;
- Bladder;
- uterine cavity.
The fluid will not be able to resolve on its own, so it can be observed during each ultrasound examination. To accurately determine the disease, the gynecologist will order additional tests (urine, blood); if they confirm inflammation, antibacterial drugs will be prescribed.
Treatment of the inflammatory process of the pelvic organs should begin immediately after examination by a doctor. At the initial stage of the disease, the doctor may prescribe one or several types of antibiotics. If such treatment is ineffective or for another reason why oral administration of drugs is impossible, the patient must be hospitalized. In the hospital, antibiotics are administered by injection or IV.
With such a disease, there is a need to treat the partner, since it is often the partner who becomes the carrier of the infection. Neglecting its treatment can provoke a recurrence of the disease.
Surgery involves opening the abscess or eliminating perforation. That is, the operation is prescribed for advanced cases when there is a large accumulation of pus in the tissues. This is necessary to eliminate the abscess before it ruptures and fills the abdominal cavity with pus. If abscesses form on the uterus or ovaries, removal of the affected organ may be prescribed.
Subuterine fluid during pregnancy
During an ultrasound of a woman during pregnancy, free fluid in the pelvis is diagnosed in very rare cases. But where does it come from? And is this dangerous for the health of the expectant mother and her baby? In women, fluid behind the uterus may appear due to natural causes, such as after ovulation or during menstruation. And also after surgical termination of pregnancy (abortion). It is clear that during a normal pregnancy this is impossible. Therefore, if an ultrasound reveals retrouterine fluid during pregnancy, this indicates that the expectant mother has a disease.
Possible diseases
We list the diseases that can cause fluid to form in the pelvis:
- chronic and acute inflammatory processes in the organs located in the pelvis lead to fluid gradually accumulating behind the uterus, most often this is diagnosed in the following diseases: ovarian apoplexy, endometriosis, pelvioperitonitis, hemoperitoneum, purulent salpingitis, ascites, peritonitis;
- bleeding in the abdominal cavity;
- cancer in the latent period, for example, neoplasms on the ovaries;
- liver diseases.
As you can see, free fluid during pregnancy is a symptom of many serious diseases. Naturally, all of the above conditions are potentially dangerous both for the health of the baby and for the health of the woman. In this regard, you need to understand that if an ultrasound during pregnancy revealed fluid in the pelvis, then the expectant mother should immediately contact her obstetrician-gynecologist. The doctor, having familiarized himself with the results of the study, will prescribe a general blood and urine test for the woman, and, after studying the data obtained, will prescribe appropriate treatment or refer her to another specialist.
Ectopic pregnancy
If the fertilized egg does not reach the uterine cavity, but is implanted into the wall of the tube, an ectopic pregnancy occurs. There is a need to take a hCG test and undergo another ultrasound examination (vaginal).
But statistics show that an ectopic pregnancy makes itself felt even before an ultrasound reveals free fluid in the retrouterine space. This is explained by the fact that the liquid appears after the pipe ruptures.
Apoplexy occurs if a vessel of the Graafian bladder, ovarian stroma, follicle cyst or corpus luteum ruptures and hemorrhage begins in the ovary. Its tissue is destroyed and hemorrhage continues in the abdominal cavity and in the retrouterine space.
When performing an ultrasound, fluid is observed in the retrouterine space. To be more precise, this liquid is blood, often with clots. The serous cover of the uterus is pink, the size is not increased. Chronic inflammation in the form of adhesions can be observed in the uterine tubes.
This disease can be caused by disorders in the tissues and vascular system of the ovary, which are caused by hyperemia, sclerotic or dilated vessels, inflammation, and small cystic deformation of the ovary. There will be heavy bleeding even with a small rupture (1 cm in diameter).
With apoplexy, the following symptoms are observed:
- pain in the lumbar region and lower abdomen;
- bloody discharge from the vagina, which stops along with the pain;
- general weakness;
- dizziness.
Reasons for the breakup:
- injury;
- sexual intercourse.
Apoplexy is an acute disease that requires urgent medical examination. If there is a suspicion of this disease, urgent hospitalization is indicated. Treatment is aimed at localizing bleeding, restoring ovarian tissue and stabilizing the condition after blood loss.
Cervical mucus analysis
Proper preparation before the test is important to get the right results the first time.
A week before the test, you should not change your usual lifestyle or diet. You cannot take new medications. It is prohibited to have sexual intercourse several days before taking the sample. On the day of testing, you must wash your external genitalia. The test is taken in the morning. It is necessary to calculate the phase of the menstrual cycle. The study can be completed within one week after the end of menstruation. At this time, the secretion has its original form, the maximum amount of sex hormones is produced for the production of cervical fluid.
The doctor takes a smear and sends it to the laboratory immediately, before the cells and substances in it are destroyed.
The following mucus parameters are determined in a smear from the cervical canal:
- volume of secretion;
- viscosity;
- time required for hardening;
- stretching of secretions between glass slides (carried out before examination under a microscope);
- cellular composition revealed in the field of view of a microscope.
The cervical number is the value that is added up after evaluating the above parameters. It can be low (0-7), medium (8-12) and high (13-15). The higher the indicator, the greater the possibility of conceiving a child.
If leukocytes are detected in the field of view of the microscope, then an infectious infection has occurred that requires therapy.
Important!
At the time of testing, there should be no inflammatory diseases of the genital organs or infection. Only then will the analysis show the true results.
Another laboratory test is the determination of antisperm antibodies in cervical mucus. These are immunoglobulins that are directed against antigens of male germ cells. They suppress the ability to conceive by destroying sperm and preventing them from passing through the canal.
Before the test, you must abstain from sexual intercourse for three days before the test. They take the test in the middle of the cycle (from 11 to 13 days) before the release of the corpus luteum.
To determine the amount of immunoglobulins of antisperm antibodies, the enzyme immunoassay method is used.
Acute purulent salpingitis
Acute purulent salpingitis is an acute inflammation of the pelvic organs. An ultrasound examination will show expansion, thickening, and elongation of the fallopian tubes, which are characterized by a decrease in echogenicity. There is an accumulation of free fluid in the rectal uterine cavity.
Symptoms of the disease:
- abdominal pain;
- sensitivity during cervical movement;
- elevated temperature;
- leukocytes more than 10500;
- the presence of pus during puncture of the posterior fornix;
- ESR >15 mm/h.
Treatment of salpingitis is carried out in 3 stages:
- Preparing for surgery.
- Removal of purulent fluid and treatment of the lesion.
- Rehabilitation after surgery.
Before surgery, acute manifestations of inflammation are stopped, the aggression of microbial pathogens is suppressed, and metabolic disorders are corrected.
For more effective treatment, if discomfort, pain or symptoms of the disease appear, you should not delay or try to treat yourself using traditional medicine or, especially, prescribe yourself medications. Once every six months you need to visit a gynecologist and, if necessary, undergo an ultrasound. The initial stage of almost any disease is treatable, so do not neglect your health.
Fluid detected on an ultrasound in the retrouterine space may be a completely harmless phenomenon or, conversely, indicate the presence of certain diseases.
But how to determine how dangerous this symptom is and when urgent treatment is needed? First of all, it should be said that if a few milliliters of fluid are detected during a pelvic ultrasound 14-15 days after the start of the cycle, then nothing bad happens.
At this time, the woman’s body has just undergone ovulation - the process when an egg is released into the abdominal cavity from the ovary after the rupture of a mature follicle filled with fluid.
It is precisely this fluid that can temporarily accumulate in the retrouterine space. After a few days, this fluid will resorb or resolve. The appearance of fluid in other cases indicates the need for a more thorough examination of the condition of nearby organs.
How many days does conception occur after intercourse?
Before meeting the sperm, the egg begins its journey to the uterus in the fallopian tube at a certain speed. After fertilization, this speed does not increase; the future embryo moves towards the uterus in the same way as before fertilization.
The entire woman’s body contributes to the entry of the fertilized egg into the uterus; the fallopian tube plays a crucial role here:
- The muscles of the fallopian tube begin to move, contracting towards the uterus;
- The fluid in the fallopian tube begins to move towards the uterus, carrying the egg in its flow;
- The muscle connecting the fallopian tube and the uterus relaxes, allowing the fertilized egg to enter the uterus.
All these actions occur under the influence of the hormones estrogen and progesterone, which, with the fertilization of the egg, begin to be produced in the ovaries with a vengeance.
The process of moving the embryo into the uterus takes about 4 days, and another 2 days for the process of implantation into the wall of the uterus. In general, these processes take 6-7 days. So the answer to the question: “How long does it take for conception to occur?” sounds like this: “About a week.”
What does an ultrasound show?
If we talk about the structure of the female body, the uterus is a pear-shaped cavity. The main task of this organ is to bear and protect the fetus throughout the entire pregnancy.
The postuterine space, or as it is also called in medicine, the space of Douglas, surrounds the uterus and is limited by the layers of the peritoneum and the anterior surface of the rectum. Usually, when liquid appears there, it accumulates in the lower part of the space in a small depression.
The transducer used to perform ultrasound is a microphone that can detect high-frequency sound waves, somewhat similar to a submarine's echo sounder. These waves are inaccessible to the human ear. Ultrasound not only sends high-frequency waves into the body, but also tracks how the wave reflects off the tissues and organs inside each of us. The received data is displayed on the monitor in the form of a picture.
The intensity of reflection depends on the density of tissue, its structure, as well as many other indicators, and is determined through frequency, amplitude, signal travel time, and characteristics of the wave itself. If there is no fluid in the retrouterine space, then the cavity of this space itself will not be detected on ultrasound. Therefore, any experienced ultrasound specialist can always determine whether there is such a liquid or not.
It is difficult to find out in any other way than ultrasound about the presence of fluid in the pouch of Douglas. It is not surprising that many women are unaware of its existence before research.
Although this symptom may be decisive for more serious examinations and tests, which should not be postponed under any circumstances. After all, sometimes it is quite difficult to accurately determine what has accumulated in the cavity: inflammatory exudate, transudate, blood or something else.
Presence of bloody fluid
One of the pathologies is the presence of a large amount of bloody fluid. It comes from an ovary that has ruptured. In medicine, this disease is called. The disease develops with a follicular cyst, rupture of internal vessels, ovarian stroma or its cyst. After its destruction, the substance enters the peritoneum. Often the blood has small clots. All this is accompanied by:
- abundant secretion;
- weakness;
- headaches;
- discomfort in the lower back.
Blood often appears as a result of harsh sexual contact, injuries, excessive physical exertion, and deformation of the appendages.
Discharge during pregnancy
During ovulation
The approximate date can be calculated using your calendar:
- Determine the duration of the menstrual cycle.
- Divide this number by two.
- We count this number of days from the beginning of the last menstruation.
The resulting date will serve as the beginning of the fertile period.
Rarely does the ovulatory phase occur, which occurs precisely in the middle of the cycle. This is due to hormonal levels, physiological and psychological factors. For more accurate forecasting, it is necessary to measure basal temperature for several months and record the results. According to doctors, for most of their patients, favorable days occur from the 11th to the 21st day of the cycle.
To answer this question, it is necessary to find out the duration of ovulation. For everyone it is almost the same - approximately 48 hours. The mature egg remains viable for another day, so the characteristic discharge may still continue.
Cervical mucus, caused by a favorable time for conception, can last only a couple of days, and then gradually thickens due to an increase in progesterone content.
On a note! When vaginal fluid does not tell you anything about the beginning of the fertile phase, it is worth buying a special test that will show two stripes at the moment the egg leaves the ovary.
Vaginal discharge is not the only sign of the best time for fertilization. You also need to take into account the following signals:
- may pull in the lower abdomen;
- basal temperature increases (37.1–37.3°);
- strong sexual attraction to partner;
- minor pain and breast engorgement.
Signals of conception
The signs of pregnancy and egg release are very similar, so it is difficult to determine successful fertilization right away. Implantation bleeding causes pink and brown discharge to appear during ovulation, but it occurs after about a week and a half, when the fertilized egg attaches to the wall of the uterus.
Remember that liquid and watery secretions are practically excluded, because the reproductive system prepares safe conditions for the development of the fetus, and therefore the vaginal mucus becomes thicker.
No secretion
If you have no discharge, this does not at all indicate pathology or lack of ovulation. A large number of girls do not feel anything at the moment the egg leaves the ovary; they even experience vaginal dryness. Under such conditions, it is unlikely that conception will occur, but fertilization cannot be ruled out. After all, the lack of secretion may be due to low estrogen levels.
It is possible that instead of mucus, uncharacteristic creamy, smearing marks are observed on the panty liner. The reason most often lies in hormonal background, dietary habits and other external factors (strong experiences, stress).
There is no need to sound the alarm when you notice:
- copious (wet) secretion for only a few days;
- slightly yellowish or creamy marks on panty liners;
- bloody smear;
- watery, homogeneous discharge without lumps.
Women often describe white discharge during ovulation. However, it is worth considering that it is colorless mucus that indicates a favorable period for conception. When it comes to cloudy or white secretions, then most likely ovulation is behind you or the vaginal microflora is disturbed.
Remember that normal cervical fluid cannot be released against the background of unpleasant sensations, which most often indicate negative processes in the body.
Failure of the reproductive system cannot be ruled out if the discharge is accompanied by the following symptoms:
- Yellow with a green, gray tint (sexually transmitted infection).
- White curds with a sour smell, itching, burning (thrush).
- Heavy bleeding during ovulation - the pad gets wet in less than an hour (bleeding).
- Very liquid, have a foamy consistency (inflammation, infection).
- Dark brown, almost black (endometriosis).
They speak with confidence about a violation when the secretion is supplemented:
- unpleasant smell of fish, rot;
- clotted blood;
- pus and lumps;
- lasting more than two or three days;
- high body temperature;
- severe pain;
- systematic burning, redness and itching of the genitals.
Such symptoms should not be ignored, and visiting the hospital and getting tested is the key to the fastest possible recovery, and will also help to identify pathologies in time in the early stages of development.
Before ovulation
Before the fertile period, the concentration of estrogen in the female body increases, which increases the amount of vaginal secretion, making it liquid and mucus-like. Without this hormone, normal follicle formation in the ovary is impossible.
As the release of the egg approaches, or rather a few days before, the cervical fluid becomes viscous and sticky, continuing to grow in quantity. And unfavorable conditions remain for the movement of male cells, since the woman’s reproductive system is not yet ready for fertilization.
Secretion associated with the pre-ovulatory period begins differently in all women. Some do not have cervical mucus, while others report a thin and heavy vaginal discharge. Both options are considered normal.
Signs of deviations:
- a clot of pus, blood;
- foamy or curdled consistency;
- itching, burning and swelling of the labia
- sharp pain in the lower abdomen;
- watery yellow, green secretion.
With blood
Bloody or brown discharge before ovulation is considered dangerous. They are no longer associated with menstruation and are not yet caused by rupture of the follicular sac.
The exceptions are women who take OCs and use an intrauterine device.
The color is influenced by the type of pathology: from pale pink, red, to brown, brown and even black. If we describe the consistency, we observe:
- daub;
- slime;
- egg white;
- some water.
Vaginal secretions help a woman determine ovulation, but this is not the most accurate method of calculation. If pregnancy is undesirable, it is better to use special tests or monitor your basal temperature for 2–3 months.
After ovulation
To understand what discharge should be after ovulation, it is necessary to determine the current state of the body. The nature of vaginal secretion always changes after ovulation, but supplemented by other signs, indicates the beginning of the gestation period or a health problem.
If conception is not accomplished, then spotting after favorable days cannot be considered normal. The second half of the menstrual cycle in this case has its own characteristics:
- predominance of progesterone in the body;
- first a sticky or sticky state of the cervical fluid;
- increased thickness of mucous secretion;
- transparency is replaced by a white, beige shade of discharge;
- gradual decrease in secretion volume.
While the woman did not make plans to become a mother, she is confident and knows the date of her menstruation. The fertilized egg is no longer released, sending instead whitish mucus, similar to ovulation fluid. This is explained by the active production of hormones. The same situation occurs after sexual intercourse, after some time after which active fluid secretion can be observed.
Lower back pain
White discharge: what does it indicate?
Ovarian cycle
During ovulation, a small sac containing fluid and an egg, called a follicle, bursts in the ovary. If 2 or more rupture, then in this menstrual cycle the chances of a multiple pregnancy increase.
An egg is released from the follicle and begins its journey to the uterus. At the site of the rupture in the ovary, the corpus luteum, or corpus luteum, develops from cells called granulosa cells. It is a hormone-producing organ that releases progesterone into the blood, which throughout the second phase of the cycle prepares the body for pregnancy.
It is worth understanding that there should be a minimal amount of blood, this bleeding cannot last more than 2-3 hours, otherwise you should look for another reason and consult a doctor, especially if you are worried about pain in the lower abdomen.
If fertilization occurs, the corpus luteum turns into the corpus luteum of pregnancy and in this form produces a large amount of progesterone, so many people note a white thick discharge after conception, which is stimulated by a very high level of this hormone throughout pregnancy. If fertilization does not occur, the corpus luteum undergoes reverse development, and a small scar remains in its place.
Uterine cycle
Changes occur in the uterus that prepare it for the introduction of new life. Nutrients for the future embryo accumulate in the endometrium and blood supply improves. The phases of proliferation and secretion occur.
Cervical cycle
Few people know, but such a concept exists. The cervix undergoes changes every month. In the follicular phase, the first 14 days of a 28-day cycle, the volume of mucus that is secreted by the glands of the cervix, stimulated by the hormone estrogen, increases. By the middle of the cycle there is a maximum amount of it and it becomes liquid, changing its physical and chemical properties.
But the method has disadvantages: it cannot be used by women with unstable hormonal levels, with cycle disruptions and diseases in which there is a change in vaginal discharge, and in which creamy discharge after ovulation can be observed on any day of the cycle.
Vaginal cycle
They don’t even know about his existence, but he exists. The changes are especially noticeable in the upper third of the vagina. By the middle of the cycle, the epithelium grows, becomes more vascularized, loosens, and the vaginal glands synthesize more creamy mucus. In the luteal phase, all these phenomena disappear.
The cause of white discharge may be thrush. During pregnancy, the body reduces immunity so that the embryo can attach and develop. This prevents the mother’s body from rejecting it, because it contains 50% of foreign genetic material. With such physiological immunodeficiency, candidiasis develops.
It can only manifest itself as weak leucorrhoea, which a woman will not regard as a disease. The white, thin discharge may be copious cervical mucus, a watery vaginal secretion that forms in response to hormonal stimulation by progesterone. In combination with other signs, this increases the chances of seeing the coveted two stripes soon.
Lower back pain
Rising progesterone leads to a relaxed state of all muscle groups and ligaments, which causes pain during exercise, and sometimes at rest. If you experience white discharge after ovulation, this means you are pregnant, wait until the first day of your delay and take a hCG test.
There is an unusual emotional state with constant mood swings.
These symptoms are very similar to premenstrual syndrome. But if your PMS is usually not accompanied by these signs, then it’s worth taking a pregnancy test after a while.
Some women notice a tingling sensation in the abdomen and think that this is how the egg implants in the uterus. But it’s worth remembering the size of the egg; the body cannot detect implantation, but it responds well to increasing stimulation with progesterone. And in the small pelvis there are also muscles and ligaments, the relaxation of which causes tingling and soreness. When, after ovulation, the stomach hurts like before menstruation and white discharge occurs for several days, pregnancy is suspected
Many women, when they learned about their situation, noted that after ovulation they had unusual, very profuse leucorrhoea, similar to cream. But this symptom is not observed in everyone.
Until now, doctors cannot give an exact answer why this happens. Maybe this is hyperstimulation of the endocrine glands with progesterone, as a result of which they secrete a lot of mucus. Or maybe changes in the uterine mucosa occur earlier than an increase in pregnancy hormones can be detected.
For most women, the period called postovulation is when yellowish marks are visible on the underwear. Here it is important to understand what shade they have. Light-colored spots are the norm, which cannot be said about dark yellow marks, which signal a possible disease, in particular if, along with the discharge, an unpleasant odor, pain, increased body temperature, and itching appear.
The most common is white discharge. In order to figure out whether they are normal or not, you should correctly characterize the observed cervical fluid.
- A translucent, or even completely white, color of the discharge indicates normality if it is visually similar to egg white, the duration of which is no more than seven days;
- White discharge, along with itching and an unpleasant odor, indicate that you should immediately consult a doctor who will take a smear for analysis. Often this phenomenon indicates the presence of some kind of disorder in the body. Properly selected hygiene products, a properly formulated diet and medications will correct the situation;
- The release of mucus that has a grayish-green color indicates the presence of an inflammatory process in the uterine cavity. This disorder is accompanied by copious discharge of fluid with a sour odor. Symptoms in the form of itching and burning indicate an urgent visit to the gynecologist;
- A more serious situation occurs if the outflow of cervical fluid is accompanied by severe itching. This indicates the neglect of the inflammatory process as the cause that led to the formation of cracks in the walls of the mucosa. At the same time, the walls of the genital organs swell and turn red, which indicates the need for immediate medical attention;
For example, discharge 7 days after the ovulatory phase, on the eve of menstruation and after it is more abundant. Vaginal secretions are of great diagnostic importance in gynecological practice and indicate pathological processes occurring in the female body.
Vaginal secretions can have a certain diagnostic role, for example, indicate the fertilization of an egg by a sperm, that is, the beginning of pregnancy.
If conception has occurred, the discharge is clear and liquid in consistency, has no odor and does not cause discomfort to the woman.
This is exactly what the discharge should be like after fertilization, but there may be other options, which will be covered below.
If there is no discharge after ovulation, then this phenomenon is normal, but if there was discharge before ovulation, you should consult a doctor. This symptom may indicate a violation of hormonal processes, nervous tension, inflammatory diseases of the female reproductive system.
Ovulation process
What does the color say?
Discharge after ovulation on different days of the menstrual cycle has distinctive features and may even indicate conception that has occurred in the female body.
When a fertilized egg implants into the uterine wall, pinkish, brown and red marks may appear on the pad. The intensity of coloring of such discharge will depend on the number of blood streaks in the vaginal secretion.
Leucorrhoea, in which there is no microbial flora and leukocytes, is observed in virgins and women who are not sexually active. Also, white creamy discharge after ovulation is found in healthy women and contains a small amount of non-pathogenic microflora.
White, thick, creamy discharge can be one of the first signs of pregnancy and subsequently turns pinkish. Thick discharge acquires this consistency due to increased production of progesterone and occurs a week after ovulation.
White cheesy discharge is one of the main signs of vaginal candidiasis, the diagnosis of which requires confirmation by a doctor.
Brown
Brownish discharge after ovulation and before the onset of menstruation appears during implantation of the embryo into the uterine mucosa and may be accompanied by pain in the lower abdomen. In addition, such discharge occurs during erosive processes on the cervix and requires consultation with a specialist.
Yellow
Yellow discharge occurs with purulent inflammatory diseases that are sexually transmitted. For example, with gonorrhea, chlamydia, trichomoniasis. In addition, yellow discharge occurs after the ovulatory phase due to the predominance of the hormone progesterone.
Active secretion of cervical fluid
During the period when the egg is preparing to be released, mucus begins to come out of the cervix in large quantities, which is a normal process. Such secretions are viscous, transparent and in some ways similar to the mucus that makes up the prenatal plug, but their quantity is much less.
Abundant discharge after ovulation of a dark yellow hue, accompanied by a stench and pain in the lower abdomen, directly indicates an inflammatory process localized in the uterus or vagina. In this case, there is a possibility of a rupture of the fallopian tube, which is fraught with dangerous consequences. It’s better not to delay this and immediately see a specialist.
The norm is the secretion of mucus, which consists of dead microbial cells and epithelial tissue, a secretion produced by the Bartholin glands of the vagina. A healthy woman may notice a whitish discharge without a characteristic odor. Otherwise, if unhealthy signs appear in the form of burning, itching or pain, you should seek medical help.
Female discharge during the postovulation phase serves as a sign of health or illness. The question of what kind of female discharge occurs after ovulation is also of concern in order to determine the favorable phase for conception. Also, the specificity of the secreted fluid can show whether the expected conception has occurred or not.
If copious discharge persists during the postovulatory period, then it is necessary to monitor the amount of mucus, its smell and itching, if any. If the mucous fluid is greenish, gray, white or bloody in color, this indicates various diseases and pathologies.
Normal vaginal discharge during the post-ovulation period can be of different shades, consistency, and smell. Normal discharge is considered:
- White, almost transparent. The presence of pinkish bloody streaks is allowed.
- A thick, cloudy secretion that gradually acquires a yellowish tint.
- Brownish-beige, appearing within 5 - 7 days upon the onset of ovulation.
Copious discharge after ovulation is odorless, does not cause irritation on the skin of the external genital organs and does not cause discomfort. Their intensity depends on the phase of the menstrual type, as well as on the individual characteristics of the woman.