Among all benign types of mammary gland pathology, the fibroglandular form of mastopathy is the most dangerous in terms of precancerous changes, especially in women over 50 years of age and with pronounced cell proliferation. The main causative factor of the disease is dishormonal disorders, typical symptoms indicate a diffuse form of pathology, and treatment is aimed at restoring endocrine balance. The health prognosis for mastopathy with a predominance of the glandular component is quite favorable, subject to regular medical supervision and preventive therapy.
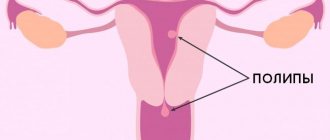
Classification of endometrial polyps, causes of occurrence
The endometrium consists of glandular, connective (fibrous) tissues and blood vessels. The percentage of these tissues in the endometrial polyp will determine the type of its structure and the method of treatment. The vast majority of formations are glandular-fibrous and benign in structure.
Based on their histological structure, endometrial polyps are divided into the following types:
- Ferrous:
- glandular
- glandular-cystic
- adenomatous (precancerous)
- Glandular fibrous (mixed)
- Fibrous
- Placental
At the beginning of the menstrual cycle, under the influence of sex hormones, the glandular cells of the uterine mucosa rapidly divide - the endometrium grows. At the end of the cycle, the overgrown layer is rejected and released from the uterus in the form of menstrual bleeding. This process is regulated at the cellular level and depends on many factors, including the level of sex hormones.
Glandular polyps of the endometrium are observed in women with preserved menstruation and practically never occur in postmenopause, because the glandular tissue atrophies with low levels of sex hormones. For the same reason, endometrial fibrous polyps are observed mainly in postmenopause.
A long-term, sluggish inflammatory process (chronic endometritis) stimulates the synthesis of connective tissue in the uterine mucosa. Gradually, the glandular tissue is replaced by connective tissue - fibrosis develops, and the processes of endometrial rejection are disrupted. The area of the mucous membrane that is not rejected grows with blood vessels - a glandular-fibrous endometrial polyp .
A placental polyp is always formed from fragments of the fertilized egg remaining in the uterus after childbirth or abortion. Over time, it degenerates into fibrous.
Back to contents
Reasons for appearance
A polyp in the uterus can appear for various reasons. The occurrence of the disease is influenced by a group of factors. Main causes of the disease:
- hormonal disorders;
- vascular pathology;
- inflammation in the reproductive system;
- thyroid diseases;
- abortions;
- concomitant chronic diseases;
- excess weight;
- sedentary lifestyle.
Diseases of the blood vessels located near the uterus can cause the appearance of polyps. If blood circulation is disrupted, the cells do not receive the necessary nutrition. This stimulates their uncontrolled growth. As a result of the proliferation of the epithelium, formations appear.
Inflammatory diseases are a risk factor for the development of polyposis. During illness, the body actively produces substances whose purpose is to stop the inflammatory process. At the same time, the number of cells in the endometrial layer increases. And this is the material for the construction of potential formations.
When the thyroid gland is not functioning properly, it affects the body's production of hormones. An imbalance occurs, as a result, sex hormones begin to be released in excess, which provokes polyposis.
Medical and medical abortions are traumatic for a woman’s reproductive system. The situation becomes even more complicated if, after termination of pregnancy, curettage of the uterine cavity was performed. Initially, such rough manipulations lead to the formation of areas of erosion, and over time, cysts or polyps form.
Women suffering from chronic diseases that affect metabolism and blood circulation are more likely to experience the appearance of growths in the uterus. Against the background of diabetes or hypertension, blood circulation in small vessels is impaired, which affects the quality of tissue nutrition and the growth of the epithelial layer.
Excess kilograms are an additional source for the formation of estrogen hormones. Their increased content is the basis for the formation of benign neoplasms.
A sedentary lifestyle also negatively affects the functioning of the reproductive system. Blood stagnation occurs in the pelvic organs, which leads to disruption of the formation of new cells and disposal of waste cells.
Genetic predisposition can affect the development of polyps in the uterine cavity. If a woman has been treated with drugs that block the perception of sex hormones, neoplasms may also appear inside the organ.
Symptoms of uterine polyp
- Changes in the nature of menstruation:
The listed symptoms are not specific and are characteristic of other gynecological diseases.
The presence and severity of symptoms depends on the size of the polyp, its structure, location in the uterine cavity and concomitant gynecological pathology.
Patients with endometrial polyps may have no complaints and clinical symptoms. Often the formation becomes an accidental finding on a preventive ultrasound of the pelvic organs.
Back to contents
What symptoms can be used to suspect pathology?
When an endometrial polyp is suspected, symptoms vary in severity. Sometimes an asymptomatic course is possible when the size of the lesion is small, up to 1 cm.
The leading signs of endometrial pathology are uterine bleeding of several types:
- acyclic, which appear regardless of the phase of the monthly cycle;
- contact are observed after sex or examination by a gynecologist;
- menometrorrhagia - heavy menstrual flow.
Cramping pain in the lower abdomen can appear with large growths, torsion of the legs and tissue necrosis.
During reproductive age, the causes and symptoms of overgrowth often cause primary infertility. The lack of ovulation, which accompanies most women with this pathology, is a consequence of hormonal imbalance. This means that it is impossible to say for sure whether it is possible to become pregnant without treatment. If a neoplasm forms against the background of an unchanged endometrium, then pregnancy can occur, but the risk of spontaneous termination is increased.
Important!
Women with a normal menstrual cycle may develop a functional polyp. It is formed in the second half of the MC and is capable of cyclical changes, like the rest of the endometrial layer. Such growths respond to the introduction of estrogens and progesterone.
Diagnosis of polyps of the uterine cavity
A gynecological examination on a chair is informative only when the formation is large and extends from the uterine cavity into the vagina.
The diagnostic standard is transvaginal ultrasound of the pelvic organs and diagnostic hysteroscopy.
Ultrasonography
Transvaginal ultrasound of the pelvic organs on days 6-7 of the menstrual cycle can identify dense fibrous and glandular-fibrous endometrial polyps.
Glandular polyps are similar in structure to normal endometrium, have a soft consistency, are compressed by the walls of the uterus and are not distinguishable when small in size.
If there are symptoms and no signs of endometrial pathology on ultrasound, it is recommended to conduct a repeat ultrasound examination on days 12-14 of the menstrual cycle, by which time the glandular polyp will have grown, increased in size and become visible on ultrasound.
A more informative ultrasound examination is echohysterosalpingoscopy (ECGS), an ultrasound examination with contrast of the uterine cavity. The uterine cavity is filled with saline, it expands, the polyp takes its natural shape and is contoured against the background of a contrast liquid.
Ultrasound conclusion: suspicion of focal endometrial hyperplasia is an indication for hysteroscopy.
Hysteroscopy
First, diagnostic hysteroscopy is performed - an endoscopic examination of the uterine cavity. Diagnostic hysteroscopy allows you to visually confirm or exclude a uterine polyp.
Video selection of hysteroscopic examinations
If an endometrial polyp is detected during hysteroscopy, it is removed - hysteroresectoscopy. If hysteroscopy does not confirm a uterine polyp, a targeted biopsy of the endometrium is performed in the location described in the ultrasound protocol.
Ultrasound and hysteroscopic findings are not a diagnosis. The final diagnosis is made only after removal of the formation and clarification of its histological structure.
Back to contents
Treatment of fibroglandular polyp of the endocervix
Treatment of fibroglandular lesions involves its mandatory removal. The operation is planned. Before treatment, a course of drug therapy is carried out, especially in the presence of inflammatory processes.
Indications for surgical removal are:
- Large growths of the mucous membrane (can cause blockage of the cervical lumen and interfere with pregnancy);
- Woman’s age over 35 years (risks of multiple polyps and polyposis);
- Ineffectiveness of drug treatment, including hormone replacement therapy;
- Infertility of a woman caused by pathological tissue proliferation;
- Risks of malignancy.
Considering the planned nature of the removal, the woman has the opportunity to carefully prepare, and the doctor has the opportunity to formulate the correct removal tactics and choice of method.
Main types of surgery
The following manipulations are effective against polyps:
- Laser coagulation. The method involves removing the polyp by excision of the stalk and evaporation of the pathological tissue under the influence of a laser beam. During the operation, simultaneous soldering of the vessels occurs, which prevents the development of bleeding. The disadvantage of this method is the presence of heavy smoke during surgery and the inability to remove large or multiple polyps.
- Polypectomy. Removal of a pathological growth by excision or twisting from the walls of the cervix. The method is effective for polyps up to 2.5-3 cm. After removal, the wound surface of the bed is cauterized with electrodes or a laser.
- Diathermoexcision. Loop removal, which involves placing a loop on the growth and excision it, followed by cauterization with electric current. It is used for severe dysplasia of the walls of the cervical lumen, as well as for the risk of adhesions and erosive lesions.
- Cryodestruction. The method involves freezing the stalk or body of the polyp using liquid nitrogen. After freezing, the polyp is removed. The main advantage is low trauma and rapid recovery. After manipulation there is no risk of scar tissue formation.
- Radio wave coagulation. Removal is carried out using special equipment - the Surgitron apparatus. It is characterized by minimally invasiveness, low trauma and speed of execution.
- Resection. Abdominal surgery, which involves removing part of the uterine cavity or the entire organ. A radical decision is made when the tumor becomes malignant in order to avoid metastasis to other parts of the pelvic organs.
The type of intervention is selected based on the size and symptomatic picture of the polyposis lesion, as well as on the basis of the characteristics of the woman’s medical history.
Possible complications
Despite the small volume of most removal methods, the risk of complications still remains. The main complication of the operation is the emergence of new lesions. In almost 12% of all clinical cases, relapse occurs.
Other complications include:
- Formation of adhesions and scar tissue;
- Infectious lesion;
- Malignancy of an incompletely removed polyp;
- Bleeding when the canal walls are damaged;
- Allergic reactions, severe swelling;
- Hematometra is severe internal bleeding followed by stagnation of blood in the uterine cavity.
Drug therapy after removal
Considering that the uterus, ovaries, appendages, and cervical canal are hormone-dependent organs, it is important to restore the hormonal levels of the female body. After surgery, there may be an imbalance of progesterone and estrogen, which can lead to unpleasant consequences
After removal of the polyp, the following medications are prescribed:
- Hormonal drugs (Utrozhestan, Duphaston, Tri-Mercy);
- Antibacterial drugs (Diclofenac, Piroxicam, Celecoxib, Cifran-OD);
- Douching with antiseptics (Miramistin, Chlorhexidine, Furacilin).
After removal, women are shown a protective regime, sexual rest and strict adherence to the regimen of taking certain medications. After surgery, you should undergo an ultrasound scan at least 2 times a year, take blood tests, and treat infectious diseases in a timely manner.
The prognosis for timely removal of fibroglandular polyps is favorable. When atypical cells are detected by histology, prognostic criteria are determined by the extent of the oncogenic process.
You can make an appointment with a doctor directly on our website.
Be healthy and happy!
Treatment of endometrial polyps
The first stage of treatment is removal of the polyp under visual control - hysteroresectoscopy.
This is the only way to remove the polyp completely and avoid relapse. All removed formations and biopsies are subject to histological examination to determine the type of structure. The second stage is treatment in accordance with the histological conclusion.
Endometrial polyps, as you now know, have different histological structures, and the treatment that helped your friend may not be effective in your case!
Glandular polyps of the endometrium are treated with hormonal and antihormonal drugs, epigenetic therapy is additionally prescribed, and the menstrual cycle is corrected.
For fibrous, glandular-fibrous and placental hormones are not effective, anti-inflammatory treatment, immunocorrection, and physiotherapy are carried out.
The effectiveness of treatment is monitored after 3 months, ultrasound examination and diagnostic hysteroscopy with endometrial biopsy are performed. For 2 years, patients are under clinical observation and undergo ultrasound examination of the pelvic organs every 6 months.
Back to contents
Treatment of glandular polyps after removal
Is drug treatment (hormonal, anti-inflammatory, complex) necessary after surgical removal of a true glandular polyp? This issue remains controversial to this day.
Most researchers insist that if the intrauterine polyp is completely removed, if selective ablation of the underlying basal layer of the endometrium is done and the woman does not have any other (except for the removed polyp) gynecological pathology, she does not need additional treatment. The patient is recommended to have a healthy lifestyle and follow-up with a gynecologist with ultrasound control at least once every 6 months.
Other authors are not so optimistic - they believe that after removal of a glandular polyp it is advisable to carry out hormonal therapy.
If the patient, along with the endometrial polyp, has other gynecological diseases, then the polyp is removed and the latter are treated.
The choice of optimal therapy in each individual case is individual. It depends on the patient’s age, on the presence of concomitant gynecological, endocrine-metabolic, and other diseases, and on the woman’s individual reproductive plan. The management tactics for a patient with an endometrial polyp are determined based on the results of histological diagnosis.
Treatment options for endometrial glandular polyp after removal
| Histological diagnosis | Reproductive age | Age over 48 years |
| Glandular polyp against the background of typical endometrial hyperplasia | Monophasic COCs: Logest, Mercilon, Novinet, Lindinet-20, Microgynon, Rigevidon, Janine... The course of treatment is 3-6 months. Progestins: Duphaston 20 mg per day from 16 to 25 days of the cycle. Utrozhestan 200 mg per day from 16 to 21 days of the cycle. 17a-OPK intramuscularly 250 mg on the 14th and 21st days of the cycle. Course of treatment 6 months | Continuous gestagens: Depo-Provera 150 mg once a week. 17a-OPK 250 mg 2 times a week The course of treatment is 6-9 months. GnRH agonists: Buserelin or Zoladex in standard dosage. The course of treatment is up to 6 months. |
| Glandular polyp against the background of atypical endometrial hyperplasia or with focal adenomatosis | Atypical endometrial hyperplasia is treated: read here | Atypical endometrial hyperplasia is treated |
Can a glandular polyp reappear after it is removed? Yes! In case of relapse of the disease, more aggressive methods of treating the polyp are chosen:
- Medical menopause (during reproductive age) – treatment with GnRH agonists.
- Electrosurgical ablation of the endometrium has recently been used less frequently.
- Hysterectomy.
Possible complications of the disease
Why should even asymptomatic glandular polyps be removed? Because without treatment, the following dangerous conditions can develop against the background of a polyp:
- Uterine bleeding.
- Secondary anemia.
- Infertility.
- Infection or necrosis of the polyp can lead to general intoxication and sepsis.
- Malignancy - the risk of malignancy of glandular polyps reaches 3%. If foci of adenomatosis appear in a polyp, then the probability of its degeneration into cancer increases to 40% or more.
When can you get pregnant after polyp removal? Read more: Endometrial polyp and pregnancy
Prognosis and possible complications
With timely treatment, the prognosis of the disease is favorable. In advanced cases, malignant transformation of tissue growth may occur. In addition, polyps tend to recur.
If polyps that appear in the cervix are not treated in a timely manner, a woman may develop complications such as:
- anemia due to constant bleeding from the vagina;
- degeneration of normal cells into atypical ones;
- growth of pathological growths and blockage of the cervical canal;
- uterine bleeding;
- threat of miscarriage during pregnancy.
Symptoms and diagnosis
The initial stage of endocervical polyp formation is characterized by an asymptomatic course. But during its growth, clinical signs appear such as:
- release of blood from the genital tract during or after sexual intercourse;
- spotting not associated with the menstrual cycle;
- white discharge of mucous consistency;
- pain and discomfort during sexual intercourse.
When the above symptoms appear, the woman undergoes additional examination to identify polyps in the cervix. Confirmation of the diagnosis is carried out after a mirror examination and colposcopy.
Inspection using mirrors makes it possible to detect large formations and those that protrude into the external uterine os. In addition to colposcopy, cervicoscopy is performed.
There are also indirect signs indicating the formation of a growth in the cervical region. They are detected during a gynecological examination. One of them is a dense and thickened cervix. In addition, the following signs indicate pathology:
- pain appears on palpation of the cervix;
- hypertrophy of the external pharynx;
- swelling of the cervical canal;
- detection of an elastic formation of a round shape.
Large polyps can be detected through ultrasound.
Main types of surgery
There are several methods for removing a polyp in the cervical canal area, and the choice of one of them is determined by the size of the tumor and its location:
- Surgical curettage.
- Hysteroscopy.
- Polypectomy.
- Cryodestruction.
- Radio wave loop polypectomy.
- Laser coagulation.
Cervical polyps
Benign neoplasms. Outgrowths from the columnar epithelium of the cervix are detected during a standard medical examination or ultrasound scanning. The following options are available:
- Glandular polyp of the cervical canal;
- Glandular-fibrous;
- Fibrous;
- Decidual (during pregnancy);
- Adenomatous.
The first four options are safe from an oncological point of view. Adenomatous polyp refers to a precancerous condition, in which it is necessary to quickly carry out all necessary therapeutic measures to prevent cervical cancer.