The possibility of pregnancy depends on the woman’s health, including reproductive health. Even the slightest deviation or disorder can cause infertility. There are many pathologies that interfere with successful conception, and, unfortunately, a woman is not always aware of the violations. The occurrence of a glandular endometrial polyp is important to identify and remove on time. Delay in therapy is fraught with unpredictable consequences.
What is an endometrial polyp?
Uterine lining
The endometrium is one of the three linings of the uterus. The outer membrane is called the perimetrium (or serosa). The middle, largest lining of the uterus, the myometrium, consists of smooth muscle cells (myocytes).
The lining of the uterus consists of three layers
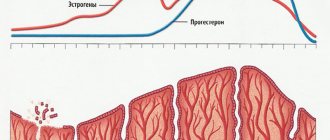
The inner lining is the endometrium. It is represented by two layers of cells: basal and functional. The cells of the basal layer have a small number of receptors for hormonal substances, due to which they are practically not susceptible to hormonal influences. The basal layer is the basis for the overlying functional layer.
The most superficial layer is functional, the cells of which are most sensitive to any hormonal changes in a woman’s body. It is rejected along with menstrual blood during menstruation, and after its end it is completely restored with the help of the basal layer.
How does growth occur?
A polyp is formed only from the mucous membrane of the uterus - the endometrium, as a result of hyperplastic processes. Due to intensive growth, the endometrium grows in height, forming a nodular neoplasm consisting of a stalk and a body.
As the growth forms, blood vessels begin to sprout, providing blood supply. Thus, its size can range from a few millimeters to 5–6 centimeters or more.
Types of polyps
Since the endometrium contains several types of cells, the neoplasm is formed with a predominance of one of them. Polyps are identified:
- adenomatous (glandular): growth with a predominance of glandular cells;
- fibrous: formation is formed by connective tissue cells;
- glandular-fibrous: the composition includes equally both connective tissue cells and glandular cells.
Features of a glandular polyp
The endometrial glandular polyp is largely represented by glandular cells, and to a lesser extent by stromal cells.
Depending on the layer from which it was formed, two types are distinguished:
| Type of polyp | Description |
| Basal (true) | It is formed from the endometrial layer of the same name. Unlike the second type, it is practically immune to sex hormones and does not change its structure |
| Functional (pseudopolyp) | It is formed from the most superficial - functional layer, which must be rejected during menstruation. However, if an area of unseparated endometrium persists for some reason, a growth forms on it |
The functional growth is highly sensitive to any hormonal changes, so its shape and structure can change along with the healthy endometrium throughout the menstrual cycle.
Based on histological type, pseudopolyps are divided into the following types:
- proliferative;
- hyperplastic;
- secretory.
Glandular neoplasms are extremely rare and are considered the most dangerous, as they are prone to malignant transformation, especially in postmenopausal women, against the background of neuroendocrine and metabolic disorders.
The risk of degeneration into a malignant form increases in proportion to size. With a size of 1.5 cm, the probability of transformation is 2%, 1.5–2 cm – 2–10%, more than 2 cm – malignancy occurs in more than 10% of cases.
The number of polyps in the uterus may also indirectly indicate the risk of transformation. Thus, single neoplasms rarely malignize (1–2%), multiple ones more often (20%), diffuse (familial) malignancy very often (80–100%).
Is deletion necessary?
The patient herself can choose the treatment method after consultation with a gynecologist. But you need to be well aware that the polyp cannot disappear. There are no folk remedies that will help get rid of it without surgery. The need for surgical treatment is due to the nature of the pathology - tissue proliferation.
If the form of uterine disease is of a type with a high risk of degeneration, the doctor will recommend a surgical treatment method. Most often this is done for fibrous and adenomatous types of polyps. The size of the endometrial pathology also influences the preference for surgical treatment.
Mandatory removal of tumors is recommended for women of premenopausal age.
Surgery is recommended for young patients if the growth causes severe bleeding from the uterus or causes infertility.
Reasons for the development of pathology
The reasons for the formation of a functional and basal polyp are somewhat different.
The development of endometrial polyp of functional and basal type has different reasons
Functional form
Since the functional layer is most susceptible to hormonal changes, formations of the functional type increase against the background of hormonal disorders, namely with hyperestrogenism.
The causes of dishormonal conditions can be:
- frequent stress;
- obesity, hypertension;
- diabetes mellitus, thyroid disease and other neuroendocrine pathologies;
- hyperestrogenism arising from inadequate therapy with estrogen-containing drugs;
- injuries and inflammatory processes of the uterine mucosa (endometritis);
- some other gynecological diseases.
Basal form
The basal layer is practically not subject to hormonal influences, therefore dishormonal conditions do not play a key role in the development of a basal type endometrial polyp.
A common cause of occurrence is injury to this layer and some other pathologies:
- abortion;
- fractional diagnostic curettage;
- prolonged presence of the intrauterine device in the uterine cavity, its incorrect installation;
- conducting a biopsy of the internal walls of the uterus without high-quality sterilization of instruments, inaccurate implementation;
- diseases of the immune system: allergies, autoimmune pathologies, especially those involving the vascular wall, immunodeficiency states;
- inflammatory processes in the uterus caused by sexually transmitted infections and some other pathogens;
- complicated obstetric history (miscarriages, termination of pregnancy, complicated childbirth).
Contraindications
Image courtesy of imagerymajestic on FreeDigitalPhotos.net
Considering the planned nature of curettage, it is possible to conduct high-quality diagnostics and exclude possible contraindications.
The operation is not performed for the following conditions and diseases:
- acute inflammatory diseases of the respiratory tract, gastrointestinal tract, genitourinary system;
- heat;
- severe pathologies of the heart, kidneys, liver;
- exacerbation of chronic diseases;
- lactation;
- postoperative period for other conditions;
- acute allergic reactions to anesthesia;
- severe mental disorders.
The doctor selects a method for removing uterine polyps based on multiple criteria. Contraindications are relative. If necessary, surgery is performed to stabilize the woman’s condition.
Symptoms
The beginning of the formation of a neoplasm almost always goes unnoticed, since during this period the woman does not observe any symptoms, and ultrasound methods cannot visualize it.
One of the symptoms of the pathology is nagging pain in the lower abdomen
Reaching a certain size, a polyp can provoke the following symptoms:
- intense pain before and during menstruation;
- the appearance of bloody discharge long before the onset of menstruation (intermenstrual bleeding). A woman can detect spotting on her underwear on any day of the menstrual cycle: at the beginning, in the middle or just before menstruation;
- delay of menstruation followed by copious discharge of menstrual blood;
- pulling pain in the lower abdomen;
- dyspareunia (pain during sexual intercourse);
- spotting after sexual intercourse, physical activity, stress;
- lack of a regular menstrual cycle.
Menopausal women may experience bleeding from the genital tract. At this age, this is a formidable sign, which often indicates oncological processes in the gynecological area.
Symptoms
Often the polyp does not manifest itself in any way, and the woman does not even suspect its presence. As a rule, the disease is diagnosed accidentally (during ultrasound examination). But specific symptoms may also appear. It is worth paying attention to heavy periods, as well as any bleeding in the middle of the cycle. Irregularity of menstruation is another symptom of the disease. If the polyp is large (more than 2 cm), then specific pain sensations are possible. It is also common for a woman to experience unpleasant feelings during sex. If bleeding occurs after menopause, a specialist may suspect the presence of neoplasms.
Endometrial polyposis and pregnancy are also associated. As a rule, a woman cannot conceive a child with this diagnosis. The polyp in the body behaves like an intrauterine device, that is, it does not allow the fertilized egg to attach itself to the organ cavity. It can also block the fallopian tube, preventing sperm from entering.
Diagnostics
If at least one of the symptoms appears, you should immediately contact a gynecologist. Based on complaints, anamnesis, results of a bimanual gynecological examination and speculum examination, the doctor will be able to suspect this pathology.
Laboratory research methods
To make a diagnosis, the doctor prescribes a hormonal study: determining the amount of estrogens, progesterones, follicle-stimulating hormone, luteinizing hormone, thyroid hormones, adrenal glands and others. The material is collected on different days of the cycle.
Additionally, tumor markers can be studied, especially in menopausal and postmenopausal women.
Instrumental research methods
Instrumental research methods are mandatory; they allow you to visualize the neoplasm, perform a biopsy with further examination of the tissue for benignity or malignancy.
Pathology is often detected during ultrasound
The following types of instrumental studies are used:
- Ultrasound examination of the pelvic organs (ultrasound). The method allows you to assess the condition of the endometrium, the presence of hyperplastic processes and neoplasms in it;
- endoscopic examination using a hysteroscope (hysteroscopy). A hysteroscope is a special optical device that is inserted into the uterine cavity and allows you to examine its mucous membrane in detail.
During hysteroscopy, it is possible to perform a targeted biopsy of the tumor for its subsequent cytological and histological examination.
Another option is fractional diagnostic curettage. Tissue fragments isolated during the procedure are also sent to the laboratory to evaluate the cellular and tissue composition.
Cytological and histological studies are necessary to assess the degree of cell differentiation, the presence or absence of their malignancy and to determine further tactics for managing the patient.
Medical examination plan
A standard examination of a woman in a gynecological chair often turns out to be uninformative. A doctor cannot confirm a pathology based solely on its external manifestations. Basic screening includes the following instrumental diagnostic methods:
- Ultrasound (the information content of the study is about 98%).
- Study of uterine cavity aspirate (used to exclude the malignant nature of the neoplasm).
- Hysteroscopy (helps assess the location and size of the polyp).
- Diagnostic curettage (allows you to determine the type of tumor).
Based on the results of the examination, the gynecologist makes recommendations for therapy.
Therapy
Most often, a glandular polyp is treated surgically.
During the operation, the gynecologist inserts a hysteroscope into the uterine cavity, after a growth is visualized in the field against the background of pathologically unchanged endometrium, it is precisely removed mechanically or using laser ablation, electrocoagulation, etc.
Polyp removal is usually performed during hysteroscopy
If fractional diagnostic curettage was performed at the diagnostic stage and the polyp turned out to be functional, further surgical intervention is not required.
In postmenopausal women, especially with frequent relapses and multiple polyps, extirpation of the uterus and appendages is recommended, since these factors significantly increase the risk of malignancy of neoplasms.
Treatment of endometrial glandular polyp after removal
This is an important stage of therapy. In order to restore hormonal levels, the following are used:
- gestagens (drugs containing progesterone): Micronor, Levonorgestrel, Duphaston, Utrozhestan;
- gestagen-estrogenic drugs or combined oral contraceptives: Yarina, Zhanin, Diane-35.
Progesterone-containing drugs are prescribed for treatment, in particular Utrozhestan
The regimen and duration of therapy is determined by the gynecologist individually for each patient.
If the results of a cytological examination of the material taken during a biopsy indicate malignancy and there are signs of an oncological process, the treatment differs from the usual and must be carried out by a gynecological oncologist.
Prevention methods
In order to reduce the risk of the disease, regular examinations by a gynecologist are necessary. All inflammatory or infectious processes must be treated promptly. Taking care of your health will bear fruit. Experts recommend choosing contraceptives wisely and planning to conceive a child. This will significantly reduce the likelihood of abortions, which can cause a condition such as endometrial polyposis. Any disruptions in the functioning of the body should immediately alert the woman. If a problem is detected, postponing a visit to the doctor is undesirable and dangerous.
Complications
A timely and adequately untreated glandular polyp can cause the following complications:
- infertility, miscarriage, placental abruption, fetal hypoxia during pregnancy;
- metrorrhagia (uterine bleeding) with the development of anemia;
- addition of infection or disruption of blood supply with the development of necrosis;
- malignancy, adenomatous transformation.
For early detection of endometrial hyperplastic processes and other gynecological pathologies, it is necessary to visit a gynecologist regularly (at least once a year), try to eliminate risk factors, and promptly treat gynecological diseases.
Cases when surgery cannot be avoided
The neoplasm cannot be cured with medications. If the growth is small or there are contraindications for surgery, the doctor prescribes hormone therapy and symptomatic medications. The conservative method involves reducing the growth rate of the tumor and eliminating the manifestations of the disease (bleeding, pain). Methods for eliminating polyps are only surgical.
The reason for prescribing mandatory surgery is the increased risk of malignancy (adenomatous polyp, frequent bleeding, etc.)