Causes of mastitis
The most common (82 - 92%) cause of mastitis is Staphylococcus aureus (Staphylococcus aureus) in the form of a monoculture or in combination with other microorganisms - Escherichia coli and Pseudomonas aeruginosa, Proteus, streptococci, bacteroides).
The source of infection is patients suffering from purulent-inflammatory diseases, so lactation mastitis often develops in the maternity hospital soon after childbirth or in the first days after discharge from the hospital.
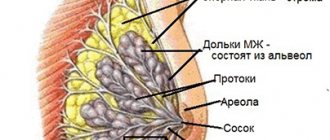
The entry point for infection is cracked nipples. Sometimes pathogens penetrate intracanalicularly (through the thoracic duct), which occurs when expressing milk and feeding a baby. In addition, bacteria can enter the mammary gland through lymphatic and blood vessels.
The following factors contribute to the spread of infection:
- Unpreparedness of the mammary gland, which is often observed in primigravidas.
- Impaired milk flow (80 - 90%).
- Cracked nipples.
- Decreased immunity, which is facilitated by diseases during pregnancy (pyelonephritis, anemia), as well as complications that arise during pregnancy, during childbirth and after childbirth.
- Improper nipple care.
- Availability of silicone implants.
- Smoking.
The risk group for lactation mastitis includes women with mastopathy, abnormal nipple development, giving birth at a late age, patients with rheumatoid arthritis, diabetes mellitus, and people taking glucocorticoids.
Rice. 2 and 3. Lactation mastitis.
Treatment
The initial stage of purulent mastitis can be treated with conservative and traditional methods. Advanced infiltrative and abscess forms require surgical intervention.
Conservative methods
Patients with serous lactation mastitis are recommended:
- limit physical activity and stay in bed;
- express milk every 3 hours;
- take laxatives based on sodium sulfate to dehydrate the body and suppress lactation;
- administer antispasmodics intramuscularly twice a day: no-shpa, pituitrin, papaverine hydrochloride solution in combination with oxytocin;
- take antibacterial drugs.
Patients with the first symptoms of mastitis are prescribed broad-spectrum antibacterial agents and milk culture for bacteria. After receiving the tests, the doctor selects medications taking into account the sensitivity of the microflora. Antibacterial agents can be supplemented with antihistamines to relieve swelling. The drugs are best administered intramuscularly or intravenously.
Conservative methods of treating mastitis include early radiotherapy and electrophoresis of novocaine or ethyl alcohol. Ultrasound exposure, irradiation with a Sollux lamp, applications with ozokerite and other thermal physiotherapeutic procedures are prescribed after normalization of body temperature and reduction of breast swelling.
In the early stages of purulent mastitis, an ice pack wrapped in a fabric bag is applied to the mammary gland. Cold suppresses lactation, relieves spasms in the milk ducts and reduces discomfort. Ice treatment is recommended in the first 4–5 days of acute mastitis.
Probiotics for Pain Reduction
Lactanza Lc40
A special probiotic for the mammary gland, Lactanza Lc40, helps reduce pain due to mastitis. The lactobacilli Lc40 included in its composition regulate the level of inflammation, helps reduce pain and the number of pathogenic bacteria that actively multiply during illness. Lc40 Lactans will help maintain healthy breastfeeding. Since it helps to normalize the microbial composition of the mammary gland and breast milk, which reduces the risk of relapse of mastitis in the mother and intestinal infections in the baby.
Traditional methods
Home remedies for mastitis should only be used after consulting a doctor. The most popular methods include:
- Herbal tea made from lemon balm, thyme and chamomile. Infusions are taken orally to strengthen the immune system and reduce inflammation.
- Honey rubbing. Diluted honey has antiseptic properties and heals cracked nipples.
- Cabbage compresses. Cabbage leaves draw out water and relieve swelling, relieve pain and help with extreme heat.
Rubbing and compresses are used only cold. Heat increases the growth of bacteria and can cause mastitis to worsen.
Operation
Surgical intervention is recommended for chronic and advanced acute forms, as well as for non-lactation mastitis that occurs against the background of mastopathy or fibroadenoma. The operation is performed under general anesthesia, less often under local anesthesia.
The doctor opens and cleans the ulcers, installs a drainage system for washing the inflamed cavities with antiseptic solutions. In advanced cases, purulent abscesses are resected along with surrounding tissues.
After the operation, the woman is additionally prescribed a low-dose UHF electric field, laser therapy and intravascular ultraviolet irradiation.
How the disease develops
Mastitis affects the breast parenchyma and/or interstitial tissue. Inflammation quickly spreads through the delicate parenchyma even after surgical incision of the abscess. Initially, the inflammation is serous in nature. Over time, the pathological process becomes purulent with the formation of abscesses.
Milk in the acini of the mammary gland is a good breeding ground for microbes that multiply intensively when lactostasis develops. Due to the dense network of milk and lymphatic ducts, the presence of a large amount of fatty tissue and cavities, inflammation rapidly spreads to neighboring areas, even with adequate therapy.
If the inflammatory process is limited to the milk ducts, then milk is released mixed with pus.
Rice. 4. Purulent form of lactation mastitis.
Features of diagnostics
If a woman discovers pus from the nipple of the mammary glands, she should immediately contact a mammologist. A particularly urgent visit to the doctor’s office is required in the following cases:
- Discharge of purulent secretion with blood.
- The flow of pus is profuse and does not stop.
Experts warn against self-medication, which often only aggravates the course of the disease and provokes the development of severe complications.
After examining the mammary glands, the doctor will prescribe a diagnostic test to clarify the root cause of the pathological phenomenon:
- X-ray of the breast.
- Ultrasound.
- Ductography.
- Mammography.
- Needle biopsy.
You will also need to pass laboratory tests:
- General blood test.
- Hormone analysis.
- Test for tumor markers.
- Cytological test of pus.
Based on the examination data obtained, a diagnosis is established and a treatment regimen is developed.
Classification
Mastitis is divided into:
- Lactation (80 - 85%), non-lactation (10 - 15%), including pregnancy mastitis (0.5 - 1%).
- According to the course: acute and chronic.
- By localization - subcutaneous, intramammary (in the gland itself) - the most common, retromammary (behind the gland), diffuse.
- According to the nature of inflammation, acute lactostasis, serous, infiltrative and destructive (abscessing, phlegmonous and gangrenous) mastitis are distinguished.
- Rare forms of lactation mastitis: galactophoritis (inflammation of the milk ducts) and areolitis (inflammation of the areola).
- Specific: tuberculosis and syphilitic.
- Chronic mastitis: purulent and non-purulent.
Rice. 5 and 6. Lactation mastitis.
What treatment is indicated for the presence of pus?
Doctors advise against self-treatment, especially if the symptomatic manifestations are severe. First of all, it is necessary to identify the nature of the disease that led to the formation of pus, and only then decide on therapy.
However, there are situations when it is not possible to visit a doctor’s office in the next few hours. In this case, you can use external medications to alleviate the condition.
How to remove pus from a nipple at home? The following medications help:
- Vishnevsky ointment.
- Levomekol.
- Ichthyol ointment.
- Solcoseryl.
- Bepanten.
- Panthenol.
- Baneocin.
Even after successful use of external remedies, you should consult a doctor at the first opportunity.
Treatment against diseases
Features of therapy depend on what pathological processes cause the appearance of purulent secretion from the nipples:
- Inflammation. For mastitis, anti-inflammatory and antiseptic drugs are prescribed, and in severe situations, surgical intervention is used.
- Bacterial infections. Treatment with antibiotics and, in some cases, hormonal agents is recommended.
- Intraductal papilloma. It can be cured surgically (excision of the affected area of the breast is performed).
- Surgery. It is performed in situations where it is necessary to open a boil or remove a tumor in the breast tissue.
- Malignant tumors, including Paget's disease. A mastectomy of both glands is prescribed or only one formation is removed.
Use of medications
| Drugs | Drug effect | Name |
| Nonsteroidal anti-inflammatory drugs | Reduce pain. Relieves swelling. Suppress the inflammatory process. | Nimesulide. Diclofenac. Indomethacin. |
| Analgesics | Relieves pain. | Analgin. Tempalgin. Paracetamol. |
| Antibiotics | Inhibits the activity of pathogenic organisms. | Amikacin. Cefazolin. Isepamycin. Tobramycin. Cephalexin. Kanamycin. |
Signs and symptoms of mastitis
All forms of mastitis have an acute onset: body temperature rises to 38 - 400C, weakness, headache and chills appear, appetite decreases, and general health deteriorates. The mammary gland in the affected area is hyperemic, sharply painful and hot to the touch.
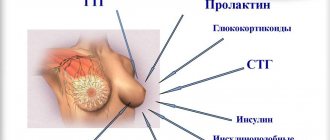
Lactation mastitis most often develops between 1 and 3 weeks in the postpartum period. Its development is facilitated by milk retention (acute lactostasis), which occurs from the 3rd day of the postpartum period and in the next 6 weeks. The clinical picture of the disease depends on the nature of the inflammatory process.
Rice. 7. The photo shows the location of the abscesses: subareolar (1), intramammary (2), retromammary (3).
Signs and symptoms of acute lactostasis
Severe pain due to cracked nipples is the reason for refusal to feed the newborn and express milk, which leads to stagnation of milk in the ducts of the mammary glands - acute lactostasis. Tension and a feeling of heaviness appear in the mammary gland. Upon palpation, compactions are revealed in individual lobules; they are mobile, have clear boundaries, and are painless. The woman's general condition remains satisfactory. Expressing milk brings relief. With regular implementation, the situation often normalizes. If measures are not taken, infectious mastitis develops, requiring surgical intervention.
In case of acute lactostasis, it is necessary to organize emptying of the mammary glands, restore milk secretion and its separation. For this purpose, you should adjust the feeding regimen and expressing remaining milk, including using a breast pump.
Reduced milk secretion is caused by fluid restriction and taking medications such as Parlodel or Dostinex.
Signs and symptoms of serous mastitis
The milk in the acini of the mammary gland is a good breeding ground for microbes. When lactostasis has developed, their rapid reproduction and spread is noted, which is facilitated by a dense network of milk and lymphatic ducts, the presence of a large amount of fatty tissue and cavities. After infection, serous mastitis develops within 2 to 4 days.
The onset of the disease is acute, body temperature reaches 39 - 400C. Chills, weakness, headache appear, and appetite decreases. There are changes in the general blood test, and the ESR increases.
There is a feeling of tension and heaviness in the mammary gland that does not disappear after pumping, bursting pain and local heat. Diffuse tissue swelling. The compaction is sharply painful on palpation. With untimely and inadequate treatment, after a few days serous mastitis becomes infiltrative.
Rice. 8. Lactation mastitis, serous form.
Signs and symptoms of infiltrative mastitis
With infiltrative mastitis, a painful infiltrate forms in the tissues of the gland, sharply painful on palpation, and there are no areas of softening. The skin over the infiltrate is sharply hyperemic. The body temperature takes on a hectic character. Intoxication symptoms are pronounced.
If treated incorrectly, inflammation during infiltrative mastitis becomes purulent.
Signs and symptoms of purulent mastitis
If treatment is ineffective, the infiltration phase is replaced by an abscess formation phase, when foci of purulent melting appear in the infiltrate, and a symptom of fluctuation is determined by palpation. At the same time, the patient's condition sharply worsens. The number of leukocytes in the blood reaches 15 - 20x109/l, ESR accelerates to 30 - 50 mm/hour. Palpation in the area of suppuration is sharply painful. Inflammation quickly spreads beyond the primary focus.
Abscesses are divided according to localization into subareolar, intramammary and retromammary.
Rice. 9. Lactation mastitis, purulent form.
Signs and symptoms of phlegmonous mastitis
With phlegmonous mastitis, 3-4 quadrants of the mammary gland are involved in the infectious process. It increases significantly in volume. The skin over the lesion is sharply hyperemic, shiny, in places with a cyanotic tint, sometimes takes on the appearance of a “lemon peel”, the superficial veins are dilated, the nipple is retracted. The entire infiltrate is subjected to purulent melting.
The patient's condition deteriorates sharply. Symptoms of intoxication are pronounced. Dry mouth and nausea, insomnia and severe headaches appear, and there is a complete loss of appetite. Body temperature rises to 400C, accompanied by stunning chills. Regional lymphadenitis is recorded.
The number of leukocytes in the blood reaches 20 x109/l, ESR accelerates to 50 mm/hour, red blood cells, protein, granular and hyaline casts appear in the urine (toxic urine).
Rice. 10. Phlegmonous mastitis.
Signs and symptoms of gangrenous mastitis
If you seek medical help too late, gangrene of the organ (gangrenous mastitis) may develop. The cause of the disease is thrombosis of the vessels of the organ parenchyma. The area of destruction extends to all quadrants of the mammary gland.
The condition of the patients is extremely serious. The temperature reaches extremely high numbers, the pulse reaches 120 beats/min, and the filling is weak. The skin is pale. Lips and tongue are dry. Weakness, headache, loss of appetite progress, and insomnia appears.
The mammary gland significantly increases in size, upon palpation it is sharply painful, pasty, swollen, the skin over it is dirty green, and sometimes blisters appear. The nipple is retracted. Milk is not released from the mammary ducts. Regional lymphadenitis is recorded.
The number of leukocytes in the blood reaches 30 x109/l, ESR accelerates to 50 - 60 mm/hour, a sharp shift of the formula to the left. Hemoglobin drops to 100 g/l. Red blood cells, protein, granular and hyaline casts appear in the urine (toxic urine).
Rice. 11. Gangrenous form of mastitis.
Treatment of breast inflammation
Mastitis must be treated. You cannot run the process to avoid negative consequences. Treatment of inflammation of the mammary glands in women at the initial stage is carried out by doctors using medications and physiotherapy. Antibiotic therapy, rest, and regular breastfeeding will help you recover faster. With immediate treatment, you will feel better within 48 hours.
Mastitis usually causes fever, as well as pain, redness, and swelling of the affected breast. The presence of a lump in the breast indicates abscess formation, which usually requires surgical drainage. Treatment for breast inflammation in women usually involves medication, with surgical drainage of abscesses if present.
Breastfeeding women need to express excess milk in time to empty the affected mammary gland. If the baby cannot get all the milk through breastfeeding or if the feeding procedure is too painful, you should use a breast pump to empty the breast until the pain goes away.
A cold compress, such as crushed ice, on a damp cloth placed on the sore, red area of the gland for 20 minutes is a known folk remedy that will help relieve pain between feedings. Many mothers have found that chilled cabbage leaves inserted inside the bra cup around the affected area of the breast can also reduce soreness.
Compatible painkillers or anti-inflammatory drugs will help, but they should be taken after consulting a specialist. If purulent cavities in the mammary gland and a large number of leukocytes in the blood are detected, the doctor may prescribe antipyretics and antihistamines. Physiotherapy procedures have proven themselves to be effective for the treatment of breast cysts, as well as the prevention of purulent mastitis.
Advanced forms, such as purulent and gangrenous, require surgical intervention. Local removal of an abscess takes place under local anesthesia, and the operation is carried out under the careful supervision of a mammologist. Its outcome in 85% of cases shows good results and gives positive feedback from patients. Doctors will take a puncture to study cytology so as not to miss cancer. Resection is carried out sectorally, the damaged area of the gland is removed.
Important points in the prevention of breast inflammation
Mastitis usually occurs in nursing mothers, pregnant women, and menopause, when bacteria enter the body through cracks in the nipples. This may cause an infection. Usually it all starts with a slight tingling sensation, which intensifies over time, causing fever and burning pain near the nipples. To prevent a dangerous disease, you must follow some rules:
- Nursing mothers need to adhere to a feeding schedule and express the remaining milk from the breast. Dry your nipples after each breastfeeding session to prevent irritation and cracking. Use a lanolin-based ointment, such as Dimexide, to keep the breast skin healthy. This cream can also be used to relieve pain in wounds or cracks.
- Eat healthy foods and drink plenty of fluids whenever your body feels thirsty.
- When the time comes to wean the baby, breastfeeding is gradually stopped. Gradual weaning is better for both. This helps prevent the mammary gland from overfilling with milk, and the newborn will quickly adapt to new feeding patterns.
- Wear only comfortable, properly sized underwear made from natural fabrics.
- During puberty, girls' hormonal levels begin to change, so a teenager should not be ashamed of his constantly changing breasts and try to wear tight-fitting clothes. All this can cause the development of inflammation in the glands. Parents should explain to the child that all changes in his body are natural and are not pathology.
- Poor latching is a major risk factor, so one of the main methods of prevention and treatment is to review breastfeeding practices. The first week is indicative of the establishment of the correct capture of the glands in the baby.
- Hygiene in this case is as important as performing gymnastic exercises.
- Every month it is necessary to conduct an independent inspection to identify the formation of compactions and lumps. A timely, planned visit to a gynecologist reduces the risk of developing complications and chronic forms of the disease by 55%.
Mammologists and gynecologists are the best health care specialists for diagnosing breast inflammation. They base their assessment on the description of symptoms and on physical examination, instrumental and chemical tests. Strictly speaking, there is no medical test that can confirm the diagnosis. But psychosomatics often becomes the main manifestation of pathology.
Although mastitis usually affects women who breastfeed, it can still develop in teenage, non-breastfeeding men.
It is extremely important to take your medications as prescribed, consistently, until the end of your treatment period.
Non-lactation mastitis
Microorganisms in non-lactation mastitis penetrate into the mammary gland from outside due to accidental injury, burns or from areas of skin affected by pustular infection. The spread of microorganisms occurs through the subcutaneous fatty tissue. The glandular tissue of the gland is affected secondarily.
Rice. 12. The photo shows a picture of non-lactation mastitis, the cause of which was a breast boil.
Preventive measures
To prevent the development of this disease, it is necessary to prevent weakening of the immune system, promptly treat infectious diseases, observe personal hygiene standards, and the milk duct of the breast should not be injured.
Non-lactation mastitis can strike a woman at any time. Therefore, it is necessary to promptly contact a specialist if any pathological changes in the mammary glands are detected.
You will learn about the forms, symptoms and treatment of mastitis from our video.
Diagnostics
The diagnosis of mastitis is made based on the clinical symptoms of the disease. Significant assistance is provided by ultrasound and bacteriological examinations, mammography, as well as express diagnostics with dimastin and Diana diagnosticum. Mastitis should be distinguished from cystic mastopathy and breast cancer.
Ultrasound signs of serous lactation mastitis:
- Lactostasis.
- Shaded picture.
Ultrasound signs of infiltrative lactation mastitis:
- Lactostasis.
- Determination of areas of homogeneous structure surrounded by an area of inflammation.
Ultrasound signs of purulent lactation mastitis:
- Dilation of ducts and alveoli surrounded by an infiltration zone (symptom of “honeycomb”).
- Visualization of a cavity with bridges and jagged edges, surrounded by an infiltration zone.
Rice. 14 and 15. Ultrasound signs of purulent mastitis. Cavities are indicated in dark color: single (left) and multiple (right).
Treatment of mastitis
Treatment of mastitis is complex. Timely and adequate therapy almost always ends in recovery. Death is recorded in 0.05% of cases in severe forms of the disease. Non-purulent forms of lactation mastitis are treated conservatively, purulent forms - only surgically.
Conservative methods of treatment for serous and infiltrative mastitis include:
- antimicrobial therapy,
- infusion therapy,
- desensitizing therapy,
- drug cessation of lactation,
- immunostimulation,
- physiotherapy,
- retromammary novocaine blockade.
It is necessary to maintain an elevated position of the mammary gland, which is achieved by wearing a bra and bandages that do not compress the organ. Breastfeeding continues. Administration of antispasmodics is allowed. Rough massage is absolutely excluded! The milk is sucked out by a breast pump. A retromammary novocaine (lidocaine) blockade with the antiseptic Decasan is used, which helps to expand and eliminate spasm of the thoracic ducts, which, in turn, facilitates the release of milk.
Broad-spectrum antibiotics are used among antimicrobial drugs.
In the treatment of mastitis, metronidazole is widely used, to which many types of anaerobic microorganisms are sensitive.
Infusion therapy is carried out using hemodez, plasma expanders, protein preparations, gamma globulin and saline solutions.
Physiotherapeutic procedures are widely used in the treatment of serous mastitis: microwave therapy, ultraviolet radiation, ultrasound. When treating infiltrative mastitis, the same procedures are used, but with an increased thermal load.
After relief of clinical manifestations, restoration of lactation is allowed, which is achieved by using Bromicriptine or Dostinex (Carbergoline).
The issue of stopping lactation is decided individually. The main indications are severe and treatment-resistant mastitis. To suppress lactation, drugs such as Parlodel or Dostinex are used.
Treatment of destructive forms of mastitis
All forms of purulent lactation mastitis are subject to surgical treatment, which consists of opening and draining the abscess cavity. The operation is performed under local anesthesia or general anesthesia. The tendency to relapse obliges the surgeon to carefully perform the operation, open all existing abscesses and infiltrates, perform a complete necrectomy and perform rational drainage. In the postoperative period, it is necessary to carry out anti-inflammatory, detoxification and immunostimulating therapy. The nipple must remain free of the bandage for the milk expression procedure.
Types of incisions during surgery:
- Linear (with subcutaneous ulcers).
- Lunar (with subareolar ulcers).
- Radial and arcuate (with intramammary abscesses).
- An incision under the mammary gland (for retromammary abscesses).
For phlegmonous mastitis, the same incisions are made, but the necrectomy is wider.
For gangrenous mastitis, a wide necrectomy is performed. In some cases, the mammary gland must be amputated.
Rice. 16 and 17. Scheme of retromammary novocaine blockade (left). The main types of incisions when opening breast abscesses (right): radial incisions (1), Bardenheier incision (2), paraareolar incision (3).
Treatment methods
For purulent mastitis, treatment should be timely and comprehensive, including surgical and conservative therapy. A conservative treatment method without surgical intervention is carried out only if the disease is in the serous stage without accumulation of pus in the glandular ducts.
Conservative
Conservative treatment should be carried out only in the first days of the disease, no later than five days. Before starting treatment with medications, it is necessary to ensure rest for the mammary gland and regularly express milk.
The main and widely used drugs include:
- oxytocin 0.5 ml IV, to reduce milk production by the mammary glands;
- solution of platifilin 2% IM or diclofenac 5 ml to relieve pain;
- solution of trypsin or chymotrypsin 10 mg in combination with novocaine 0.5% for retromammary blockade;
- a solution of ceftriaxone 1.0 to 10.0 sodium chloride intravenously in a bolus to eliminate the bacterial pathogen.
To improve the pharmacokinetic properties of drugs and improve general microcirculation in a woman’s body, physiotherapeutic procedures are used, which include:
- exposure to ultrasonic radiation at the site of damage;
- phonopheresis with the addition of enzymatic preparations;
- exposure to x-rays.
In the complete absence of positive dynamics in the patient, surgical intervention is indicated.
Surgical
The surgical method of treating a purulent disease is considered the fastest and most effective; this is due to the massive accumulation of pus in the glandular tissue. For purulent mastitis, the operation can be performed in the form of a puncture puncture of the abscess cavity, followed by suction of the purulent contents.
If there are many pustules or a large abscess, the surgeon makes several incisions throughout the inflammatory focus, extracts pus from the wound, rinses the abscess cavity with antiseptic solutions and installs passive drainage to drain the remaining pus.