Metroendometritis is an inflammation of the uterus, namely, an inflammatory process in the mucous and muscular lining of the uterus. Such inflammation after childbirth occurs as a result of the entry into the uterus of a septic infection such as E. coli streptococci, staphylococci and gonococci, as well as the penetration of other microorganisms.
Metroendometritis appears on the 3-4th day in most cases after childbirth or abortion. This complication occurs as a result of the formation of blood clots or remnants of placental tissue in the uterus.
Almost all complications and inflammation after childbirth occur in the uterus. Inflammation of the uterus can be expressed in different ways. Inflammation can manifest itself not only on the inner surface of the uterus, but also on all layers of the uterine wall. It follows that metroendometritis manifests itself in a variety of ways.
Acute form of metroendometritis
Symptoms of the acute phase appear at the very beginning of the disease and usually last no longer than one week. The main features boil down to:
- increased body temperature;
- apathy and weakness;
- chills;
- increased fatigue;
- pain in the lower abdomen;
- possibly increased heart rate and nausea.
During the acute course of the disease, body temperature can reach 39 degrees, and severe pain can spread to the sacrum and groin area. During this period, a woman experiences unbearable pain in the uterine area, swelling appears, and the pain increases sharply when palpating the organ. In the process of complete rejection of the mucous layer of the endometrium, it disintegrates, and the inflammatory process spreads to the muscle layer, lymph nodes and blood vessels.
Complications that appear in the acute phase of metroendometritis can lead to uterine sepsis, which is extremely dangerous not only for the health, but also for the life of the patient.
How to treat
A treatment regimen for chronic endometritis can only be effective if it includes the following criteria:
- elimination of the causative agent of the inflammatory process;
- normalization of the menstrual cycle;
- elimination of signs of the disease;
- restoration of the female body’s ability to bear offspring.
Since treatment must cover several problems, it occurs in several stages:
- infections are eliminated;
- increasing the body's resistance to diseases;
- restoration of the body's metabolic processes;
- treatment with hormones, including hormonal contraceptives.
Let's consider an approximate scheme according to which diseases are treated:
- Since most often chronic processes are of bacterial origin, intrauterine treatment with antibacterial or antiviral medications is initially prescribed. If the disease is in the active phase, then antibiotics of 2-3 types are used simultaneously. 1 or 2 drugs are administered intramuscularly, intravenously or in tablet form, and the third drug is given intrauterine infusion through a thin catheter. If the causative agent of inflammation is a herpes virus or cytomegalovirus, Acyclovir may be prescribed by the attending physician. If the cause is a fungal infection, Hexicon suppositories and other local or systemic drugs may be prescribed.
- To stimulate the immune system, medications based on animal thymus, interferon preparations and polyoxidonium are prescribed.
- If there are a large number of adhesions and polyps in the uterus in a woman who is still planning a pregnancy, surgical intervention is indicated. Excision of these formations is carried out using an electrocoagulator loop under the control of a hysteroscope.
- The last stage of treatment is restorative and should ensure natural processes in the endometrium. Hormonal contraceptives, progesterone-based medications, hemostatic and vascular strengthening agents, as well as metabolic and enzyme preparations are prescribed. To eliminate inflammation, suppositories with indomethacin (rectal) or diclofenac can be used.
In addition to drug treatment, physiotherapy plays an important role. A good effect from physiotherapy appears after UHF, magnetic therapy, ultrasound treatment, and lidase electrophoresis. The patient is also shown resorts where she can undergo the same physiotherapeutic procedures and supplement them with mud and hydrotherapy, as well as drinking slightly alkaline mineral water.
Good results in the treatment of inflammatory processes in the uterus are attributed to hirudotherapy. Leeches are placed on the lower abdomen and vagina for a maximum of half an hour. You need to undergo about 15 such procedures with breaks of 1-2 days. On ultrasound, the effect of them appears after 2 months.
Subacute
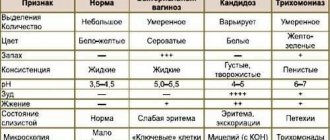
The main symptoms in the subacute stage of the disease are bloody, purulent and mucous discharge. Pus in the subacute form is released less intensely compared to the acute phase. It is at this stage that the symptoms of the disease can proceed quite unnoticed and develop into a chronic form, the treatment of which is much more difficult and lengthy.
Pain in the abdominal area in the subacute form is less intense and is characterized primarily as pulling and unpleasant, but can also spread to the lumbar and groin areas. Another characteristic symptom of the subacute stage is long and heavy menstruation, in some cases even menorrhagia may occur. When the course is particularly intense, inflammatory processes contribute to the destruction of myometrial tissue, which leads to their replacement with connective fibers.
Kinds
Classification is carried out based on various factors. Thus, according to the nature of the causative agent of the inflammatory process, there are chronic nonspecific and specific endometritis. The reason for the first is opportunistic microflora, which normally lives in small quantities in the vagina, perineum and anus. Such organisms include cocci, Proteus, Klebsiella, Gardnerella and Escherichia coli.
The cause of specific endometritis is yeast-like fungi, herpes simplex viruses, cytomegalovirus, chlamydia, mycoplasma and other bacteria localized inside cells.
Based on morphological characteristics, the following types are distinguished:
- atrophic, in which atrophy of the glands, fibrosis of the stroma and its infiltration by lymphoid elements occurs;
- hypertrophic, when inflammation causes mucosal hyperplasia;
- cystic, overgrown fibrous tissue presses on the glands, the contents in them thicken, forming cysts.
According to the nature of the inflammatory process, the disease is divided into three degrees of activity:
- Moderate degree of activity. This stage is characterized by the presence of subjective symptoms; inflammation is visible on ultrasound. A biopsy performed during hysteroscopy will show changes in endometrial tissue caused by a fairly active inflammatory process.
- Sluggish endometritis. It has minimal manifestations, which are visible only with an ultrasound of the uterus. A biopsy will show the presence of changes in tissue caused by low-grade inflammation.
- With chronic inactive endometritis, that is, with a disease in remission, signs of the disease can only be detected by microscopic examination of the endometrium, since there are no obvious symptoms.
According to the degree of prevalence of the inflammatory process, endometritis can be focal (develops only in some areas of the inner uterine lining) and diffuse (inflammation affects almost all or all of the endometrium).
According to the depth of damage to the endometrium, the disease can be superficial, occurring only in the inner layer of the uterus and affecting the muscle tissue of the organ.
Another way to classify endometritis is a morphological assessment of the severity of the disease. The assessment is carried out by scraping the endometrium, and the result is given in the form of points. With a mild degree of severity of the disease, a score is given from 1 to 4, with a moderate severity - 5-7 points. If, based on the signs, area occupied and homogeneity of the endometrium, inflammation scores 8-10 points, it can be classified as severe.
Chronic
It is the most common type of disease, the symptoms of which are especially characteristic of postmenopausal women. The chronic form of metroendometritis, as well as its acute form, contributes to the destruction of the mucous membrane in the uterine cavity and the spread of lesions to muscle tissue. Advanced stages contribute to the emergence of complications and the spread of infectious processes to the peritoneum and pelvic vessels. More severe complications, such as sepsis and persistent bleeding, are also possible.
Symptoms of the disease
The most common symptoms of any form of metroendometritis are:
- mucous, bloody and purulent vaginal discharge;
- increased body temperature (in acute and subacute forms it can reach 39 degrees, chronic forms are caused by constant low-grade fever - up to 37.8 degrees);
- various types of irregularities in the menstrual cycle (intercyclic bleeding, prolonged heavy or, on the contrary, too scanty periods, cycle failure);
- leukocytosis, leading to weakness, difficulty breathing, increased sweating, pain in the limbs;
- an increase in ESR (erythrocyte sedimentation rate);
- Difficulties in the process of conception, regular miscarriages, infertility.
Complications
The most dangerous complication of this disease is infertility.
Even when the long-awaited conception occurs, the disease can cause, if not miscarriage, then a complicated course of pregnancy and childbirth. The inflammatory process can cause oligohydramnios, disrupt fetoplacental blood flow and contribute to intrauterine infection of the fetus. With this disease there is a high risk of developing the following pathological conditions:
- ectopic pregnancy;
- endometrial diseases;
- inflammatory and purulent processes in the pelvic organs;
- neoplasms and cysts in the ovaries.
Reasons for appearance
Causes of acute and subacute appearance
The infection process occurs due to the entry of pathogenic microorganisms, fungi or bacteria into the uterine cavity. Most often, the disease is provoked by pathogenic microorganisms such as streptococci, gonococci, staphylococci, as well as E. coli, etc. The most likely cause of infection is various gynecological operations, childbirth, abortion, unprotected sexual intercourse (especially during menstruation), as well as neglect of basic rules hygiene.
Often the cause of metroendometritis can be a common cold or flu.
Symptoms of acute or subacute metroendometritis may appear several days after birth. Indeed, during labor, the uterine cavity remains completely unprotected for various types of infections. It should be noted that after a caesarean section the risk of infection is much higher than during a natural birth.
Reasons for education
Most often, symptoms of the chronic stage of the disease appear as a result of an untreated acute form. Much less often it is noted as an independent disease. Often the chronic form of the disease is a consequence of the activity of bacterial infections, for example, chlamydia and other harmful sexually transmitted bacteria.
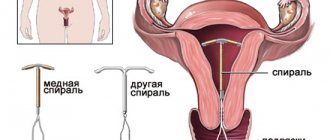
As in the case of acute metroendometritis, the chronic form can be caused by various gynecological procedures and operations: abortion, hysteroscopy, removal of tumors or polyps.
The main risk factors include:
- installation of intrauterine devices;
- pregnancy (during gestation, severe hormonal disturbances occur, and the functioning of the immune system decreases);
- diagnostic curettage and probing;
- unprotected sexual intercourse;
- self-douching;
- use of tampons;
- early onset of sexual activity after childbirth.
Despite the fact that infection occurs as a result of the ingestion of harmful bacteria and microorganisms, the development of the disease usually occurs against the background of reduced immunity and disruptions in the functioning of the body’s protective functions.
Treatment
Mandatory hospitalization is required for those patients who have acute metroendometritis or if it occurs immediately after childbirth. The lack of adequate treatment during this period can cause complications such as sepsis and uterine bleeding, which in the most severe cases lead to death.
When conducting outpatient treatment, complete rest, bed rest, diet and cold compresses on the lower abdomen are recommended, which will help reduce the local temperature and reduce pain.
If metroendometritis occurs as a result of a miscarriage, a course of intrauterine antiseptic lavages is required. They allow you to cleanse the uterine cavity of blood clots, reduce the symptoms of inflammation and eliminate the proliferation of pathogenic microorganisms.
Drug therapy
The main treatment for this disease involves:
- broad-spectrum antibiotics;
- antimicrobial agents;
- analgesics that relieve pain;
- sulfonamides.
In case of heavy uterine bleeding, ascorbic acid and vasoconstrictor drugs are additionally prescribed. Hormonal imbalances are treated with a course of corticosteroid medications.
The chronic form of the disease is treated comprehensively. In addition to mandatory drug therapy, physiotherapeutic procedures are also prescribed: mud therapy, hirudotherapy, sanatorium treatment, electrophoresis, light therapy and much more.
Application of traditional methods
The use of some folk recipes can really alleviate the patient’s condition, remove the main symptoms and speed up the recovery process. But it should be taken into account that such treatment should be comprehensive, combined with conservative methods and selected together with a herbalist.
Self-treatment with folk remedies is strictly prohibited, since incorrectly selected methods can worsen the condition and lead to serious complications.
Recommended treatment during remission or prevention of the disease involves:
- self-douching with solutions of sage, chamomile, nettle or linden flowers;
- drinking medicinal decoctions and tinctures from herbal collections;
- sitz baths with the addition of herbs that have anti-inflammatory and soothing effects.
Treatment of metroendometritis during pregnancy
Undoubtedly, a disease diagnosed during pregnancy can have a very negative impact on the development of the fetus and the course of pregnancy as a whole. Complications that are possible with the development of metroendometritis during pregnancy are premature birth, dysfunction, difficulties in the activity of the placenta, intrauterine hypoxia, and delayed fetal development.
Since most of the drugs used in the treatment of this disease are quite strong and can harm the child, therapy is not used for the indolent form of the disease. Pregnant women are specially registered with a specialist, and treatment is carried out already in the period after delivery. However, the presence of metroendometritis has no effect on the birth process itself.
Is it possible to cure
High-quality and timely diagnosis gives a positive prognosis for cure. It is quite possible to permanently cure a chronic inflammatory process in the reproductive system; it is important to choose a successful treatment regimen that takes into account the degree of the disease, the activity of the process, the presence of complications and the type of pathogen that caused this pathology. Modern medicine offers treatment of endometritis in 2, maximum 4 stages, while the non-acute course of the disease allows the course to be completed on an outpatient basis.