Causes of the disease
Endometritis is a polymicrobial disease. The reason for its development is various opportunistic aerobic and anaerobic bacteria that make up the normal microflora of the lower genital tract of women:
- Escherichia coli (Escherichia coli), Enterococcus faecalis (fecal enterococci), Bacteroides fragilis (bacteroid fragilis).
- Strepto- and staphylococci.
- Sexually transmitted pathogens - chlamydia, mycoplasma, ureaplasma, gardnerella.
- Mushrooms of the genus Candida.
- Herpes viruses and cytomegaloviruses.
- Among specific endometritis, the causative agents of gonorrhea, tuberculosis, actinomycosis and syphilis are recorded.
Increasingly recently, an association of microorganisms such as chlamydia and herpes simplex viruses has been identified.
Therapeutic measures
Treatment of postpartum endometritis requires the mandatory use of antibacterial therapy, against the background of which breastfeeding should not be done. Important conditions for the effectiveness of drug treatment are the earliest possible start of taking broad-spectrum antibiotics and complex therapy of inflammation in a hospital setting. When prescribing antibiotics, the doctor will consider the following factors:
- probable or identified types of infection in bacterial culture;
- the period of time that has passed since childbirth;
- delivery option (natural birth or cesarean section);
- severity of symptoms;
- severity of general condition;
- risk of complications.
In addition to antimicrobial medications, the following treatments should be used:
- droppers with solutions that reduce the severity of inflammatory intoxication;
- anti-inflammatory drugs;
- increasing immune defense;
- vascular drugs;
- symptomatic medications.
If there is a high risk of sepsis or peritonitis, surgical intervention will be required: in order to save the life of a postpartum woman, it is necessary to remove the source of infection - the uterus affected by endometritis.
Risk factors
There are a number of factors leading to the development of acute endometritis:
- Childbirth complicated by injuries.
- Long-term use of intrauterine contraceptives.
- Damage to the vagina caused by neglect of personal hygiene and frequent douching.
- Conditions for the development of pathogenic microorganisms are created by spotting, which is caused by menstruation, abortion, childbirth, probing, diagnostic curettage, endometrial biopsy, vaginal examinations, feminine hygiene tampons, sexual intercourse during menstrual cycles, unnoticed cervical ruptures during childbirth.
- Suppression of the immune system, which occurs under the influence of stressful conditions, hormonal fluctuations, endocrine disorders, mental stress, allergies, and the presence of foci of chronic infection.
- The risk of developing endometritis increases in women who have had sexually transmitted diseases and inflammation in the past.
Rice. 2. The intrauterine device is one of the causes of the development of the disease.
Reasons for the development of postpartum endometritis
After delivery, the uterine mucosa does not recover immediately - it usually takes 5-6 weeks. During this time, opportunistic microflora from the vagina, as well as many other infectious agents: staphylococci, gonococci, mycoplasmas, enterobacteria, can enter the damaged endometrium through the ascending route. They become the source of an acute inflammatory process. Less commonly, microorganisms enter the uterine cavity from foci of chronic infection in the body through the blood and lymph flow, for example, with pyelonephritis, which worsens during pregnancy.
The following categories of women are especially vulnerable:
- Postpartum women with reduced immune resistance;
- Those who gave birth at a young age;
- Patients with chronic diseases of the genitourinary system, especially if they recur in the third trimester of pregnancy;
- Patients with endocrine disorders;
- Suffering from immunodeficiencies and autoimmune diseases;
- Postpartum women susceptible to anemia;
- Mothers belonging to low-income segments of the population and having a low social level: unbalanced diet and unhealthy habits;
- Postpartum women with a history of abortion, curettage, as well as a long history of using intrauterine contraceptives.
It is also worth highlighting the features of pregnancy and childbirth, which can aggravate the condition of the endometrium and cause inflammatory processes:
- Low localization and placenta previa;
- Suturing the cervix, installing an obstetric pessary;
- Invasive screening procedures (amnio- and cordocentesis, chorionic villus biopsy);
- Severe anemia and gestosis;
- Late rupture of fetal membranes;
- Prolonged attempts;
- Untimely discharge of amniotic fluid and a long anhydrous period (more than 12 hours);
- Polyhydramnios and multiple pregnancies, leading to overstretching of the uterus;
- Intrauterine monitoring during labor and multiple vaginal examinations;
- Chorioamnionitis (polymicrobial infection of the membranes and amniotic fluid);
- Injury to the perineum;
- Manual separation of placenta;
- Pathological blood loss or its uncompensated replacement;
- Intrauterine infections in a newborn (pneumonia, blood poisoning);
- Insufficient genital hygiene after childbirth.
How does acute endometritis develop?
Endometritis develops when infection enters the uterine cavity. First, the inner (basal) layer of the endometrium is affected. When the infection spreads through the lymphatic tract, it develops through damage to the muscle layer (metritis or metroendometritis). When an anaerobic infection occurs in the myometrium, necrotic processes develop, in which the mucous membrane is rejected, liquid purulent-bloody leucorrhoea and even bleeding appear.
Rice. 3. Schematic representation of the female genital organs.
Classification
The differentiation of pathology forms is carried out on various grounds. The most general one is given in the International Classification of Diseases, in which postpartum endometritis is distinguished by:
- the nature of the course of labor: independent or by caesarean section;
- clinical course: mild, moderate and severe;
- clinical manifestations: classic or erased form.
In clinical practice, a more expanded classification is used, in which forms of the disease are distinguished based on the severity of compensatory reactions on the part of the body’s defenses. According to this basis, postpartum endometritis can be:
- compensated;
- subcompensated;
- decompensated.
In the compensated form of the disease, the inflammatory process is localized inside the uterus, while the symptoms of endometritis are mild - patients only sometimes notice a slight increase in temperature. The main symptom in this case is that the uterus does not decrease in size after childbirth.
The subcompensated form is characterized by more pronounced symptoms of inflammation: the temperature rises, which is not reduced by anti-inflammatory drugs, and immune reactions appear.
Decompensated postpartum endometritis, in turn, is divided into the following clinical forms:
- purulent-catarrhal, in which inflammation passes from the uterine cavity to its appendages and nearby tissues;
- after a caesarean section;
- purulent, which develops against the background of reduced immunity in the presence of infectious agents in the body;
- protracted, characterized by erased symptoms and duration of course.
The most dangerous is the decompensated type of the disease, since it can lead to peritonitis and general blood poisoning.
Signs and symptoms of acute endometritis
Young women are more likely to suffer from endometritis. Severe disease is recorded in 60 - 80% of cases. Endometritis according to its clinical course is divided into acute, subacute and chronic.
The first signs of the disease are recorded, as a rule, 3–4 days after infection. The acute phase lasts about 7 - 10 days.
The main symptoms of acute endometritis:
- Body temperature rises from subfebrile to febrile, reaching 38 - 390C. The pulse rate increases. Chills are possible.
- The pain in the lower abdomen is severe, radiating to the groin and sacrum. Dyspareunia (pain during sexual intercourse) is noted.
- Discharge from the uterine cavity is initially serous, then serous-purulent. When infected with E. coli they have an unpleasant odor. In older women, pyometra is observed - an accumulation of pus in the uterine cavity.
- One of the main symptoms of endometritis is spotting from the uterine cavity and uterine bleeding not associated with menstrual cycles. With gonorrheal infection, the disease begins immediately with bleeding and proceeds like a long menstruation. Bleeding often occurs a few days after the end of the monthly cycle. Severe bleeding occurs when residual fragments of the fertilized egg are retained in the uterine cavity.
- Urinary dysfunction.
- Soreness of the uterus on palpation.
With timely and adequate treatment, the prognosis is favorable. Less common is the transition of the inflammatory process into subacute and chronic forms. Sometimes, with self-treatment and indiscriminate use of antibiotics, the inflammatory process takes an easier abortive treatment.
Treatment with folk remedies
Traditional medicine presents many recipes for the treatment of endometritis. However, none of them guarantees complete healing. For mild cases, you can practice douching with infusions of medicinal herbs. To do this, marshmallow root, oak bark, and cuffs are mixed in equal proportions. Then the mixture is poured with 200 ml of boiling water and infused for an hour. The herbs listed can relieve pain and reduce the manifestations of the inflammatory process.
Still, it is better to seek help from a qualified specialist and not self-medicate. After all, timely and correct treatment is the key to a quick recovery and prevention of complications of the disease.
Signs and symptoms of subacute endometritis
In the subacute course, the inflammatory process is mild. Most often, the disease occurs in individuals with reduced body resistance. The first signs of the disease are recorded 2 or more weeks after infection. Such patients seek medical help late, which affects the recovery time and the incidence of complications.
The first symptoms of subacute endometritis include weakness and low-grade body temperature. The pain is mostly aching in nature. Vaginal discharge is scanty. Trouble is indicated by spotting and bleeding from the uterine cavity. Disruptions in the menstrual cycle are often observed: brownish-colored discharge during the intermonth period and a small amount of blood during the monthly cycle. In advanced cases, monthly cycles stop completely.
About postpartum endometritis, read the article “Postpartum endometritis”
What is it: endometritis after childbirth?
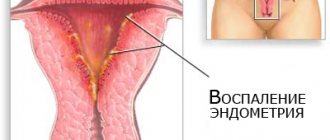
Endometritis is an inflammatory process that is characteristic of the inner layer of the uterus - the endometrium. Women encounter this disease as a result of intrauterine examinations, artificial termination of pregnancy, but most often new mothers suffer from it immediately after childbirth. Postpartum endometritis can negatively affect subsequent pregnancies. After all, while carrying a baby, it is very important that the work of the uterine mucosa is complete.
Throughout the menstrual cycle, the endometrium changes its structure to create favorable conditions for the implantation of a fertilized egg. If pregnancy does not occur, then the inner mucous membrane of the uterus begins to be rejected. As a result, women experience bleeding every month.
Inflammation of the uterus after childbirth disrupts all processes occurring in it in a healthy state. Subsequently, women face various kinds of complications: both when trying to conceive and while carrying a baby.
According to statistics, after a natural birth, 2-5% of women in labor encounter endometritis; the likelihood of uterine inflammation during a cesarean section is slightly higher and amounts to 10-20%. This disease has ICD code 10 - 086 Other postpartum infections
.
Chronic endometritis
As a result of long-term persistence of the infectious agent in the endometrium, multiple secondary morphological and functional changes develop, resulting in disruption of the cyclic transformation and reception of mucosal cells.
Most often, the disease develops after untreated acute inflammation. In half of the cases, women have a history of invasive interventions on the pelvic organs, including in the uterine cavity. It is noted that chronic endometritis is often combined with chronic inflammation of the fallopian tubes and ovaries, as well as with adhesions in the pelvis.
The disease is asymptomatic or low-symptomatic for a long time, which causes patients to seek medical help later. Clinical manifestations of chronic endometritis are associated with the depth of morphological changes in the area of inflammation and their duration. Symptoms of the disease are:
- Pain that appears before and after menstruation.
- Pain that occurs during sexual intercourse, urination and bowel movements.
- Lengthening or shortening of monthly cycles.
- Increased intensity of bleeding during menstruation.
- The appearance of spotting a week before and after menstruation.
- Changing the color of the discharge.
The development of the disease is indicated by spontaneous abortions, the inability to conceive a child, and hormonal imbalances.
On palpation, compaction of the uterus is noted. Ultrasound shows thinning of the endometrium. In areas of inflammation, the mucous membrane is replaced by connective tissue structures. The body of the uterus increases due to the accumulation of exudate in its cavity.
For more information about chronic endometritis, read the article “Chronic endometritis”
Rice. 4. The photo shows chronic endometritis.
What kind of phenomenon?
This is not a disease, it is a consequence of a pathological process in the main reproductive organ of the uterus. This phenomenon itself represents the localization of calcium salts in a certain uterine area. Note that calcifications can occur not only in this organ, but also in other organs, for example, in the liver. Thus, calcification is not only a gynecological disease, it is a pathological process that occurs due to disruption of the normal functioning of a specific organ.
Such formations are clearly visible during ultrasound and MRI. But during an ultrasound, the tissues that make up the formation are not visible, so the presence of calcification can only be assumed. This situation requires additional examination of the woman in order to exclude diseases much more serious than the presence of calcium salt deposits.
Calcification on ultrasound
Complications
Endometritis not only leads to loss of ability to work, but also often deprives a woman of the happiness of motherhood due to the development of primary and secondary infertility associated with the appearance of adhesions and obliteration of the fallopian tubes.
Previous endometritis is often the cause of chronic pain in the pelvic area, the development of ectopic pregnancy, and impaired uteroplacental circulation. The likelihood of spontaneous miscarriages and premature births increases. Infection of the fetus often develops.
If the infection spreads, parametric phlegmon, peritonitis, and pelvic abscess may develop. Cases of septic pelvic thrombophlebitis have been reported.
In the absence of timely treatment, the chance of developing serious complications increases.
Surgical delivery
It has been proven that cesarean section increases the risk of inflammatory processes compared to natural childbirth. Of no small importance is the preparedness for the operation, or, on the contrary, the urgency of its implementation.
According to statistics, with emergency surgical delivery, the morbidity rate increases to 22 - 85%.
Due to tissue inflammation, the healing of the incision slows down, the scar swells greatly, and natural cleansing is disrupted, which leads to the emergence of a source of infection. The disease develops 1-2 days after surgery, very rarely - on 5-6 days. This situation, especially with insufficient a/b therapy, carries the threat of adnexitis, parametritis, peritonitis and suture dehiscence.
Diagnostics
Diagnosis of acute endometritis is based on the patient’s complaints, medical history, data from objective, laboratory and instrumental research methods:
- Gynecological examination through the vagina and rectum.
- General blood analysis.
- Microscopy of vaginal discharge.
- Bacteriological study followed by determination of the sensitivity of microorganisms to antibiotics.
- PCR diagnostics and ELISA are effective in detecting sexually transmitted diseases.
- Using ultrasound, it is possible to determine accumulations of pus and fluid in the uterine cavity, the condition of the endometrium and myometrium.
- If necessary, sexual partners are examined.
How it manifests itself
Symptoms of postpartum endometritis depend on the type. Symptoms of acute endometritis:
- a sharp increase in temperature;
- a painful sensation occurs in the lower abdomen, the pain radiates to the sacrum;
- the presence of bloody-purulent, serous-purulent, serous discharge from the vagina;
- there is a feeling of malaise, headaches.
Close attention should be paid to the discharge. During the postpartum period, heavy bleeding occurs for several days. Afterwards they become scarcer and acquire brown and yellow shades. In a month and a half they should stop altogether. While during illness, they flow profusely, with blood, for a long period. Sometimes they are greenish in color.
Characteristic signs of chronic endometritis after childbirth:
- high temperature that does not subside;
- irregular uterine bleeding;
- discharge with a strong unpleasant odor;
- pain during bowel movements.
Causes and factors of the occurrence and development of postpartum endometritis
The structure of the endometrium combines two layers of mucosa: basal and functional. The latter, as mentioned above, is rejected at the end of each menstrual cycle. The basal layer subsequently forms a new functional layer. It is damage to this structure that can become the primary source of the inflammatory process. However, it is worth noting that endometritis does not occur after injuries to the mucosa, which is typical during labor, but due to the penetration of pathogenic bacteria and viruses into the structure of the inner layer of the uterus. The causative agents of the disease are most often: • Proteus; • Escherichia coli; • Klebsiella; • enterobacter; • chlamydia; • tuberculosis microbacteria; • mycoplasma; • diphtheria bacillus; • group B streptococci. A significant role in the manifestation of the inflammatory process of the uterus is given to the immunological defense of the body. At the end of the third trimester of pregnancy, this function loses its ability and resumes only 5-10 days (depending on the type of delivery) after birth. The likelihood of developing endometritis after childbirth is increased by: 1) concomitant diseases of the body; 2) failure to comply with hygiene rules; 3) the presence of chronic foci of infection; 4) use of intrauterine contraception before pregnancy; 5) acute infectious diseases suffered during pregnancy; 6) remains of the placental placenta in the uterus; 7) invasive (intrauterine) diagnostic methods during pregnancy, etc. Endometritis can also occur during childbirth. In this case, the development of inflammation can be provoked by: an anhydrous period of up to 12 hours, pathological blood loss, manual separation of the placenta, and a cesarean section. These factors alone cannot cause the onset of endometritis, but the combination of several increases the likelihood of developing the disease several times.