The structure and purpose of the endometrium
The endometrium is basal and functional in structure. The first layer remains practically unchanged, and the second regenerates the functional layer during menstruation. If there are no pathological processes in a woman’s body, then its thickness is 1-1.5 centimeters. The functional layer of the endometrium changes regularly. Such processes are associated with the fact that during menstruation in the uterine cavity, individual sections of the walls peel off.
Damage appears during labor, during mechanical abortion or diagnostic sampling of material for histology.
The endometrium performs an extremely important function in a woman’s body and helps ensure a successful pregnancy. The fruit is attached to its walls. The embryo receives nutrients and oxygen necessary for life. Thanks to the mucous layer of the endometrium, the opposite walls of the uterus do not stick together.
Proliferation phase
The endometrium of the early stage of the proliferation phase (the fifth to seventh day) has the form of straight tubes with a small lumen; on its cross section, the contours of the glands are round or oval; the epithelium of the glands is low, prismatic, the nuclei are oval, located at the base of the cells, intensely colored; The surface of the mucosa is lined with cuboidal epithelium. The stroma includes spindle-shaped cells with large nuclei. But the spiral arteries are weakly tortuous.
In the middle stage (eighth to tenth day), the surface of the mucosa is lined with high prismatic epithelium. The glands are slightly convoluted. There are many mitoses in the nuclei. A mucus border may appear at the apical edge of certain cells. The stroma is edematous and loosened.
In the late stage (eleventh to fourteenth day), the glands acquire a tortuous outline. Their lumen is already expanded, the nuclei are located at different levels. In the basal part of some cells, small vacuoles that contain glycogen begin to appear. The stroma is juicy, its nuclei increase, are colored and rounded with less intensity. The vessels become convoluted.
The described changes are characteristic of the normal menstrual cycle; they can be observed in pathology
- during the second half of the monthly cycle with an anovulatory cycle;
- with dysfunctional uterine bleeding due to anovulatory processes;
- in the case of glandular hyperplasia - in different parts of the endometrium.
When tangles of spiral vessels are detected in the functional layer of the endometrium corresponding to the proliferation phase, then this indicates that the previous menstrual cycle was two-phase, and during the next menstruation the process of rejection of the entire functional layer did not occur, it only underwent reverse development.
Women's menstrual cycle
Changes occur in the female body every month that help create optimal conditions for conceiving and bearing a child. The period between them is called the menstrual cycle. On average, its duration is 20-30 days. The beginning of the cycle is the first day of menstruation. At the same time, the endometrium is renewed and cleansed.
If women experience abnormalities during the menstrual cycle, this indicates serious disorders in the body. The cycle is divided into several phases:
- proliferation;
- secretion;
- menstruation.
Proliferation refers to the processes of reproduction and cell division that contribute to the growth of internal tissues of the body. During the proliferation of the endometrium, normal cells begin to divide in the mucous membrane of the uterine cavity. Such changes may occur during menstruation or have a pathological origin.
The duration of proliferation is on average up to two weeks. In a woman’s body, estrogen begins to increase rapidly, which is produced by an already mature follicle. This phase can be divided into early, middle and late stages. At an early stage (5-7 days) in the uterine cavity, the surface of the endometrium is covered with epithelial cells, which have a cylindrical shape. In this case, the blood arteries remain unchanged.
The middle stage (8-10 days) is characterized by the covering of the plane of the mucous membrane with epithelial cells, which have a prismatic appearance. The glands are distinguished by a slightly convoluted shape, and the nucleus has a less intense shade and increases in size. A huge number of cells appear in the uterine cavity, which arose as a result of division. The stroma becomes swollen and quite loose.
The late stage (11-15 days) is characterized by a single-layer epithelium, which has many rows. The gland becomes tortuous, and the nuclei are located at different levels. Some cells contain small vacuoles that contain glycogen. The vessels have a tortuous shape, the cell nuclei gradually acquire a rounded shape and greatly increase in size. The stroma becomes engorged.
The endometrium of the secretory type uterus can be divided into several stages:
- early (15-18 days of the menstrual cycle);
- medium (20-23 days, pronounced secretion is observed in the body);
- late (24-27 days, secretion gradually fades away in the uterine cavity).
The menstrual phase can be divided into several periods:
- Desquamation. This phase occurs from day 28 to day 2 of the menstrual cycle and occurs when fertilization has not occurred in the uterine cavity.
- Regeneration. This phase lasts from the third to fourth day. It begins before the complete separation of the functional layer of the endometrium along with the beginning of the growth of epithelial cells.
Content
Today, one of the most common tests in the field of functional diagnostics is histological examination of endometrial scraping. To carry out functional diagnostics, the so-called “line scraping” is often used, which involves taking a small strip of the endometrium using a small curette. The entire female menstrual cycle is divided into three phases: proliferation, secretion, bleeding. In addition, the phases of proliferation and secretion are divided into early, middle, and late; and the bleeding phase - for desquamation, as well as regeneration. Based on this study, we can say that the endometrium corresponds to the proliferation phase or some other phase.
When assessing the changes that occur in the endometrium, one should take into account the duration of the cycle, its main clinical manifestations (the absence or presence of postmenstrual or premenstrual blood discharge, the duration of menstrual bleeding, the amount of blood loss, etc.).
Normal structure
Hysteroscopy helps the doctor examine the uterine cavity to assess the structure of the glands, new blood vessels and determine the thickness of the endometrial cell layer.
If the study is carried out at different phases of the menstrual cycle, the test result will be different. For example, towards the end of the proliferation period, the basal layer begins to increase, and therefore does not respond to any hormonal influences. At the very beginning of the cycle, the internal mucous cavity of the uterus has a pinkish tint, a smooth surface and small areas of the functional layer that has not completely separated.
At the next stage, a proliferative type of endometrium begins to grow in a woman’s body, which is associated with cell division. Blood vessels are located in folds and arise as a result of uneven thickening of the endometrial layer. If there are no pathological changes in the woman’s body, then the functional layer should be completely rejected.
Premenopause
Since the volume of this layer and the intensity of its renewal directly depend on the hormonal status of the patient, normally the size of the endometrium differs in premenopause. That is, when hormonal status changes.
Endometrial thickness in hyperplasia and normal in premenopause
| Stage | Standard in mm | Pathology |
| Days of menstruation | No more than 4 (rarely 5, at the very beginning of perimenopause) | More than 5 at the end of perimenopause and more than 7 at the beginning |
| Beginning of the proliferative stage | No more than 7 | More than 8-9 in the middle of perimenopause (a little more at the beginning, and a little less at the end) |
| End of the proliferative stage | No more than 11 | More than 12 |
| Secretory stage | No more than 16 | 17 or more |
Endometrial thickness alone does not make a diagnosis of hyperplasia. However, its size plays a significant role in diagnosis, as it helps determine the necessary studies.
Forms of deviation
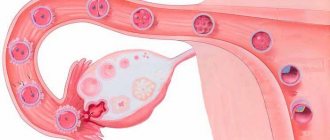
Any deviations in endometrial thickness arise as a result of functional causes or pathological changes. Functional disorders appear in the early stages of pregnancy or a week after fertilization of the egg. In the uterine cavity, the baby's place gradually thickens.
Pathological processes arise as a result of chaotic division of healthy cells, which form excess soft tissue. In this case, neoplasms and malignant tumors form in the body of the uterus. These changes most often occur as a result of hormonal imbalance due to endometrial hyperplasia. Hyperplasia comes in several forms.
- Glandular. In this case, there is no clear separation between the basal and functional layers. The number of glands increases.
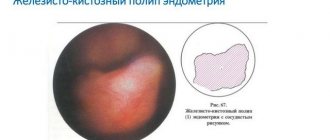
- Glandular-cystic form. A certain part of the glands forms a cyst.
- Focal. In the uterine cavity, epithelial tissue begins to grow and numerous polyps form.
- Atypical. In a woman’s body, the structure of the endometrium changes and the number of connective cells decreases.
The endometrium of the uterus of the secretory type appears in the second phase of the menstrual cycle; in case of conception, it helps the fertilized egg attach to the wall of the uterus.
Treatment
Treatment is carried out in two ways:
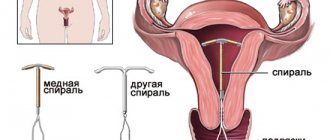
- Conservative treatment involves the use of drugs to normalize hormonal levels. Combined oral contraceptives, gonadotropin-releasing factor antagonists, and gestagens are used;
- Surgical treatment involves laser or electrical cauterization, and in rare cases, amputation of the uterus.
More information about approaches to therapy can be found in the article “Treatment of uterine endometrial hyperplasia.”
Secretory type
During the menstrual cycle, most of the endometrium dies, but when menstruation occurs, it is restored through cell division. After five days, the structure of the endometrium becomes renewed and is quite thin. The endometrium of the secretory type uterus has an early and late phase. It has the ability to grow and with the onset of menstruation it increases several times. In the first stage, the inner lining of the uterus is covered with cylindrical low epithelium, which has tubular glands. In the second cycle, the endometrium of the secretory type uterus is covered with a thick layer of epithelium. The glands in it begin to lengthen and take on a wavy shape.
In the secretory stage, the endometrium changes its original shape and increases significantly in size. The structure of the mucous membrane becomes saccular, glandular cells appear through which mucus is secreted. The secretory endometrium is characterized by a dense and smooth surface with a basal layer. However, he does not show activity. The secretory type of endometrium coincides with the period of formation and further development of follicles.
Glycogen gradually accumulates in the stromal cells, and a certain part of them is transformed into decidual cells. At the end of the period, the corpus luteum begins to involute, and progesterone stops working. In the secretory phase of the endometrium, glandular and glandular-cystic hyperplasia can develop.
Types of chronic endometritis
According to morphological characteristics, chronic endometritis is divided into 3 types:
— Atrophic endometritis
(glands atrophy, stromal fibrosis occurs, it is infiltrated with lymphoid elements).
— Cystic endometritis.
It develops when the ducts of the glands are compressed by fibrous tissue. The contents of the glands begin to thicken, which leads to the formation of cystic formations.
— Hypertrophic endometritis.
This variant of the disease is associated with hyperplasia of the mucous membrane.
Causes of glandular cystic hyperplasia
Glandular cystic hyperplasia occurs in women of all ages. In most cases, formations occur in the secretory type of endometrium during the period of hormonal changes.
Congenital causes of glandular cystic hyperplasia include:
- hereditary genetic abnormalities;
- hormonal imbalance during puberty in adolescents.
Acquired pathologies include:
- problems of hormonal dependence - endometriosis and mastopathy;
- inflammatory processes in the genital organs;
- infectious pathologies in the pelvic organs;
- gynecological manipulations;
- curettage or abortion;
- disturbances in the proper functioning of the endocrine system;
- excess body weight;
- polycystic ovary syndrome;
- arterial hypertension;
- depressed function of the liver, mammary gland and adrenal glands.
If one of the women in the family was diagnosed with glandular cystic endometrial hyperplasia, then other girls need to be especially careful about their health. It is important to regularly come for a preventive examination to a gynecologist, who can promptly identify possible deviations or pathological disorders in the uterine cavity.
Secretion phase
During the early stage of the secretion phase (fifteenth to eighteenth day), subnuclear vacuolization is detected in the epithelium of the glands; vacuoles push the nucleus into the central sections of the cell; the nuclei are located on the same level; The vacuoles contain glycogen particles. The lumens of the glands are dilated; traces of secretion may already be revealed in them. The endometrial stroma is juicy and loose. The vessels become even more tortuosity. A similar structure of the endometrium is usually found with the following hormonal disorders:
- in case of defective corpus luteum at the end of the monthly cycle;
- in case of delayed onset of ovulation;
- in the case of cyclic bleeding that occurs due to the death of the corpus luteum, which has not reached its prime stage;
- in the case of acyclic bleeding, which is caused by the early death of the still defective corpus luteum.
During the middle stage of the secretion phase (nineteenth to twenty-third day), the lumens of the glands are expanded and their walls are folded. Epithelial cells are low, filled with secretion, which is separated into the lumen of the gland. A decidua-like reaction begins to appear in the stroma during the twenty-first to twenty-second day. The spiral arteries are sharply tortuous and form tangles, which is one of the most reliable signs of an absolutely complete luteal phase. This endometrial structure can be observed:
- with increased prolonged function of the corpus luteum;
- due to taking large doses of progesterone;
- during early intrauterine pregnancy;
- in case of progressive ectopic pregnancy.
During the late stage of the secretion phase (twenty-fourth to twenty-seventh day), due to regression of the corpus luteum, the juiciness of the tissue is minimized; the height of the functional layer decreases. The folding of the glands increases, obtaining a sawtooth shape. There is a secret in the lumen of the glands. The stroma has an intensely expressed perivascular decidua-like reaction. Spiral vessels form coils that are closely adjacent to each other. On the twenty-sixth to twenty-seventh days, the venous vessels are filled with blood with the appearance of blood clots. Infiltration of leukocytes appears in the stroma of the compact layer; Focal hemorrhages appear and increase, as well as areas of edema. This condition must be differentiated from endometritis, when the cellular infiltrate is located mainly around the glands and vessels.
Clinical manifestations
Glandular cystic hyperplasia, which forms in the secretory endometrium, is manifested by the following symptoms.
- Menstrual irregularities. Spotting between periods.
- The discharge is not profuse, but with bloody, dense clots. With prolonged blood loss, patients may experience anemia.
- Pain and discomfort in the lower abdomen.
- Lack of ovulation.
Pathological changes can be determined at the next preventive examination by a gynecologist. Glandular cystic hyperplasia of the secretory endometrium does not resolve on its own, so it is important to seek help from a qualified doctor in a timely manner. Only after a comprehensive diagnosis will a specialist be able to prescribe therapeutic treatment.
Postmenopause
At this stage, menstruation stops. There is no longer a menstrual cycle, which means the endometrium is no longer renewed. Its thickness no longer changes much; it becomes more or less stable. In deep postmenopause, the size of this layer is generally stable.
On ultrasound
The diagnosis of hyperplasia can be made much easier. If the size of this layer exceeds 11 mm, then diagnostic curettage of the endometrium is necessary.
Diagnostic methods
Glandular cystic hyperplasia of the secretory endometrium can be diagnosed using the following diagnostic methods.
- Diagnostic examination by a gynecologist.
- Analysis of the patient’s medical history, as well as determination of hereditary factors.
- Ultrasound examination of the uterine cavity and pelvic organs. A special sensor is inserted into the uterus, thanks to which the doctor examines and measures the endometrium of the secretory type of uterus. He also checks for polyps, cystic formations or nodules. But ultrasound does not give the most accurate result, so patients are prescribed other examination methods.
- Hysteroscopy. This examination is carried out with a special medical optical apparatus. During diagnosis, differential curettage of the secretory endometrium of the uterus is performed. The resulting sample is sent for histological examination, which will determine the presence of pathological processes and the type of hyperplasia. This technique should be carried out before the onset of menstruation. The results obtained are the most informative, so gynecologists will be able to make a correct and accurate diagnosis. With the help of hysteroscopy, it is possible not only to determine the pathology, but also to perform surgical treatment of the patient.
- Aspiration biopsy. During a gynecological examination, the doctor scrapes the secretory endometrium. The resulting material is sent for histology.
- Histological examination. This diagnostic method determines the morphology of the diagnosis, as well as the type of hyperplasia.
- Laboratory tests to determine the level of hormones in the body. If necessary, hormonal disorders are checked in the thyroid gland and adrenal glands.
Only after a thorough and comprehensive examination will the doctor be able to make the correct diagnosis and prescribe effective treatment. The gynecologist will individually select medications and their exact dosages.
Pathology
Knowledge of the normal structure of the endometrium is extremely important for determining pathological conditions of the reproductive system. The most common pathologies of the internal uterine layer:
- adenomyosis – pathological growth of the endometrium into the underlying layers;
- endometriosis - proliferation of cells of the inner layer outside the uterus;
- cancer;
- Asherman's syndrome - sclerosis of the uterine cavity due to synechiae, which begin to form when the basal layer is damaged. As the tissue heals, it is replaced by scar tissue. It is more often observed after gross manipulations - abortion, curettage, hysteroresectoscopy. With a constant inflammatory focus that melts tissue - tuberculosis, endometritis, cancer.
Unfortunately, not all women know about the normal structure of the inner layer of the uterus, which ensures the attachment of the embryo and gestation. It is important to remember that rough intervention leaves an indelible mark on the endometrium, which is not always easy to correct. The consequences of severe pathology of the basal layer, which is unable to perform its functions, can lead to infertility.
Competition "bio/mol/text"-2011
This article was submitted to the competition of popular scientific works “bio/mol/text”-2011 in the category “Best review article”.
Stem cells are already taking their place in modern clinical practice. There are proven schemes for isolating subpopulations of stem cells, culturing them, and even correcting their differentiation in a given direction. But these achievements are not enough to realize all the hopes placed on cellular technologies.
None of the currently existing sources of human stem cells or methods for obtaining them can fully meet the needs of researchers and the requirements of clinicians. The use of embryonic stem cells, in addition to an avalanche of ethical issues, carries with it a high risk of cancer complications. Obtaining adult stem cells (syn.: regional stem cells, somatic stem cells), devoid of these disadvantages, is associated with the use of invasive, traumatic, painful for the donor (often not without the risk of complications) and, most importantly, expensive. All this, of course, limits experimental research on human stem cells and slows down the introduction of cell technologies into clinical practice.
It is recommended to read other articles on stem cells: “Safe stem cells” [17], “There was a simple cell, it became a stem cell” [18], “A snowball of problems with pluripotency” [19]. - Ed.
This article proposes to consider the possibility of using the endometrium as a source of stem cells.
Comparative characteristics of stem cells of endometrial origin
Endometrial stem cells are a heterogeneous pool of progenitor cells that have all the properties necessary to be recognized as pluripotent. Their ability to form cell colonies in a culture medium, self-renewal and self-maintenance of these colonies has been proven. Their ability to differentiate into various derivatives of ecto- and mesoderm, which is most important from a practical point of view, has been determined. A complex of specific markers corresponding to the standard set of surface proteins of mesenchymal stem cells is described.
Moreover, a number of characteristics of endometrial progenitor cells distinguish them favorably from stem cells of other origins.
The source of this type of progenitor cells is undoubtedly easily accessible. Obtaining menstrual tissue for isolating stem cells does not involve traumatic procedures for the donor and can be carried out repeatedly from the same donor. Any complications associated with the collection of material were excluded. Also, the technology for obtaining stem cells from menstrual tissue requires minimal financial costs.
An important aspect for choosing the optimal source of stem cells is the number of desired cells per unit of tissue. Isolation of stem cells from other postnatal tissues is complicated by their extremely low content (less than a thousandth of a percent in the case of umbilical cord blood during full-term pregnancy). In endometrial tissue, up to 0.22% of epithelial cells and up to 1.25% of stromal cells have clonogenic potential [2].
Many researchers have noted a higher proliferation rate of stem cells of endometrial origin without reducing the life span of the colony due to increased telomerase activity [4–6].
The advantage of stem cells of endometrial origin over embryonic stem cells is obvious - in the absence of inconsistency with ethical and legislative standards, the use of adult stem cells undoubtedly has less oncogenic potential. Another positive aspect of the use of adult stem cells is the possibility of autotransplantation of cellular products obtained from them, which completely solves the immunological issues that always accompany stem cell therapy. In addition, there is evidence of the ability of mesenchymal stem cells, whose properties are also shared by endometrial stem cells, to exert antiproliferative, anti-inflammatory and immunomodulatory effects [7–9].
The most attractive property of endometrial stem cells is their plasticity. Their ability to develop in chondrogenic, adipogenic, osteogenic, cardiogenic, and neurogenic directions in vitro under the influence of environmental stimuli has been proven (Fig. 2). Not all researchers agree with the ability of somatic stem cells to change their specialization and differentiate into derivatives of other germ layers. For the practical use of this quality of stem cells, it is not so important whether the cells undergo true transdifferentiation under the influence of microenvironmental factors or this “transformation” occurs due to the heterogeneity of the stem cell culture or the fusion of stem and mature cells. One way or another, this property of endometrial stem cells sets them apart from other stem cells [4], [5], [10], [11].
Figure 2. Differentiation of endometrial-derived mesenchymal stem cells into cardiomyocytes. The immunocytochemical method detected markers of cardiomyocytes - troponin, actin and connexin 43.
[4]
Prospects
Stem cells of endometrial origin have great potential for use in studying the properties of stem cells, searching for new factors that determine the differentiation of progenitor cells, and using genetic engineering technologies to realize the required cellular properties. Their use in clinical practice for the treatment of various diseases, perhaps previously incurable, is also promising.
The high need for this type of cells may require the organization of menstrual tissue donation programs and banks of cryopreserved stem cells of endometrial origin. The possibility of autodonation may serve as an incentive for women of reproductive age to participate in such programs.