Take the first step
and make an appointment with your doctor!
After conceiving a child, multiple changes begin to occur in a woman’s body, the purpose of which is to make pregnancy and birth more likely. They manifest themselves at all levels, from the anatomy of the genital organs to metabolism and hormonal levels. One important aspect is changes in the cervix during pregnancy. A woman who does not know about them can often mistake the normal processes happening to her for pathological ones and vice versa.
Why is medical supervision needed?
It is advisable to conduct an examination of the cervical canal before conception. If it is shortened or there is another pathology, this will allow maintenance therapy to be started in advance and will minimize the likelihood of miscarriage.
Medical supervision is mandatory throughout pregnancy so that a specialist can monitor the condition of the cervix and fundus of the uterus and, if necessary, can quickly respond and select effective therapy.
Normal indicators
Until week 20, the size remains virtually unchanged, and there is no need for observation, however, further changes should be monitored. Although the length of the cervical canal is slightly different for all women, there are certain standards that allow you to control the process and make it possible to detect deviations. The normal indicators are determined based on medical research and are shown in the table below. To continue the pregnancy, if something goes wrong, urgent treatment or hospitalization may be required.
Bishop's degree of cervical maturity
Table “Cervical length during pregnancy by week”
The organ matures rapidly during the last two prenatal weeks. Its length is reduced to one centimeter, and the cervical canal, closed by a mucous plug throughout the entire gestation period to protect the fetus from various infections, opens and forms an exit from the uterus to the vagina. This is how the body should prepare for the birth process; all deviations have their own reasons and require mandatory correction.
What it is
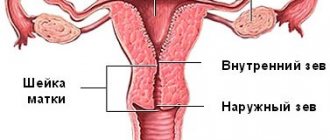
Cervix uteri is the Latin name for the cervix, the lower part of the main reproductive organ in women. The cervical canal runs inside the cervix, the lower part of the cervix enters the vagina, and the upper part communicates with the uterine cavity.
Nature has assigned important functions to this cylindrical part of the uterus.
Before pregnancy, the cervix acts as a “gatekeeper,” tightly closing the entrance to infection, microbes, and even sperm if they arrive at the wrong time. Mucus completely covers the cervical canal.
Once a month, the cervix holds an “open day” - this happens before ovulation , when under the influence of hormones the mucus becomes liquid, freeing the passage into the cervical canal for male reproductive cells.
If pregnancy occurs, the cervix again “seals” the passage with a mucous plug, reliably protecting the developing embryo, and subsequently the fetus, from microbes, fungi, destructive microflora and anything that can harm.
In addition, the cervix is responsible for holding the baby in the uterine cavity until birth. If she is weak and unable to cope with this task, there is a real threat of termination of pregnancy.
During childbirth, the small cervix does a big job - it opens up to such a size that the baby's head can pass through it. It is through the cervical canal that the baby leaves the mother’s womb after 9 months to begin an independent life in this world.
Anatomically, the cervix is quite complex. She has a vaginal part - this is what doctors study during a routine examination using a speculum. The deeper structures are the vaginal vaults, through which the cervix connects to the uterine cavity. To examine them, a gynecological speculum alone will not be enough; a special device, a colposcope, is needed, and the examination procedure will be called colposcopy.
Diagnostic methods
The condition of the uterus and all its elements is assessed using two methods:
- When examined in a chair by a gynecologist. The doctor determines the approximate density and length of the cervix, its location in relation to the pelvic axis, and the condition of the external pharynx.
- Through ultrasound. The examination allows you to determine the structure of the external and internal pharynx and calculate the length of the lower segment.
At mid-term, the fetus begins to grow faster, which puts more strain on the muscles, so regular examinations become especially important. Also at this stage, a second screening ultrasound is performed, in which special attention is paid to the cervical canal. If there is a suspicion that it is shortened, a transvaginal examination is auxiliary, which involves inserting a sensor into the vagina, making it possible to measure the length more accurately.
How to measure and why
To successfully carry a pregnancy, women must regularly go for examinations with gynecologists. Specialists can determine the size of the cervix in the following ways:
- Manual. The patient sits on the gynecological chair. The doctor assesses the structure of the organ and its length through palpation. Normally, the following results should be observed: the external pharynx is closed, dense structure, length 3.5 cm.
- Hardware. The cervix is measured and its condition is assessed during an ultrasound examination with a vaginal probe. The doctor, thanks to highly sensitive equipment, is able to determine the size with an accuracy of a millimeter. From the 20th week, this data can be obtained by undergoing an ultrasound with a transabdomial sensor.
Shortened cervix
This deviation is dangerous, as it not only threatens the normal course of pregnancy, but can also provoke a miscarriage.
Causes and consequences
Factors that can cause excessive shortening in the early stages include:
- anatomical and physiological characteristics of the body as such and the reproductive system in particular;
- scars left after an abortion or other surgical interventions, or as a result of muscle rupture during a previous birth;
- pelvic diseases of an inflammatory nature;
- infections suffered during pregnancy;
- complications caused by bleeding;
- progesterone deficiency and other hormonal disorders;
- psychogenic factors such as stress and fear.
IMPORTANT! Most often, shortening of the organ indicates isthmic-cervical insufficiency. Its danger lies in the fact that the cervix with this pathology cannot hold the child in the uterine cavity: it opens prematurely, unable to withstand the load, which entails premature birth.
Symptoms of ICN
The diagnosis of isthmic-cervical insufficiency is determined on the basis of medical studies, however, there are signs by which a pregnant woman can identify a possible problem before undergoing an ultrasound. The pathology is often accompanied by bursting pain in the vagina, which also spreads to the lumbar region and groin.
However, you cannot rely only on the absence or presence of pain. The course of ICI can be asymptomatic, and the woman will not feel anything suspicious until the very moment when it is no longer possible to save the situation. This is why observation by a gynecologist is necessary.
Treatment
What therapeutic measures need to be taken in each specific case is decided by the doctor, based on the cause of the pathology. So, the following can be used:
- Hormonal drugs. They are prescribed in cases where INC is caused by endocrine disorders and restoration of hormonal levels can still return the size of the organ to normal.
- Installation of a pessary. It is a ring made of silicone or plastic and is installed directly in front of the canal through the vagina. The procedure takes only a few minutes and does not require painkillers. The pessary supports and is used in combination with medications. A pregnant woman with an obstetric pessary should remain in bed most of the time and avoid any stress to ensure that the device does not become dislodged and performs its function properly.
- Cervical cerclage. This procedure is also known under a simpler name, which immediately reveals its essence - suturing the cervix. There are two main methods by which cerclage can be performed: Shirodkar and MacDonald. The latter involves the application of temporary circular sutures, which temporarily narrow the canal and are removed at approximately 37 weeks of pregnancy. If cerclage is carried out according to the first method, then the suture will be permanent, and childbirth will require a cesarean section. Being a surgical intervention, cerclage is performed under anesthesia - epidural or spinal, less often general.
Regardless of what kind of treatment was prescribed, constant medical supervision is a prerequisite for therapy. The specialist must keep the process under control in order to correct it in time if necessary.
Medical supervision is especially important in the first time after cerclage has been performed, since the procedure is associated with certain risks. To make sure that the surgical intervention does not provoke premature onset of labor, doctors monitor the pregnant woman’s condition for several hours. During the first week, it is advisable to move as little as possible and observe bed rest, and you also need to mentally prepare for the fact that after suturing, cramps and minor bleeding are possible for several days.
Deviations
Congenital features or diseases of the cervix can complicate pregnancy and childbirth. Let's look at the most common problems.
Isthmic-cervical insufficiency during pregnancy
This condition is considered a pathology when carrying a baby and often leads to miscarriage or premature birth, since the cervix cannot cope with the load and cannot hold the fetus in the uterus for the required period.
In fact, the cervix consists of muscle and connective tissue that form a kind of sphincter (muscle ring) in the area of its internal os, the purpose of which is to retain the resulting fertilized egg for 9 months.
The reasons that this ring ceases to perform its natural function can be different, based on them, the pathology is divided into two types.
Insufficiency of traumatic type
It occurs after various gynecological interventions performed before, associated with forced expansion of the ring, for example, during research or abortion, as well as damage to the integrity of the muscles of this area during natural childbirth.
With any muscle rupture in this area, a scar is formed at the site of damage, in which muscle tissue is replaced by ordinary connective tissue, thereby disrupting the further ability of muscle stretching and contraction. The same applies to the cervix itself as a whole.
Functional type deficiency
This disorder in most cases occurs when there are hormonal imbalances in a woman’s body. Most often, with such deficiency, there is either an excess of androgen or a deficiency of progesterone.
In this case, ICI appears during pregnancy from 11 to 27 weeks, most often from 16 to 26 weeks. At this time, the developing fetus’s own adrenal glands begin to work, producing additional hormones, which include androgens.
If a woman’s level of this hormone is already elevated or she is sensitive to androgens, then with additional supply from the fetus, the cervix begins to quickly soften and shorten, preparing for the birth of the baby, after which dilation occurs.
As a rule, there are no special signs of this condition, and the tone of the uterus with the functional form of ICI may not change.
If a woman does not attend routine medical examinations, she may not know that she has such a problem until the very moment of premature labor, when it will no longer be possible to provide the necessary assistance to maintain the pregnancy.
In the presence of ICN, it is especially important to maintain hygiene in order to avoid the occurrence of an inflammatory process in the vagina, since through a slightly open cervix, harmful bacteria can enter the fertilized egg, infecting it, which causes a loss of strength of the membranes and leads to their rupture.
In this case, the woman’s water breaks quickly and painlessly without any special symptoms, and a miscarriage occurs.
Endocervicitis of the cervix
Any woman between the ages of 20 and 40 can become infected with this disease; the infection can spread not only through unprotected sex, but also when visiting public places such as saunas, solariums, swimming pools, and gyms.
It is important to be regularly examined by a gynecologist as a preventive measure for the occurrence of such a disease, and this applies not only to pregnant women or those planning to become a mother.
If endocervicitis is not detected in a timely manner and there is no treatment, the disease can lead not only to infertility, but also to the appearance of oncology of the internal genital organs.
Cervical erosion during pregnancy
Erosion is called damage to the mucous membranes of the vagina, with the replacement of normal epithelial cells by cylindrical ones, which are the epithelium of the cervical canal. This problem is common among expectant mothers, but it does not have any effect on the condition of the woman, the fetus, or the process of childbirth.
Erosion looks like a red spot located on the cervix with virtually no symptoms, so most women can only find out about the presence of such a problem when examined by a gynecologist.
Sometimes women with erosion may experience bloody vaginal discharge or experience pain during sexual intercourse.
Most often, this problem occurs in nulliparous women. Erosion can appear for various reasons, the main one of which is hormonal instability, since the columnar cells of the cervical epithelium are very sensitive to any fluctuations in hormones.
Erosion often results from taking hormonal contraceptives, in particular pills, or using chemical contraceptives (suppositories, sponges, rings). In addition, mechanical damage to the mucous membranes, as well as chemical irritation, is a common cause.
Cervical erosion cannot cause any complications in a pregnant woman, nor can it create complications during childbirth, so treatment is not carried out during pregnancy. The violation is cauterized only after childbirth if the erosion does not go away on its own by this time.
Elongated cervix
Not only a short, but also a long neck is possible. This situation may be due to the following reasons:
- atypical structure of the patient’s organ;
- previous operations;
- an unformed or disturbed generic dominant, which manifests itself in a depressed state of mind, fear of the upcoming birth.
The elongated canal does not affect the course of pregnancy at all and does not pose a danger to the development of the fetus, but it can complicate the birth itself. The long neck usually has a compacted structure - obstetricians sometimes call it “oak” - and does not open well during contractions, and in some cases does not open at all, which will require an emergency caesarean section.
In order for the birth to take place naturally and without complications with an elongated organ, the woman is prescribed medications that are designed to soften and smooth out the structure. As a rule, such therapy is carried out in preparation for childbirth.
Prenatal changes
The lower segment of the uterus is a hollow ring-shaped muscle, the length of which in non-pregnant women is mainly from 4.5 to 3 cm. During pregnancy, it gradually contracts, this process begins to take place actively from the 37th week (the rates of changes at earlier stages are shown in the table above).
The organ becomes not only shorter, but also softer and centered in relation to the pelvis. The period during which these changes occur varies depending on the characteristics of the reproductive system of the woman in labor. So, in some women, the cervix smoothes out to the final state (1-1.5 cm) and opens properly over several days or even weeks, while in others this process takes place within a day or just a couple of hours before the onset of contractions.
Whether a woman gives birth for the first time or the second time does not have much influence on the course of changes. The process sometimes differs only in that in pregnant women who have given birth before, the contraction during the early stages will be less pronounced, but will pass quickly immediately before childbirth.
From the moment of conception to childbirth, the cervix undergoes various changes, the most important of which is shortening in length. This indicator affects whether the expectant mother will be able to carry the child for the entire prescribed period or not, and deviations from the norm are fraught with such serious consequences as miscarriage and premature onset of labor.
A short cervical canal, however, is not a categorical contraindication to motherhood, and the negative impact of the pathology can be balanced by various therapeutic measures, in particular the use of a pessary or cerclage. In order to identify the problem in time and eliminate it, you need to be observed by a gynecologist and take his recommendations responsibly.
Useful video: common questions during pregnancy
List of sources:
- Savitsky G. A. Biomechanics of cervical dilatation during childbirth. St. Petersburg: ELBI, 1999. 114 p.
- Tokhiyan A. A. Features of labor depending on the “maturity” of the cervix and the content of estrogen and progesterone in the blood plasma: abstract. dis…. can. medical sciences, M., 1979. 13 p.
- Vdovin S.V., Selikhova M.S. Modern features of uterine contraction anomalies // Vestn. Volgogr. honey. academy. Volgograd, 1996. No. 2. P. 65–67.
- Sidorova I.S. Physiology and pathology of labor. M.: MEDpress, 2000. 320 p.
Author
Irina Vaganova
Doctor
Share