Modern advances in the development of laboratory diagnostics allow the use of effective procedures for detecting diseases. One of the most important tests in gynecological practice is histological examination.
This method involves examining a section of tissue of an organ under a microscope. Histological analysis determines whether the organ tissue is normal.
Histology of the uterus is performed quite often, and the cervix, as well as the inner and middle layers of the body of the organ, are diagnosed.
Anatomy of the cervix
The cervix at one end is located in the vagina, and at the other ends it passes into the body of the uterus, located in the pelvic cavity. It is shaped like a cylinder. Inside it is the cervical canal, through which the uterus connects to the vagina.
The cervical canal has two openings:
- The external os is located in the vagina and is visible during a gynecological examination. It has a round shape in nulliparous women and becomes slit-like after childbirth.
- The internal os is the junction of the cervix and the body of the uterus. It is not visible upon inspection.
The length of the cervix in a healthy woman is 3-6 cm . This value remains virtually unchanged throughout life. During childbirth, the cervix shortens, softens and dilates up to 10 cm - so that the baby can pass through the birth canal.
The fallopian tubes
The fallopian tubes (oviducts, Fallopian tubes) are paired organs through which the egg passes from the ovaries to the uterus.
Development.
The fallopian tubes develop from the upper part of the paramesonephric ducts (Müllerian canals).
Structure.
The wall of the oviduct has three membranes:
mucous
,
muscular
and
serous
.
The mucous membrane is collected in large branched longitudinal folds. It is covered with a single-layer prismatic epithelium, which consists of two types of cells - ciliated
and
glandular
, secreting mucus. The lamina propria of the mucous membrane is composed of loose fibrous connective tissue. The muscular layer consists of an internal circular or spiral layer and an external longitudinal one. On the outside, the oviducts are covered with a serous membrane.
The distal end of the oviduct expands into a funnel and ends with a fimbriae (fimbriae). At the time of ovulation, the vessels of the fimbriae increase in volume and the funnel tightly covers the ovary. The movement of the germ cell along the oviduct is ensured not only by the movement of the cilia of the epithelial cells lining the cavity of the fallopian tube, but also by peristaltic contractions of its muscular membrane.
Histology of the cervix
The wall of the cervix contains connective tissue and muscle fibers. Muscle tissue is represented by smooth muscles that contract without conscious human participation. Most of the muscles are located in the upper part of the organ - here they form a ring. Connective tissue contains blood and lymphatic vessels.
The inner and outer parts of the cervix are lined with epithelium:
- Stratified squamous epithelium is located on the vaginal part of the cervix. It is similar in structure to skin, but does not have a stratum corneum. Sometimes the cervix becomes keratinized, and then a light spot appears on its surface. This phenomenon is called leukoplakia. During reproductive age, stratified squamous epithelium is rich in glycogen, which means favorable conditions are created for the growth of beneficial microflora. During menopause, the epithelium atrophies, its glycogen concentration decreases, and its properties change.
- Columnar epithelium lines the cervical canal. Here the mucous membrane has folds and forms transparent mucus, which forms a plug. The nature of mucus changes throughout the menstrual cycle - for example, during ovulation it becomes viscous, transparent and permeable to sperm.
Stratified squamous and columnar epithelium meet each other and form a junction line. In girls and young women, this border is located in the vaginal part of the cervix. With age, the junction line moves into the cervical canal, and by menopause it is usually not visible during examination.
This is what the epithelial junction area looks like.
The meeting point of stratified squamous and columnar epithelium is the subject of close attention of the gynecologist. This is the weakest point of the cervix - it is here that pathological processes most often arise, including malignant tumors. The junction site must be visualized during colposcopy and taking a smear for oncocytology.
Why is this so important? The thing is that the main cause of the development of dysplasia and cervical cancer is considered to be the human papillomavirus (HPV). It reproduces only in actively dividing cells, such as the basal layer of the cervical mucosa. This layer is securely hidden under other layers of squamous epithelium. The virus can reach actively dividing cells only where this layer becomes thinner - at the junction. Here the basal cells are located close to the surface and become vulnerable to HPV.
Histology.RU
Material taken from the site www.hystology.ru
The female reproductive system includes paired organs - the ovaries, fallopian tubes and unpaired organs - the uterus, vagina, genitourinary vestibule and external genitalia.
The ovary is a sex gland that performs exocrine and endocrine functions. The first comes down to the formation of eggs, or oogenesis, the second - to the cyclic secretion of female sex hormones - estrogen and progesterone.
The ovary is divided into cortex and medulla. On top, the ovary is covered with a single-layer cubic (superficial) epithelium, which is a continuation of the peritoneum. Beneath the surface epithelium lies the tunica albuginea, made of dense connective tissue. As a rule, the cortex is located on the outside, the medulla is in the center of the organ (Fig. 313). In mares, the cortex is located internally, in the ovulatory fossa, and the medulla is external.
The basis of the cortex and medulla is the connective tissue stroma. In the cortex, it consists of densely lying fibroblasts, the shape of cells and nuclei resembling smooth muscle cells. The intercellular substance contains little collagen and no elastic fibers.
Rice. 313. Schematic representation of the structure of the ovary:
1 - mesovarium; 2 - germinal epithelium; 3 - primary follicle; 4 - two-layer follicle; 5 - the beginning of the formation of the follicle cavity; 6 - atretic follicle; 7 - almost completely mature follicle; 8 - atretic follicle; 9 - mature follicle; 10 - oocyte; 11 - cavity filled with follicular fluid; 12 - ruptured follicle; 13 - released egg; 14 - developing corpus luteum; 15 - connective tissue; 16 - luteal cells; 17 - fibrin of a blood clot; 18 - clotted blood; 19 -. ovarian connective tissue; 20 - fully formed corpus luteum; 21 - whitish body of the ovary; 22 - blood vessels.
The stroma of the medulla consists of loose connective tissue with its typical structure. The medulla has abundant vascularization, and its blood vessels are characterized by a tortuous course. The connective tissue of the stroma contains interstitial cells - interstitial cells. They usually lie in groups and are similar in structure to epithelial cells. These cells are classified as glandular. Their function is associated with the synthesis of estrogen. This makes up for its deficiency in those periods of a female’s life when there are no developing follicles - at the time of development of the female’s secondary sexual characteristics, as well as in the period after ovulation.
The stroma of the ovarian cortex contains developing follicles, atretic follicles, and the corpus luteum.
In each follicle, the egg is in the growth stage, which is why it is called the primary oocyte.
On the periphery of the cortex, under the tunica albuginea, there are a large number of primordial follicles (Fig. 314). During the process of ovarian function in a sexually mature female, their number gradually decreases.
The primordial follicle consists of an egg cell covered by a single layer of squamous follicular cells.
During the development of the follicle, due to the synthesis and deposition of yolk in the cytoplasm, a gradual increase in the egg (primary oocyte) occurs. At the same time, follicular cells grow and rapidly divide. From flat they turn into cubic, and then into cylindrical; From single-layer follicular epithelium becomes multilayered. This is how a granular layer forms around the egg. The cells of the granular layer are located on a basement membrane called the vitreous membrane.
Outside the granular layer, a connective tissue membrane, or theca, is formed from the surrounding stroma.
In the zone of contact between the plasmalemma of the egg and the follicular cells of the deep layer of the granular membrane, a zona pellucida appears. It is built from outgrowths of the plasma membranes of these cells.
The inner layer of the granular membrane is represented by cells of a cylindrical shape and a radial arrangement. This layer is called the corona radiata. With the help of the thinnest outgrowths
Rice. 314. Stages of development of the oocyte and ovarian follicle of mammals:
A-D-primary follicles; D-E - secondary follicles in which a cavity has formed; 1 - radiant crown; 2 - follicle shell; 3 - granular layer; 4 - brilliant zone; 5 - oocyte; 6 - egg-bearing tubercle; 7 - follicle cavity; 8 - inner layer of the follicle shell; 9 - outer layer of the follicle shell; 10 - granular membrane; F - H - mature follicles.
Rice. 315. Mature follicle. The photograph (magnitude 840) was taken using a scanning electron microscope. In the center is a spherical oocyte surrounded by cells of the corona radiata.
The cells of the corona radiata transfer nutrients from their plasmalemma to the egg cell.
Subsequently, gaps filled with liquid appear between the cells of the granular layer. From this moment on, the follicle is called vesicular. The size of the cracks gradually increases. They connect into one cavity, which is filled with follicular fluid, pushing the egg to one of the poles of the follicle. The egg lies in a tubercle consisting of follicular cells. This tubercle is called the ovarian hillock. Located in the ovarian mound, the egg is covered with a zona pellucida, a corona radiata and a granular shell.
Such a follicle is called a mature follicle, or Graafian vesicle (Fig. 315). Its wall is built of a granular layer (follicular epithelium), a vitreous (basal) membrane, and a connective tissue theca. The theca is divided into the inner - vascular and outer - fibrous layers.
Thus, in the developing ovarian follicles of a sexually mature female, the eggs are at one of three stages of oogenesis, namely at the growth stage, the essence of which mainly comes down to the accumulation of nutritional material (large growth stage). (See chapter "General Embryology".)
The development of follicles and the restructuring of other structures of the ovary and organs of the reproductive system of the female (male) are regulated by follicle-stimulating and luteinizing hormones of the anterior lobe of the adenohypophysis; the synthesis of these hormones is associated with the secretory function of gonadotropocytes (Fig. 316).
Follicular cells in the granular layer of growing follicles produce estrogen (folliculin). It accumulates in the follicular fluid of the vesicular follicle and enters the blood. Its excess in the blood causes increased formation of luteotropic hormone, synthesized by the same cells of the pituitary gland. An excess of this hormone causes ovulation (Fig. 317) - rupture of the wall of the mature follicle and the release of the egg from the ovary and the restructuring of the cells of the granular layer of the wall of the burst Graafian vesicle into the corpus luteum. The corpus luteum is a temporary endocrine gland of the ovary that produces progesterone. Under its influence, changes occur in the uterine mucosa, aimed at
Rice. 316. Diagram illustrating the interaction between the hormones of the anterior pituitary gland and the ovary, which ensures the regulation of the main events in the reproductive cycle of mammals.
creating favorable conditions for the perception of a fertilized egg (zygote), and also inhibiting the growth of other follicles. Therefore, if the corpus luteum is actively functioning in the ovary, other follicles do not develop.
Consequently, the production of estrogen and progesterone in the ovary does not occur simultaneously, which causes cyclic changes in the structure and function of the organs of the female reproductive system.
Ovulation in animals occurs during the period of estrus, which is characteristic of the stage of initiation of the female's sexual cycle. In monoparous animals, during the period of estrus, one mature follicle ovulates; in multiparous animals, several mature follicles ovulate. In some multiparous animals (pig, rabbit), several follicles can develop in one follicle.
Rice. 317. The process of ovulation in a rabbit during slow motion filming:
A - follicles 1 ½ hours before their walls rupture; B - follicles up to ½ hour before rupture; B - release of clear liquid in the initial stage of rupture of the follicle wall; G-1 - appearance of the second follicle; G-2-bloody discharge at the late stage of follicle rupture; D - rupture of the second follicle; E - egg release (according to Carlson).
eggs, so during ovulation, several eggs enter the oviduct from one follicle at once.
The ovulated mature egg, surrounded by the zona pellucida and the corona radiata, enters the fringe of the oviduct and then into the oviduct, where it is fertilized. In place of the bursting mature follicle, the corpus luteum develops from the follicular cells of the granular layer. After the wall of the follicle ruptures, blood flows into the cavity formed as a result of the release of the egg; follicular cells multiply and fill the follicle cavity; Blood vessels from the theca vascular layer grow into a mass of dividing epithelial cells. Then these cells sharply increase in size and a yellow pigment, lutein, accumulates in them, and therefore the cells are called luteal. Luteal cells begin to produce the hormone progesterone. The connective tissue membrane (theca) of the burst Graafian vesicle grows and forms the membrane of the corpus luteum, from which layers grow into it, dividing the parenchyma into lobules.
The further fate of the corpus luteum is determined by the following. If the egg has not been fertilized, then a few days before the start of estrus it decreases in size, becomes denser and reduced, and is replaced by connective tissue. Consequently, in a non-pregnant female, the corpus luteum functions during one sexual cycle. After the start of a new sexual cycle, the corpus luteum of this cycle also develops. This corpus luteum is called the corpus luteum of the reproductive cycle. If the egg has been fertilized and pregnancy has occurred, the corpus luteum, called the corpus luteum of pregnancy, remains active in most farm animals throughout pregnancy.
The number of simultaneously developing corpora lutea is proportional to the ovulated mature follicles.
As follicles develop, not all of them reach maturity and ovulate. A significant part of the follicles die at different stages of development. This process is called atresia, and the destroyed follicles are called atretic. Atresia begins with the death of follicular cells, which lose their trophic function. This also leads to the death of the egg. The zona pellucida remains the longest in the atretic follicle. The rest of the follicle is filled with overgrown connective tissue from the theca of the follicle. When the normal course of the atresia process is disrupted, ovarian cysts are formed.
Oviduct . In the wall of the fallopian tube, or oviduct, there are mucous, muscular and serous membranes (Fig. 318).
The mucous membrane is covered with single-layer (simple) ciliated epithelium. There are two types of epithelial cells in the epithelial layer: ciliated and non-ciliated cells. The first type is columnar cells. The plasmalemma of their apical pole forms microvilli and ciliated cilia, the movement of the latter is directed towards the uterus. The second type is cubic cells. They do not have cilia and are called unciliated. These cells perform a secretory function. The ratio of different types of cells in the epithelial layer may vary depending on the period of the sexual cycle. Most of them
Rice. 318. Fallopian tube of a cow:
1 - mucous membrane; 2 - muscular layer; 3- serous membrane.
the amount is observed during the period of estrus, which is due to the preparation of the female’s reproductive tract to accept the zygote.
The main lamina consists of loose connective and reticular tissue. There are individual smooth muscle cells. The mucous membrane is characterized by uneven contours. It forms numerous longitudinal (primary and secondary) folds, in the formation of which both layers of the mucous membrane take part.
The muscle layer is made up of smooth muscle cells. It forms an intensively developed circular layer. Near the uterus, it becomes thinner and an additional layer with oblique orientation of smooth muscle cells appears.
The serosa consists of loose connective tissue and mesothelium.
In the oviduct, fertilization of the egg occurs and its advancement into the uterus. This is facilitated by the structure of the wall of the oviduct: the presence of ciliated cilia on the surface of the cells, the formation of mucus that moisturizes the surface of the mucosa, as well as contraction of the muscular layer.
Uterus. In mammals, the uterus performs a number of functions that are carried out under the influence of ovarian hormones (estrogens, progesterone) and nervous regulation. An embryo develops in the uterus. It, together with the chorion and allantois, is involved in providing the embryo with nutrients, oxygen, water and the release of metabolic products.
Contraction of the uterus causes the secretion of the uterine glands to move caudally and cleanse the female’s genital tract from infections; during pregnancy, it promotes the correct position of the fetus; during childbirth, it participates in pushing the fetus out of the uterus.
During the female’s sexual cycle, in which it is customary to distinguish between pre-estrus (proestrus), estrus (estrus), post-estrus (metaestrus), inter-estrus (diestrus) (see page 431). The structure of the uterine wall undergoes significant changes. They, caused by the entry into the blood of hormones produced by the ovary, are collectively called the uterine cycle. The wall of the uterus is made up of mucous, muscular and serous membranes.
The mucous membrane (endometrium) is covered with single-layer columnar epithelium (Fig. 319). The epithelium contains ciliated and secretory cells that secrete mucous and serous secretions. The structure of the epithelial layer in different farm animals varies and depends on the period of the reproductive cycle. Thus, in sheep and mares, unlike other animals, the epithelial layer is built from a single-layer cylindrical ciliated epithelium.
In cows, during the proestrous and estrous periods, and then in the middle of the reproductive cycle, the thickness of the epithelial layer increases, processes are formed on the surface of its cells, the nuclei are located at different levels from the basement membrane -
Rice. 319. Transverse section of the uterus:
1 - lumen of the uterus; 2 - mucous membrane; a - epithelium; b - main plate; 3 - muscular layer; c - inner annular layer; g - outer longitudinal layer; d - vascular layer; 4 - serous membrane; e - glands; 5 - middle layer of the muscular layer; 6 - blood vessel.
multirow is formed, numerous mitoses occur. These changes are consistent with cyclical changes in the blood levels of estrogen and progesterone.
The main plate is well developed. It consists of loose connective and reticular tissue with a small number of smooth muscle cells. The connective tissue of the subepithelial zone is characterized by an abundance of cellular elements and reticulin fibers. Deeper, collagen fibers with a network-like orientation acquire more intensive development. This zone is subject to the greatest cyclical changes. Then, the direction of the collagen fibers becomes radial.
The connective tissue of the main lamina is very poor in elastic fibers and they are located mainly in the walls of blood vessels.
Connective tissue cells are fibroblasts, reticular cells, numerous macrophages, monocytes, granulopites, lymphocytes, plasma cells, mast cells. The latter in the subepithelial layer can have a branched or spindle-shaped shape. In the first days of the uterine cycle, an abundance of poorly differentiated cells and mitoses were found in the stroma of the mucous membrane. Tissue swelling is observed. During the period of active secretory function of the corpus luteum, cells differentiate, swelling decreases. Then, with the development of follicles in the ovaries, cellular dedifferentiation takes place. The superficial epithelial layer sinks into the main lamina and forms simple tubular branched glands of the merocrine type. Their structure is similar to the epithelial cells covering the mucous membrane.
The secretory function of the uterine glands is variable. It sharply intensifies due to the development of the corpus luteum and weakens during the period between estrus.
A feature of the structure of the mucous membrane in ruminants is the formation of caruncles. They are formed by the main plate and at the moment of attachment of the embryo to the uterus, cotylides - chorionic villi - are introduced into them. Caruncles are characterized by abundant vascularization, and in their main plate there are groups of smooth muscle cells. There are no glands in the cervix; the epithelium contains many mucous cells; the mucous membrane forms numerous folds. The uterine mucosa lacks a muscular plate and submucosa.
The muscular layer (myometrium) is made of smooth muscle tissue. Three layers are formed from its cells: the inner layer is circular, the middle layer of obliquely oriented cells and the outer layer is longitudinal. A feature of the muscular lining of the uterus is the presence of a large number of blood vessels in the middle layer. This is the vascular layer of the muscularis propria. It is clearly expressed in small predatory animals. In cows, the vascular layer is connected to the circular muscle layer and is expressed as an independent layer only in the area of the uterine horns. In mares, the vascular layer is poorly visible, since its vessels form complex relationships with muscle elements. In pigs, large blood vessels pass mainly in the connective tissue of the main plate, so there is no vascular layer of the muscularis propria.
The degree of development of the circular and longitudinal layers of the myometrium also varies in different farm animals. This is due to the length of the uterine horns and the single pregnancy of animals. In this connection, in a cow and mare, the inner annular layer has a greater thickness, and in a pig, a dog, and a copy - both layers are the same or the outer one is more intensively developed.
The length of smooth muscle tissue may change. In a non-pregnant cow, in the muscular lining of the uterus it is usually 100 microns, with a pregnancy of 1 mm.
The serous membrane (perimetry) consists of loose connective tissue and mesothelium. These tissues form layers located in the following sequence: mesothelium, basement membrane, layer of longitudinally oriented collagen fibers, layer of thin elastin fibers, cambial layer of poorly differentiated cells, deep unformed layer. During pregnancy, in the lining of the uterine horn that contains the fetus, the thickness of collagen and elastin fibers increases, and a new formed collagen layer of circularly arranged fibers is formed in the cambium layer. Destruction of elastin fibers occurs in late periods of pregnancy.
Consequently, the trophic, respiratory, and excretory functions are performed by the mucous membrane (endometrium), and the contractile function is performed by the muscular layer (myometrium) of the uterus.
The blood vessels of the uterus form the main vascular network in the myometrium, from which the vessels depart and are directed to all membranes. Under the epithelium there is a dense capillary network. Venous blood collects in the veins from all membranes; the main venous plexus is formed in the vascular layer.
The uterus is innervated by the autonomic nerve plexuses of the abdominal cavity. They include sympathetic, parasympathetic and sensory fibers. They form the main plexuses in all three membranes of the uterus. The nerve fibers coming from these plexuses end on smooth muscles and connective tissue; receptor nerve endings are also located in all membranes. The nerve plexuses adjacent to the horns and body of the uterus do not contain nerve cells. They are located in the ganglia of the lower and lateral surfaces of the cervix. These are sympathetic neurons and also chromaffin cells.
During puberty, the number of nerve elements in the uterus increases, and there are especially many of them during pregnancy.
Placenta . The structure of the placenta is described in the chapter “General Embryology”.
The vagina consists of the vagina itself and its vestibule. The wall of the vagina itself is represented by three membranes: mucous membrane, muscular layer, and adventitia.
The mucous membrane forms longitudinal folds and is built of squamous stratified epithelium and the main lamina.
The number of layers in the epithelium can vary, due to the period of the reproductive cycle. During estrus it reaches its maximum. The main plate is formed by loose connective tissue and contains lymphatic follicles.
The muscularis propria consists of smooth muscle. There are internal - circular, external - longitudinal layers.
The adventypia is built of loose connective tissue.
The vestibule of the vagina has mucous membrane, muscular membrane and adventitia.
The mucous membrane consists of squamous stratified epithelium and the main plate. The connective tissue of the main plate on the lateral wall contains the bulbs of the vestibule. This is a modified cavernous body of the urethra. The bulbs of the vestibule are well developed in mares and bitches. The epithelium of the mucous membrane contains large, or dorsal, and small, or ventral, vestibular glands. The first are simple tubular glands. Their terminal sections are built of prismatic glandular cells, large excretory ducts are lined with flat multilayer epithelium and open on the side wall of the vestibule. The second are simple branched tubular-alveolar glands that secrete a mucous secretion. Their excretory ducts open on the surface of the mucous membrane in different parts of the vestibule (pig, horse, dog) or in the lower part of the mucosa (ruminants, cats).
The muscular coat is built from striated muscle tissue that does not have a clearly defined layer-by-layer orientation.
The adventitia consists of loose connective tissue.
The clitoris is an organ homologous to the male penis. It is also built from the corpus cavernosum and is covered with a tunica albuginea. Its mucosa consists of flat stratified epithelium. The main plate forms a ring-shaped fold called the priputia. The mucous membrane is abundantly supplied with different types of receptor nerve endings. Among them, the genital corpuscles have a special development.
There are large species differences in the structure of the corpus cavernosum. It is well expressed in mares; in other animals it can turn into adipose tissue.
The labia are formed by folds of skin that pass into the mucous membrane of the vestibule. The sebaceous and sweat glands are well developed in the skin. The basis of the labia is striated muscle tissue.
The organ is abundantly innervated.
Changes in female genital organs and different periods of sexual life. The development of follicles, ovulation, and the formation of the corpus luteum in the ovaries occur cyclically. At the same time, changes are noted in other organs of the female reproductive system. The reproductive cycle is the period of time between two heats. Its duration depends on the type of animal. In wild animals, estrus usually occurs once a year, giving birth occurs in the warm season, which
Rice. 320. Graph showing the correlation between changes occurring during the astral cycle in a sow (according to Carlson).
essential for developing newborn animals. In domestic animals, the time of year is of secondary importance, so their sexual cycles are much shorter: in cows, pigs, small ruminants - every 17-21 days, in a mare - every 21-28 days or more, irregularity often occurs.
The sexual cycle includes the following phases: pre-estrus, estrus, post-estrus and inter-estrus (Fig. 320).
Precursor - preparatory phase. Tertiary follicles grow and begin to protrude above the surface of the ovary. The corpus luteum of the previous cycle is significantly reduced. In the oviduct and uterus, the height of epithelial cells doubles (or more). In a cow, two days before the start of estrus, secretion of the glands of the uterine mucosa begins, their cells multiply, the lumens and length of the glands increase. The cells of the epithelial lining of the vagina also multiply, so its thickness increases.
Estrus is characterized by ovulation and the readiness of the uterine mucosa to receive the fetus. In cows, estrus lasts 2-30 hours, in mares 5-15 days, in dogs 9-14 days. Ovulation can occur when it subsides (in a cow, 24 hours after the start and 14 hours after the end). During estrus, the greatest changes in the female's reproductive apparatus are noted. The wall of the uterus thickens due to the mucous membrane: the number of secretory cells in the integumentary epithelium increases, some of its cells may slough off, the lamina propria loosens, blood vessels dilate,
Rice. 321. Distribution of embryos in the uterus of a pregnant pig:
1 - cervix; 2 - ovary containing seven corpora lutea; 3 - ovary containing two yellow bodies.
glands grow. Sometimes the capillaries break and the secretion of the glands turns red. The cervix opens and mucus is released through it into the vagina and then through the genital slit.
Afterflow is the phase of formation of the corpus luteum, further swelling of all the membranes of the uterus and vagina. The development of secretory epithelial cells and glands reaches its maximum.
Interestrus is the phase of the reverse development of estrus symptoms. After the reduction of the corpus luteum, the development of new tertiary follicles begins. The thickness of the lining of the uterus decreases; the latter and the vagina return to normal.
If pregnancy occurs, the uterine placenta forms in the uterine mucosa, the smooth muscle cells of the muscular layer multiply and hypertrophy, blood vessels rapidly grow, and the connective tissue layer of the serous membrane of the uterus thickens (Fig. 321).
Reviews (0)
Add a review
How to examine the cervix
The following methods are used to diagnose cervical diseases:
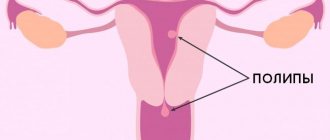
- Gynecological examination . In the mirrors, the doctor can evaluate the color and structure of the organ, detect erosion, polyp, Nabothian cysts and other changes.
- Papanicolaou smear (oncocytology test) . During the examination, the doctor takes a scraping from the cervix and sends the material to the laboratory. A smear shows the structure of the cervical epithelium and allows you to identify inflammation, dysplasia and cancer.
- Colposcopy is an examination of the cervix under a microscope. Allows you to examine the erosion or polyp in detail, evaluate the junction area, and identify pathological changes.
- Ultrasound . With an ultrasound examination, the doctor can assess the length of the cervix and identify the pathology of that part of the organ that is not visible during examination.
This is what a healthy cervix looks like during colposcopy.
All women, even if there are no complaints, are recommended to undergo an annual examination by a gynecologist and do an oncocytology test. This is the only way to notice changes in the cervix in time and maintain health.