What is histology?
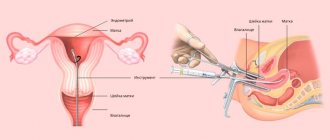
Histology is a branch of biology that microscopically studies the structure of tissues and cellular structures. Histology helps to identify any pathological changes in the endometrium, even at the stage of early cell degeneration. Material for histology is taken by hysteroscopy (hysteroscopy - gynecological examination of the cervix).
This test is called an endometrial polyp biopsy. Biological samples can be taken not only from the uterus and cervical canal, but also from the ovaries. Additionally, cervical mucus and vaginal fluid are analyzed.
Indications for the procedure are:
- the need to clarify the diagnosis;
- identification of the stage of oncology;
- control over tumor dynamics;
- the volume of the upcoming operation;
- monitoring the condition of the endometrium after radiation or chemotherapy.
Histological analysis is indicated when atypical symptoms appear in women:
- pain,
- hurts,
- pulling sensations
- abnormal discharge.
All this may indicate leukoplakia, signs of uterine fibroids, cysts and other neoplasms.
What does histology show?
Histological analysis of endometrial polyps allows us to identify any structural changes in tissues and mucosal cells. Each tissue has its own structure and order of cell arrangement. With any changes, you can suspect oncology or an inflammatory process.
In addition to histology, cytological analysis is performed. Cytology helps determine the structure of the cell (nucleus, membrane) and its functionality.
Both biopsy indicators are important in determining the final diagnosis.
Histological analysis indicates:
- atypicality of cells and tissues;
- structure of neoplasms;
- morphology of the base of the polyp.
Note! If there are no signs of atypia, then the analysis is negative. If positive results are obtained, further treatment tactics are determined. However, positive results indicate not only cancer, but also inflammation, chronic disease, and dysplasia.
How is endometrial polyp histology performed?
Before performing a biopsy, laboratory tests are carried out: a detailed blood test for genitourinary infections, HIV and syphilis, hepatitis, a urine test for protein, sugar and leukocytes. A basic gynecological examination is required, during which a vaginal smear is taken for microflora.
Sometimes a colposcopy is required to identify tumor-like neoplasms on the cervix and in the uterine cavity (find out how colposcopy is done here).
Histology is carried out in several ways:
- Pipeline method - biological material is extracted with a special tube using a vacuum;
- Vacuum aspiration - tissue collection is carried out using vacuum suction;
- Sampling with a microcurette - the mucous membrane is scraped off at the base of the polyp and sent for analysis.
The resulting material is sent to the laboratory for further research.
The laboratory diagnostic algorithm is as follows::
- Treatment and fixation with a special solution;
- Dehydration and ensuring a dense consistency;
- Paraffin impregnation for hardening;
- Cutting into plates using a microtome;
- Placing sections on glass slides and staining;
- Microscopic examination of tissues.
The obtained materials tolerate freezing well, which allows analysis several days after collection of the material. The test is usually carried out on the day of sample collection.
How much is done?
The timing of the analysis varies within 5-10 days. It all depends on the laboratory or medical institution. If the laboratory is located on the territory of the medical institution where the woman took the test, then the data can be obtained in 3-5 days. If sample transportation is required, the turnaround time may increase by several days.
Sometimes doctors resort to a rapid diagnostic method, when tissue is examined directly during hysteroscopy. If oncology is suspected, an extended surgical operation is performed. Errors in diagnostic testing are rare, but if false-positive results are suspected, the test requires a retake.
Diagnosis of fibromatous polyps
Diagnosis of the pathological process begins with an examination of the patient in a chair. The gynecologist carefully examines the woman’s reproductive organs using mirrors, carefully studying the structural features of the uterine cervix and cervical canal.
An additional method for diagnosing the disease is ultrasound. During the ultrasound examination, the specialist gets the opportunity to thoroughly examine the anatomical features of the uterus, fallopian tubes and ovaries.
Before treating polyps in the cervical cavity, the doctor must perform a biopsy - that is, take a small particle of the tumor for laboratory testing. As a result, it is determined whether the tumor is benign or malignant. Pregnancy is not considered a contraindication for tumor biopsy.
Diagnosis of a glandular fibrous endometrial polyp occurs during a gynecological examination and using ultrasound. Large polyps are detected during routine palpation examination. Smaller tumors can only be seen on the screen of an ultrasound scanner.
Additionally, the woman will be prescribed blood tests for hormone levels: follicle-stimulating hormone, luteinizing hormone, estradiol, progesterone, testosterone, prolactin, etc. This is necessary to determine hormonal imbalances, if present.
The most effective is to carry out diagnostic and treatment hysteroscopy or laparoscopy. These methods of minimally invasive intervention make it possible to accurately establish the diagnosis and carry out treatment. The full list of necessary studies is determined by the attending physician.
Decoding
The results can only be interpreted by the attending physician.
Based on the obtained sample, the following types of endometrial polypous neoplasms are histologically identified::
- Ferrous . At the heart of the polyp are functioning glands. The danger of malignancy remains constant. Women at risk during pregnancy, menopause and active hormonal disorders. Treatment of endometrial glandular polyp is described in detail on our resource.
- Glandular-fibrous . Combined polyp structure with glandular and fibrous cells. Often diagnosed in young women with an adequate menstrual cycle. Read more about the treatment of glandular fibrous polyp here.
- Fibrous . Dense, nonfunctional polyps that rarely become malignant. Cancer risk increases with a woman's age.
- Adenomatous . Such polyps are classified as precancer and are extremely rare in gynecology. Atypical cells of adenomatous polyp are most often activated after childbirth or menopause. Adenomatous polyp of the uterus, find out what it is in this article.
Hyperplastic processes of the endometrium
The endometrium is a target organ for sex hormones due to the presence of specific receptors in it. A balanced hormonal effect through cytoplasmic and nuclear receptors ensures physiological cyclic transformations of the uterine mucosa. Violation of hormonal status can lead to changes in the growth and differentiation of endometrial cellular elements and lead to the development of hyperplastic processes.
The leading place in the pathogenesis of HPE is given to relative or absolute hyperestrogenism, the absence of the antiestrogenic effect of progesterone or insufficient influence. Causes of hyperestrogenism: anovulation caused by persistence or atresia of follicles; hyperplastic processes in the ovaries or hormone-producing ovarian tumors (stromal hyperplasia, tecomatosis, granulosa cell tumor, theca cell tumors, etc.); violation of the gonadotropic function of the pituitary gland; hyperplasia of the adrenal cortex; improper use of hormonal drugs (estrogens, antiestrogens).
However, GGE can also develop when hormonal balances are not disturbed. In the development of such pathological processes, the leading role is played by disorders of tissue reception. Infectious and inflammatory changes in the endometrium can lead to the development of GPE in 30% of patients.
In the pathogenesis of HPE, metabolic and endocrine disorders also occupy an important place: changes in fat metabolism, metabolism of sex hormones in pathologies of the hepatobiliary system and gastrointestinal tract, immunity, and thyroid function.
I'M IN. Bohman put forward the concept of two pathogenetic variants of GPE. The first option is characterized by the diversity and depth of hyperestrogenism in combination with disorders of fat and carbohydrate metabolism and manifests itself in anovulatory uterine bleeding, infertility, late onset of menopause, hyperplasia of the theca tissue of the ovaries, in combination with feminizing ovarian tumors and polycystic ovary syndrome. Often, uterine fibroids and diffuse endometrial hyperplasia occur, against which polyps, foci of atypical endometrial hyperplasia and cancer arise. Metabolic disorders lead to obesity, hyperlipidemia and diabetes mellitus. In the second pathogenetic variant, these endocrine metabolic disorders are not clearly expressed or are completely absent; fibrosis of the ovarian stroma is combined with the normal structure or atrophy of the endometrium, with the appearance of polyps, focal hyperplasia (including atypical) and endometrial cancer.
In recent years, a complex system of factors involved in cellular regulation has been identified, and ideas about intercellular interactions and intracellular processes in hormone-dependent tissues have been expanded. Thus, it has been established that, in addition to estrogens, a number of biologically active compounds (polypeptide growth factors, cytokines, arachidonic acid metabolites), as well as the system of cellular and humoral immunity, are involved in the regulation of the proliferative activity of endometrial cells. In the regulation of tissue homeostasis processes and the pathogenesis of proliferative diseases, an important role is played not only by increased cell proliferation, but also by dysregulation of cell death (apoptosis). Resistance of endometrial cells to programmed cell death (apoptosis) leads to the accumulation of altered and excessively proliferating cells, which is characteristic of neoplastic changes in the endometrium.
Thus, the pathological transformation of the endometrium is a complex biological process that affects all parts of the neurohumoral regulation of the woman’s body.
As a rule, the functional layer of the endometrium undergoes hyperplastic changes, and much less often the basal layer.
According to the WHO histological classification (1975), there are 3 main types of GPE: endometrial polyps, endometrial hyperplasia, atypical endometrial hyperplasia.
In 1994, WHO adopted a new classification of GPE, based on the recommendations of leading gynecologists and pathologists.
- 1.1. GPE - proliferation of endometrial glands without cytological atypia:
- 1.1.1. Simple GPE corresponds to the previously accepted glandular cystic hyperplasia, with the characteristic overgrowth of the predominantly epithelial component of the glands characteristic of this condition.
- 1.1.2. Complex or complex (adenomatosis) GPE corresponds to atypical GPE of degree I, differs from simple GPE by the structural rearrangement of the glands and the proliferation of epithelial glands.
- 1.2. Atypical GPE - proliferation of endometrial glands with signs of cytological atypia:
- 1.2.1. Simple atypical GPE corresponds to atypical GPE of degree II and is characterized by pronounced proliferation of the glandular epithelium without signs of cellular and nuclear polymorphism.
- 1.2.2. Complex, or complex, atypical GPE is similar to grade III atypical GPE and has signs of cellular and nuclear polymorphism along with disorganization of the epithelium of the endometrial glands.
GPE occurs in approximately 5% of gynecological patients. This “histological” concept means increased growth, thickening of the uterine mucosa up to 15 mm or more, lack of division into compact and spongy layers, and disruption of the correct distribution of glands in the stroma. Depending on the severity of proliferative processes, glandular GPE is divided into “active” and “resting”. The “active” form is characterized by a large number of mitoses in the epithelial cells of the glands and stroma, high activity of alkaline phosphatase and the appearance of clusters of clear cells in the glands. These signs indicate intense estrogenic exposure - absolute hyperestrogenism (follicle persistence). The “resting” form of glandular GPE occurs with prolonged exposure of the endometrium to low levels of estrogenic hormones (follicular atresia). The endometrium is resting, non-functioning: the epithelial nuclei are intensely colored, mitoses are very rare or do not occur at all.
Based on the condition of the glands, glandular and glandular-cystic GPE are distinguished (B.I. Zheleznoye, 1981). In addition, diffuse and focal, simple and polypoid GPE are distinguished. However, most morphologists do not see a fundamental difference between them.
According to the classification of the International Association of Pathomorphologists (1985), HPE is divided into hyperplasia without cellular atypia and hyperplasia with cellular atypia, which is important for patient management tactics. There are simple hyperplasia with minor structural disorders of the glands and complex (complex) with altered endometrial architecture.
Atypical HPE involves cytological atypia, namely lack of polarity, enlargement and stratification of nuclei, changes in their shape, increased nuclear-plasmic ratio, and irregular chromatin complexes.
According to the classification of B.I. Zheleznova (1977) the terms “atypical” and “adenomatous” GPE are used as synonyms, but the first is used in relation to diffuse endometrial lesions, and the second - to local processes.
GPE is of interest mainly from the point of view of the development of endometrial cancer. Simple HPE without atypia turns into cancer in 1% of cases, polypoid without atypia - 3 times more often. Simple atypical HPE without treatment progresses to cancer in 8% of patients, and complex atypical HPE in 29% of patients.
From a morphological point of view, endometrial precancer includes hyperplasia with atypia (atypical GPE) and adenomatous polyps. However, the risk of malignancy of GPE depends not only on the morphological form, but also on concomitant gynecological and extragenital pathology (polycystic ovary syndrome, feminizing ovarian tumors, uterine fibroids, obesity, diabetes mellitus or impaired glucose tolerance, hyperlipidemia, dysfunction of the hepatobiliary system). G.M. Savelyev and V.N. Serov (1980) proposed a clinical and morphological classification, according to which endometrial precancer includes atypical GPE and adenomatous polyps in women of any age; recurrent glandular GPE in combination with hypothalamic and neurometabolic-endocrine disorders in a woman of any age; glandular GPE when first detected in postmenopause.
Endometrial polyps are the most common type of GPE, occurring in 5.3-25% of gynecological patients of all age groups. Most often, endometrial polyps are detected in pre- and postmenopausal women and become malignant in 2-3% of cases.
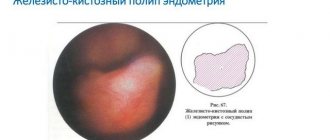
An endometrial polyp is a benign tumor arising from the basal layer of the endometrium. The glands in the polyp are located unevenly, randomly, have different sizes and shapes, and are lined with prismatic epithelium of an indifferent or proliferative type. The vessels have thickened, sclerotic walls; tangles can form at the base of the polyp. The pathognomonic anatomical sign of an endometrial polyp is its base (“pedicle”).
Depending on the histological structure, glandular (functional, basal type), glandular-fibrous and fibrous endometrial polyps are distinguished. Adenomatous polyps are classified as precancerous conditions of the uterine mucosa. Glandular polyps are most characteristic of the reproductive period, glandular-fibrous - for pre- and perimenopause, fibroglandular and fibrous - for postmenopause.
In the reproductive and premenopausal periods, endometrial polyps, as a histologically independent form, can be determined both against the background of HPE and with normal mucous membrane of various phases of the menstrual cycle.
Endometrial polyps in postmenopause are usually single; in 20-26% of patients they are multiple. Endometrial polyps in postmenopause are always determined against the background of an atrophic mucous membrane, sometimes reaching large sizes. Extending beyond the cervix, endometrial polyps mimic cervical canal polyps.
The recurrent form of endometrial polyps deserves special attention. The concept of “relapse” is not applicable if hysteroscopic control was not previously performed when removing an endometrial polyp.
In recent years, the main role in the occurrence of endometrial polyps has been assigned to infectious and immune factors. The development of glandular fibrous endometrial polyps in 75% of cases occurs with undisturbed hormonal ratios; in 95.3% of patients the endometrium is infected. In addition, patients with HPE exhibit severe immunodeficiency due to the immunosuppressive effect of estrogens, the nature and number of infectious agents, and the duration of chronic inflammation. This is especially true for the postmenopausal period, when the synthesis of estrogen in the ovaries sharply decreases, metabolic processes in the endometrium and resistance to the action of any damaging factor, including microbial ones, decrease. As a result of these disorders, a chronic inflammatory process develops in the uterus, which leads to diffuse GPE, and then to the development of focal proliferations.
The role of hormonal disorders as the main factor in the occurrence of endometrial polyps is questioned by many researchers.
A hormonal factor in the pathogenesis of endometrial polyp is currently being considered in patients receiving tamoxifen. Approximately 8% of breast cancer patients receiving tamoxifen develop endometrial polyps.
Possibility of pregnancy after histology
Often a biopsy is performed to study and further treat infertility. The treatment does not immediately lead to a positive result. Considering the traumatic nature of the method, complete restoration of the endometrium is important.
Clinicians believe that the optimal period for pregnancy planning is 2-3 months after hysteroscopy and histological analysis.
Thus, the histological analysis itself does not affect pregnancy, but the method of collecting biological material damages the endometrial membranes. Immediately after the manipulation, the fertilized egg does not attach to the walls of the uterus, rejection and traumatization of the mucous membranes occurs.
After a biopsy and treatment of polyps, it is recommended to regularly examine the uterus and monitor the condition of the mucous membranes. Dynamic monitoring allows for timely detection of relapse. Adequate preparation for pregnancy after histology is the key to successful pregnancy.
Read more about how histology is performed after curettage right here:
Histological examination of endometrial polyps is a highly informative method for studying women, which is included in the annual medical examination program. Early detection of tumors helps reduce the risk of cervical and ovarian cancer significantly.
What is a placental polyp after childbirth, read our article.
You can make an appointment with a doctor directly on our website.
Obstetrician-gynecologist, oncologist, Ph.D.
In 2012, she graduated with honors from the faculty of training and advanced training of civilian doctors of the S.M. Kirov Military Medical Academy, specialty - “General Medicine”.
2014-2015 - obstetrician-gynecologist at the gynecology department of the 31st city hospital in St. Petersburg.
2014 - postgraduate study at the N.N. Petrov Research Institute of Oncology, direction - malignant diseases of the cervix
2016 - professional retraining in the cycle “Colposcopy, destructive methods of treatment of cervical neoplasia”, St. Petersburg State Pediatric Medical Academy.
Area of professional interests: gynecological oncology - ovarian, corpus and cervical cancer, cervical and uterine dysplasia, vulvar cancer; obstetrics and gynecology - preparation for pregnancy, early pregnancy, sexually transmitted diseases, fibroids and ovarian cysts, endometriosis, hormone replacement therapy.
Telephone for registration (office) ext. 1204.
Bleeding of varying intensity usually always accompanies any surgical procedure. Also, minor bleeding may occur after removal of a uterine polyp. In some cases, complications arise in the form of intense bleeding, in which case you should consult a specialist. Severe bleeding after manipulation is a complication.
Uterine polyps have become increasingly detected in patients of different ages due to the use of modern diagnostic methods, for example, ultrasound and hysteroscopy. In many cases, doctors suggest removal of the polyp, which normally may be accompanied by mild bleeding. After the operation, a histology analysis is performed.
However, as experts emphasize, removing polyps does not prevent relapses. Removal of polyps eliminates the consequence of the pathological process, but does not affect its cause. In addition, in rare cases, complications such as heavy bleeding may occur after removal.
Treatment of fibroglandular polyp of the endocervix
Treatment of fibroglandular lesions involves its mandatory removal. The operation is planned. Before treatment, a course of drug therapy is carried out, especially in the presence of inflammatory processes.
Indications for surgical removal are:
- Large growths of the mucous membrane (can cause blockage of the cervical lumen and interfere with pregnancy);
- Woman’s age over 35 years (risks of multiple polyps and polyposis);
- Ineffectiveness of drug treatment, including hormone replacement therapy;
- Infertility of a woman caused by pathological tissue proliferation;
- Risks of malignancy.
Considering the planned nature of the removal, the woman has the opportunity to carefully prepare, and the doctor has the opportunity to formulate the correct removal tactics and choice of method.
Main types of surgery
The following manipulations are effective against polyps:
- Laser coagulation. The method involves removing the polyp by excision of the stalk and evaporation of the pathological tissue under the influence of a laser beam. During the operation, simultaneous soldering of the vessels occurs, which prevents the development of bleeding. The disadvantage of this method is the presence of heavy smoke during surgery and the inability to remove large or multiple polyps.
- Polypectomy. Removal of a pathological growth by excision or twisting from the walls of the cervix. The method is effective for polyps up to 2.5-3 cm. After removal, the wound surface of the bed is cauterized with electrodes or a laser.
- Diathermoexcision. Loop removal, which involves placing a loop on the growth and excision it, followed by cauterization with electric current. It is used for severe dysplasia of the walls of the cervical lumen, as well as for the risk of adhesions and erosive lesions.
- Cryodestruction. The method involves freezing the stalk or body of the polyp using liquid nitrogen. After freezing, the polyp is removed. The main advantage is low trauma and rapid recovery. After manipulation there is no risk of scar tissue formation.
- Radio wave coagulation. Removal is carried out using special equipment - the Surgitron apparatus. It is characterized by minimally invasiveness, low trauma and speed of execution.
- Resection. Abdominal surgery, which involves removing part of the uterine cavity or the entire organ. A radical decision is made when the tumor becomes malignant in order to avoid metastasis to other parts of the pelvic organs.
The type of intervention is selected based on the size and symptomatic picture of the polyposis lesion, as well as on the basis of the characteristics of the woman’s medical history.
Possible complications
Despite the small volume of most removal methods, the risk of complications still remains. The main complication of the operation is the emergence of new lesions. In almost 12% of all clinical cases, relapse occurs.
Other complications include:
- Formation of adhesions and scar tissue;
- Infectious lesion;
- Malignancy of an incompletely removed polyp;
- Bleeding when the canal walls are damaged;
- Allergic reactions, severe swelling;
- Hematometra is severe internal bleeding followed by stagnation of blood in the uterine cavity.
Drug therapy after removal
Considering that the uterus, ovaries, appendages, and cervical canal are hormone-dependent organs, it is important to restore the hormonal levels of the female body. After surgery, there may be an imbalance of progesterone and estrogen, which can lead to unpleasant consequences
After removal of the polyp, the following medications are prescribed:
- Hormonal drugs (Utrozhestan, Duphaston, Tri-Mercy);
- Antibacterial drugs (Diclofenac, Piroxicam, Celecoxib, Cifran-OD);
- Douching with antiseptics (Miramistin, Chlorhexidine, Furacilin).
After removal, women are shown a protective regime, sexual rest and strict adherence to the regimen of taking certain medications. After surgery, you should undergo an ultrasound scan at least 2 times a year, take blood tests, and treat infectious diseases in a timely manner.
The prognosis for timely removal of fibroglandular polyps is favorable. When atypical cells are detected by histology, prognostic criteria are determined by the extent of the oncogenic process.
You can make an appointment with a doctor directly on our website.
Be healthy and happy!
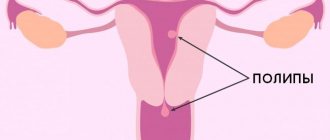
Causes and symptoms of polyposis
Uterine polyps are a consequence of focal endometrial hyperplasia, in which local growth of areas of the mucosa is noted. The pathology is more typical for women after 35-40 years.
Uterine polyps can have different shapes:
Polyposis can be represented by both single and multiple formations.
- on a thin leg;
- on a wide base.
It is generally accepted that uterine polyposis is a hormone-dependent pathology. The reasons for the formation of polyps in the uterus include:
- hyperestrogenism and lack of progesterone;
- long-term inflammatory processes of the genital organs;
- endometrial trauma;
- complications after abortion;
- RDV.
After removal of a uterine polyp, a histology analysis is required to determine the type of polyp. According to histology analysis, the following types of uterine polyps are distinguished:
- glandular;
- fibrous;
- glandular-fibrous;
- adenomatous.
Histology is essential for determining further treatment tactics. If signs of proliferation are detected in a histology analysis, polypous neoplasms are removed along with the uterine body. Delay can lead to a serious complication - the development of uterine cancer.
Small uterine polyps usually have no symptoms. The clinical picture develops with an increase in the size of the tumor and the appearance of multiple polyps. Often, polyposis disrupts the normal contractile function of the uterus, which complicates the process of mucosal rejection. Uterine polyposis can manifest itself:
- bleeding in the middle of the cycle;
- heavy bleeding during menstruation;
- pain in the lower abdomen, for example, during sexual intercourse;
- infertility;
- spontaneous termination of pregnancy.
True basal polyps
They consist of non-functioning glands, fibers and elements of muscle tissue with a predominance of the former. They do not depend on the menstrual cycle and the concentration of hormones in the body. If functional polyps of the glandular structure arise against the background of other hormone-dependent pathologies, then the basal type can form in a completely healthy woman. However, the cause is considered to be an inflammatory process. True endometrial polyps are localized near the junction of the fallopian tubes and at the bottom of the organ. By cutting such a formation, you can observe a loose spongy structure. This is explained by the structure of gland cavities, which are located in disorder.
The reason for the formation of true polyps on the endometrium:
- Damage to the walls of the uterus;
- Inflammatory processes;
- Infections of the reproductive system;
- Impaired cell regeneration;
- Allergic diseases.
Preparing for the intervention
Before removing uterine polyps, it is necessary to undergo an examination in order to prevent complications. In addition, diagnostics allows us to identify contraindications for removal.
The examination before removal of a uterine polyp includes the following studies.
- Study of the condition of the cervix. Often, instruments are inserted through the cervix during the removal process. That is why it is important to exclude inflammatory pathologies, as well as damage to the mucosa.
- Performing strokes. The woman is recommended to undergo smears to detect sexually transmitted infections and assess the condition of the vaginal microflora. If infection is present, removal is not performed due to the risk of complications, such as endometritis.
- Cytological diagnosis. A smear for oncocytology can reveal a precancerous process in the cervix. In such cases, treatment may vary in expanded scope.
- Ultrasound. Ultrasound examination is performed transvaginally and abdominally. Using this diagnostic, you can assess the condition of the internal genital organs.
- General clinical studies. Before hospitalization and removal, an ECG, fluorography, blood and urine tests, including for the diagnosis of syphilis, hepatitis and HIV, should be performed.
Contraindications
During the examination, contraindications are sometimes revealed that are an obstacle to removal. If contraindications are ignored, complications may develop, for example, intense bleeding.
Contraindications that prevent polyp removal include:
- infections and inflammatory processes of the genital organs;
- thrush and bacterial vaginosis;
- pregnancy;
- cervical pathologies that do not allow removal instruments to be inserted into the uterine cavity, for example, stenosis or gross deformation of the tissue as a complication after childbirth;
- severe somatic pathologies, in particular diabetes mellitus, accompanied by a significant increase in blood glucose levels, hypertension with fairly high blood pressure levels or exacerbation of stomach ulcers;
- ARVI.
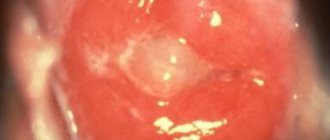
Endometrial polyp of the cervical canal
The anatomical part of the female reproductive system in the internal genital organs is the cervical canal of the cervix. The success of pregnancy and the birth process depends on his health. One of the structural pathologies of the cervical canal is polyps. Such neoplasms grow from the columnar epithelium of the endocervix.
The main causes of damage to the cervical canal:
- Traumatization during obstetric manipulations and during the birth process. Injuries are possible if the intrauterine device is installed incorrectly.
- Sexual infections.
- Structural changes in the surface of the cervix - erosion, leukoplakia.
- Violation of the vaginal microflora.
- Nonspecific infection – vaginitis, endomyometritis, vulvovaginitis, cervicitis.
- Ovarian dysfunction – polyposis, fibroids.
- Endocrine pathologies – diabetes, obesity, chronic stress.
- Hormonal disorders.
The pathological condition is manifested by bloody discharge and pain after intimacy. Many women experience menstrual irregularities and profuse leucorrhoea (if infected, they are mucopurulent in nature). If the growth puts pressure on the glands of the cervical canal, then abundant mucous discharge appears. With neoplasia of large size, nagging pain occurs in the lower abdomen.
Without timely diagnosis and treatment, growths in the cervical canal pose a threat to women's health:
- Malignant transformation.
- Risk of uterine bleeding.
- Tumor necrosis and intoxication of the body.
- Hematometra.
- Pregnant women have a risk of spontaneous abortion, low location of the placenta and the development of isthmic-cervical insufficiency.
In most cases, a standard gynecological examination is sufficient to identify pathology. During the examination, thickened and hypertrophied walls of the cervix are determined. Focal tissue proliferation may block the canal.
Treatment is surgical. First of all, the entire cervical canal is scraped. There are also other surgical techniques used for neoplasia: diathermocoagulation, cryodestruction, laser polypectomy. In especially severe cases, amputation of the cervix is indicated. The operation is performed for frequent relapses and malignant tissue degeneration. This treatment allows you to preserve the patient’s reproductive functions.
[], []
Removal methods
A polyp in the uterus is subject to removal in most cases, which is often performed through hysteroscopy followed by RDV. This procedure involves separate diagnostic curettage of the uterus and cervix. After collecting the material, it is carefully examined as part of a histology analysis.
Treatment tactics and indications for removal depend on the following factors:
- size and structure of formations;
- age;
- endometrial condition;
- causes of polyposis;
- history of metabolic and endocrine pathologies.
Indications for removal depend on the type of polyp. For example, fibrous tumors necessarily require removal. Glandular fibrous polyps, which are identified as part of a histological examination, indicate a hormonal imbalance. After their removal, the woman is indicated for treatment with hormonal drugs.
Adenomatous polyps can lead to complications such as uterine cancer. If they are detected, removal of the uterus, cervix, and ovaries in women before the onset of menopause is often indicated.
On the eve of removal, the patient can only consume easily digestible food. Cabbage, brown bread and legumes should be excluded. Doctors recommend a glass of kefir for dinner. You should not eat or drink before removal. When prescribed by the attending physician, the patient is given an enema in the evening and also in the morning.
Removal of uterine polyps is usually carried out on the second or third day after the end of menstruation. During this phase of the cycle, polyps are clearly visible in the uterine cavity. Thus, removal is less likely to be accompanied by complications, in particular bleeding.
Removal of a polyp in the uterus is performed in a hospital setting. The duration of hospitalization is several days. The woman sits on a gynecological chair, where she is injected with painkillers intravenously. In some cases, spinal anesthesia and endotracheal anesthesia are used as pain relief.
The choice of anesthesia option depends on the following factors:
- duration and volume of removal;
- a history of concomitant diseases;
- intolerance reactions to certain medications;
- possible risk of complications.
Hysteroscopy
Polyp removal using hysteroscopy is usually performed under general anesthesia. At the beginning of the intervention, the doctor inserts a hysteroscope, which is a thin tube, into the cervix. The built-in video camera transmits the resulting image to the screen. Thus, the specialist examines the uterus, identifies the location of formations and their number. Then, using a special instrument on a hysteroscope, the polyps are removed. After removal, the resulting tissue is sent to the laboratory for histology.
If the formation progresses on a stalk, removal is performed by a kind of “unscrewing”. Then the site of attachment of the leg is cauterized with current, laser or treated with liquid nitrogen. This procedure is necessary to prevent complications and relapses of the pathology. The duration of hysteroscopy is 10-30 minutes.
Scraping
It is known that in most cases, polyposis recurs after removal. That is why after removal the bed is processed. Sometimes, in the absence of the necessary equipment, a woman is simply offered curettage. In this case, the doctor works without determining the location of the formation and its size. Curettage is recommended to be performed after hysteroscopy.
What is a glandular fibrous polyp of the endometrium?
It is one of the types of endometrial hyperplastic processes and is a single or multiple benign formation of an oval or round shape with a smooth or nodular surface, growing into the uterine cavity. Its diameter ranges from several millimeters to several centimeters (more details about the types of polyps and their treatment can be found in our previous article).
The endometrium (uterine mucosa) consists of two layers - functional and basal. The functional layer always responds to cyclical and other changes in the content of sex hormones in the body and is separated during menstruation. This is accompanied by menstrual bleeding.
The restoration of the functional layer occurs due to the cells of the dense basal (supporting, main) layer, which differs from the first in cellular composition and structure. His reaction to hormonal fluctuations is minimal.
Accordingly, according to the place of formation, endometrial polyps of functional and basal types are distinguished. These formations have a glandular structure, and their differences are determined mainly by histological examination.
Functional type
Formations are formed from the functional layer as a result of the excessive influence of estrogens or progesterone. They, along with the entire endometrial layer, take part in all cyclic changes and transformations, that is, they are active.
They are characterized by a mature structure and great morphological variability. Glands in polyps of this type, as a rule, are randomly located, have a wavy shape (saw-shaped), the type of epithelial cells lining them is secretory or proliferative, the stroma is cellular in nature. A vessel is often found in the stalk of the formation.
Basal type
In contrast to the functional one, the glandular-fibrous polyp of the basal type comes from the corresponding layer of the endometrium and is located locally on the pedicle in which the vessels pass. Morphological changes in them are represented predominantly by stroma (connective tissue), which occupies the main volume of the polyp, and consists of coarse fibrotic and, to a lesser extent, collagen and muscle fibers.
In polyps of this type, glands of the basal type may be found in small quantities. A distinctive feature of the latter is the uneven location in different directions. In addition, their lumens are unevenly expanded, and some glands are stretched like cystic formations covered with flattened epithelium.
In histological examination of the tissue of a glandular fibrous polyp, glands with epithelial cells of the proliferative or secretory type are sometimes found. But basically the epithelium is represented by uterine, often atrophic, cells of an indifferent (indifferent, non-functioning) type, that is, not responding to the influence of sex hormones. Sometimes glandular cells are completely absent. In various areas of the tumor formation there are a few glomeruli of vessels with thickened sclerotic walls.
Polyps can develop against the background of an unchanged mucous membrane or against the background of the endometrium, which is in a different morphofunctional state. This is possible during reproductive age or menopause, that is, at the stage of retrogression (reverse development) of the endometrium, at the stage of hyperplasia, proliferation or atrophy, which also affects the cellular composition of the polypous formation. Depending on the predominance of certain cell types, two variants of the latter are conventionally distinguished:
- indifferent variant of glandular fibrous endometrial polyp;
- retrogressive variant of glandular fibrous endometrial polyp.
This morphological difference is a histological characteristic and is only slightly related to clinical manifestations. Sometimes it helps determine the choice of treatment principle after polyp removal.
Quite often, these tumors show signs of an inflammatory process and/or circulatory disorders, leading to necrobiotic and dystrophic changes in their individual areas. In the first case, they become swollen and hyperemic (full-blooded), in the second, they acquire a mosaic color (light areas alternate with cyanotic and purple ones). As a rule, these changes are of a combined nature.
Treatment during the recovery period
The risk of complications is minimal when performing hysteroscopy. In the first few days the following may appear:
- spasmodic pain indicating contraction of the uterus;
- minor bloody and bloody discharge.
Complications after hysteroscopy are rare. For three days, the patient is prescribed no-shpa to prevent such complications as hematometra. With this complication, no bleeding is observed, since clots accumulate in the uterine cavity.
After the intervention, a course of anti-inflammatory drugs is usually recommended, since polyps often develop due to inflammation. For hormonal causes of polyps, after evaluating the histology analysis, appropriate drugs are prescribed, for example, Norkolut, Utrozhestan, Duphaston.
Treatment of polyps on the cervix
To determine the optimal and most effective method of treatment, the doctor must take into account factors such as the age and health of the patient, the causes and characteristics of the development of the disease, as well as the results of tissue biopsy.
The main method of treating polyposis in women remains surgical removal. There are several types of surgical techniques that allow you to quickly and painlessly remove a polyp from the surface or cavity of the cervix.
- Laser coagulation is one of the most effective and safe methods used to remove polyps in nulliparous girls. It features minimal pain and a short recovery period.
- Hysteroscopy is the introduction of miniature surgical instruments and a video camera into the uterine cavity, with the help of which the tumor is excised.
- Radio wave excision.
- Endoscopic polypectomy is an operation in which not only polyps are removed, but also their base is cauterized.
- Classic full curettage.
Any operation is accompanied by a rehabilitation period, during which it is recommended to take anti-inflammatory and antibacterial medications. If necessary, the patient is prescribed hormonal medications, which are intended to normalize hormonal levels in the female body.
Recovery after removal of fibromatous polyps of the cervix
After an operation to eliminate polyps in the uterine cavity or cervix, vaginal discharge of a mucous or bloody type may appear during the first weeks. Do not despair, such signs are the norm and disappear on their own after the organ mucosa is completely restored.
In order to speed up the healing of uterine tissue, you need to remember several important rules:
- during the first 2-4 weeks after surgery, you should avoid sexual contact;
- during menstruation, it is best to use sanitary pads rather than vaginal tampons;
- refusal to douche;
- during the recovery period you need to avoid visiting the solarium;
- It is prohibited to swim in open reservoirs and pools;
- you should not visit baths or saunas;
- for hygiene procedures it is best to use a shower rather than a bath;
- It is prohibited to engage in sports or intense physical activity.
Restoration of the mucous surface of the uterus and cervical canal will be quick and painless if the woman strictly follows these rules. Also, in no case should you forget about preventive gynecological examinations, because this is an excellent way to prevent the development of many gynecological diseases.
Video: Cervical polyp - about the disease
CERVICAL POLYP - about the disease
Video: laser polyp removal
VLOG: laser removal of POLYPS
Video: cervical polyp. Fast and effective removal
Cervical polyp. Fast and effective removal
Histology results
Usually the histology analysis is ready in ten days. The results of the histology analysis are essential for determining the tactics of postoperative treatment. There are several types of polyps according to their histological structure.
- Glandular. This neoplasm is formed predominantly from glandular tissue, which causes its softness. Glandular polyps grow more often in young women. In older patients, they can contribute to the development of uterine cancer.
- Fibrous. The formation includes cells of fibrous tissue. Compared to the glandular form, such polyps are characterized by density. Glands are contained in small quantities, which is determined by histology. Such neoplasms grow more often in elderly patients, and therefore the level of malignant degeneration increases.
- Glandular-fibrous. This is a mixed variety, which is more often diagnosed as part of a histology analysis in patients with a normal cycle. These polyps contain fibrous and glandular tissue in approximately equal amounts. A feature of the glandular-fibrous form is the frequently developing inflammatory process.
- Adenomatous. This is a precancerous variety, which is relatively rare according to histology. Polyps include signs of atypia, which is especially dangerous in old age. Malignant degeneration most often occurs in women after menopause.
Symptomatic manifestations
Small-sized neoplasia is rarely accompanied by a clinical picture, and most often the polyp is discovered by chance during a routine examination.
Women in their reproductive years may experience vaginal discharge mixed with blood between periods.
Women who have already reached menopause may notice the presence of scanty bleeding, which can be both long-term and short-term. Often, spotting can occur after intimacy.
If the formation has reached a large size, nagging or sharp pain may appear in the lower abdomen. In the case of necrobiosis, the patient may complain of an increase in the amount of leucorrhoea.
Symptoms of fibrous formation in the uterus are quite nonspecific, and can also be observed with other gynecological pathologies. Therefore, consultation with a doctor and a thorough diagnosis of the disease are mandatory.
Expert opinion
Dmitrieva Elena Yurievna
Gynecologist-endocrinologist, 40 years of experience
Fibrous polyps are considered the safest tumor formations in the uterine cavity. Their transformation into a malignant formation during reproductive age is practically not observed, and in addition, they are extremely rarely accompanied by any complications. However, this does not mean at all that such neoplasms cannot be treated. Large polypous formations can interfere with pregnancy, and if there is bleeding, a woman can develop anemia. The most dangerous fibrous polyps are in the premenopausal period (40-50 years), because at this age the transformation of formations into a malignant process is up to 8%.