Consultation with plastic surgeons with over 20 years of experience is free! Make an appointment by phone. Waiting for you! When we talk about levatoroplasty, we almost always mean posterior colporrhaphy. Together, these two operations effectively strengthen the vaginal walls and pelvic floor muscles, preventing organ prolapse and allowing a woman to live a full and healthy life. Strengthening or suturing torn perineal muscles is often necessary after childbirth. This explains the popularity of posterior colporrhaphy with levatoroplasty in our clinic.
Description
Colporrhaphy is a plastic correction aimed at changing the volume of the vagina, eliminating various defects in the development of the genital organs, congenital or acquired.
On this topic
- Intimate plastic surgery
Vaginoplasty
- Editorial board of Plasticology.ru
- October 18, 2021
Vaginal plastic surgery involves achieving a number of goals. The main ones include the following:
- narrow the lumen and reduce the size;
- get rid of sagging ;
- adjust arch lines;
- remove pathological expansion of the vaginal walls;
- strengthen the organ;
- eliminate deforming or painful scars that could have formed as a result of an episiotomy or when suturing a genital rupture.
As a result, at the end of the surgical intervention, the stretching of the vaginal walls and its prolapse are eliminated. At the same time, the functionality of the vagina is not impaired in any way, including during childbearing age.
Kinds
Currently, experts classify colporrhaphy into three types, with the help of which the vagina can be sutured.
Front
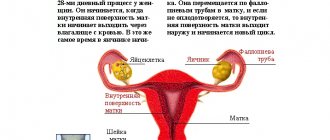
The main goal of anterior colporrhaphy is to suturing and strengthening the anterior vaginal vault adjacent to the urethra and bladder.
Middle
It is a combined type method. In this case, both walls of the genital organ are excised and sutured. Most often, such manipulation is prescribed for severe prolapse, accompanied by prolapse of the cervix of the uterine body in patients whose age is not predisposed to childbearing.
Rear
Posterior colporrhaphy is an operation to stitch the vagina to the rectum. In addition, a combination of posterior colporrhaphy and levatoroplasty is often observed, when the muscles of the pelvic organs are simultaneously strengthened.
Indications
As a rule, vaginal plastic surgery is performed for medical reasons, among which are prolapse of its walls, as well as functional or anatomical disorders associated with this condition. It is the development of complications of adjacent internal organs that most often becomes the reason for performing this type of surgical intervention.
On this topic
- Intimate plastic surgery
Phalloplasty
- Editorial board of Plasticology.ru
- October 18, 2021
If a first degree prolapse is diagnosed, this is not yet a compelling reason to prescribe colporrhaphy. In such cases, the woman is prescribed conservative therapy, which consists of performing gymnastic exercises aimed at strengthening the muscles of the pelvic floor and vulvovaginal area. If prolapse is detected at stages 2-3, a decision is made on surgical intervention.
Thus, the main indications for vaginal suturing surgery are as follows:
- urinary incontinence - the cause of this condition is displacement of the urethra, as well as severe stretching of its mouth, or cystocele (prolapse of the bladder);
- discomfort during bowel in the absence of constipation;
- the occurrence of pain during sexual intercourse or when performing physical exercises;
- protrusion of the vaginal mucosa beyond the boundaries of the genital fissure - this condition is accompanied by relapses of vulvovaginitis, ulceration of prolapsed soft tissues, maceration, and an increased risk of degeneration into a malignant tumor;
- gas incontinence and spotting - the cause is most often sphincter incompetence, when the rectum is displaced against the background of prolapse of the posterior vaginal wall.
On this topic
- Intimate plastic surgery
Circumcision
- Editorial board of Plasticology.ru
- October 18, 2021
Colporrhaphy can also be prescribed upon request. As a rule, in such situations, surgery is performed to reduce the size of the vagina, and also if there are no signs of prolapse. The main reasons why intimate plastic surgery is performed are anorgasmia or deterioration in the quality of sexual life.
In addition, the operation is required in the presence of characteristic anatomical features, when the size of the genital organs of both partners does not correspond to each other.
Posterior colporrhaphy, levatoroplasty for NMTD
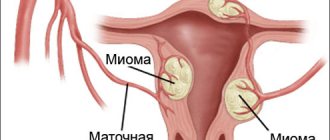
Genital prolapse (synonyms: prolapse, prolapse of the internal genital organs, insufficiency of the pelvic floor muscles) is a disease of the female genital area, combining a group of disorders of the ligamentous apparatus of the uterus and vagina, leading to prolapse and prolapse of the internal genital organs in women. First of all, genital prolapse is manifested by prolapse and prolapse of the uterus and vagina. Less commonly, prolapse manifests itself as prolapse and prolapse of the rectum. Causes of uterine prolapse and pelvic organ prolapse
The producing factor in the development of organ prolapse is an increase in intra-abdominal pressure of various types, and the predisposing factor is the incompetence of the pelvic floor. The main causes of pelvic floor incompetence:
- violation of the synthesis of sex hormones;
- chronic diseases (accompanied by metabolic disorders, microcirculation, sudden frequent increases in intra-abdominal pressure);
- post-traumatic injury to the pelvic floor;
failure of connective tissue structures in the form of “systemic” failure. Surgical treatment of pelvic prolapse includes not only the elimination of disturbances in the anatomical position of the uterus and vaginal walls, but also the correction of functional disorders of adjacent organs (bladder and rectum).
When performing an operation for uterine prolapse, it is necessary to achieve the reconstruction of the structure of the pelvic floor, the correct arrangement of organs, maintaining the necessary mobility of organs, and creating an elastic vagina of sufficient length.
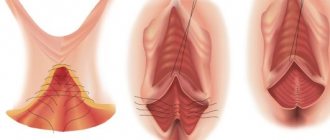
The essence of the operation is to reduce the volume of the vagina by removing the “extra” section of the mucosa, strengthening the walls of the rectum and the muscular frame of the perineum. The operation is performed through vaginal access, which allows achieving an excellent cosmetic effect. The surgery is performed on a gynecological operating chair.
After dissecting the vaginal mucosa, the rectal wall is separated and immersed using sutures. The levators (muscles) are released and with the help of the muscle the posterior wall of the vagina is strengthened. The vaginal mucosa and perineum are sutured. Indications: - prolapse of the posterior vaginal wall. — Cicatricial changes in the perineum (after episiotomy, ruptures of the perineum during childbirth) Examination for surgical intervention and the validity period of the examination results: You can undergo the entire scope of the preoperative examination at our Paracel MC in one day!
- colposcopy-12 months
- Ultrasound of the pelvic organs
- Ultrasound of the veins of the lower extremities - 3 months
- Flora smear, bacteriological culture from the cervical canal - 10 days
- oncocytology of the cervix – 6 months
- General urine test - 10 days, General blood test and reticulocytes - 10 days,
- Electrocardiogram with interpretation -14 days,
- Blood for HIV, Hepatitis B, Hepatitis C, Syphilis 3 months.
- Biochemical blood test: general, direct, indirect Bilir., Total Protein, albumin,
- urea, glucose, creatinine, uric acid, AST, ALT, alkaline phosphatase, blood sodium and potassium, cholesterol -10 days
- Coagulogram - 10 days
- Blood type and Rh factor
- Fluorography - 6 months.
- Mammography -24 months (after 36 years to 50 years), 12 months (after 50 years) Ultrasound of the mammary glands (up to 36 years) -12 months
- Consultation with a therapist, anesthesiologist and other specialists according to indications. Other examinations may be added as indicated.
Anesthesia: These operations are performed under spinal anesthesia or endotracheal anesthesia. The method of pain relief is chosen jointly by the anesthesiologist and the surgeon, of course, taking into account the wishes of the patient.
Contraindications:
Planned intervention is not performed for clinically significant blood clotting disorders, acute infections, decompensated somatic diseases (hypertension, unstable angina, severe diabetes mellitus, severe anemia).
Contraindications
Colporrhaphy has a number of limitations. Thus, among the main absolute contraindications there are:
- violation of the hematopoietic ;
- pathologies of the heart and blood vessels at the acute stage;
- kidney disease ;
- venereal diseases.
Restrictions also include:
- age under 18 years;
- gynecological pathologies ;
- cold;
- inflammatory processes occurring in the bladder;
- pustular formations localized in the perineum;
- early postpartum period.
If we talk about median colporrhaphy, it cannot be performed on women who are sexually active and plan to conceive a child in the future.
Contraindications to plastic surgery of the intimate area
Perineal plastic surgery is not performed when diagnosing the following pathological processes and disorders:
- Severe cardiovascular pathology;
- Decompensated chronic diseases of internal organs;
- Inflammatory and infectious diseases of the genitourinary system;
- Venereal pathologies;
- Bleeding disorders;
- Diabetes mellitus in the decompensation stage;
- Excessive scarring of tissue (the appearance of keloid scars).
The advisability of perineoplasty is determined by the attending physician after a thorough examination, laboratory tests and clinical studies. This will allow you to diagnose contraindications and assess the patient’s health status.
Preparation
In order for the operation to be as successful as possible and with minimal complications, you need to properly prepare for it. At the first consultation, the gynecologist examines the patient, determines the presence of vaginal prolapse and its severity, and cervical prolapse. In the case where surgical intervention is solely the desire of the woman, permission to perform the manipulation is immediately signed.
Based on existing complaints and wishes, the optimal surgical option is selected.
To exclude the presence of possible contraindications, the patient is referred to undergo laboratory and instrumental examination, which may include:
- coagulogram;
- general blood test and biochemistry;
- STI testing;
- taking oncocytological poppy;
- fluorography;
- ultrasonography;
- colposcopy;
- vaginal smear to identify flora.
On this topic
- Intimate plastic surgery
Labiaplasty
- Editorial board of Plasticology.ru
- October 18, 2021
Also during the preparatory period it is necessary to adhere to the doctor’s recommendations.
Two days before surgery, you need to exclude from your diet foods that can cause increased gas formation.
The day before colporrhaphy, the perineum is treated with an antiseptic solution, which is recommended by a specialist.
On the eve of the operation, bowel cleansing procedures are performed, as well as genital hygiene; it is important to make a deep bikini to get rid of hair.
To the clinic, a woman takes with her compression garments, sanitary pads and compression stockings. The last meal should be at least 8 hours before surgery.
Progress
Colporrhaphy is performed exclusively in a hospital setting. The patient is hospitalized as planned several days before surgery.
On this topic
- Intimate plastic surgery
How is the hymen restored?
- Editorial board of Plasticology.ru
- June 19, 2021
The procedure is performed only under general anesthesia. Some medical institutions practice the administration of epidural anesthesia. However, in this case, a special diet is required, which involves fasting.
All manipulations are carried out using access through the vaginal opening. An atraumatic clamp is used to fix and retract the cervix of the uterine body. The vaginal walls are excised, and a diamond-shaped flap is isolated. The necessary muscles are sutured and fixed. In this case, the incision will have a certain position depending on the type of colporrhaphy chosen.
After the main stage of the surgical intervention is completely completed, the tissues undergo layer-by-layer suturing. Self-absorbing sutures are placed on the muscles and fascia. The mucous membrane is closed with a continuous type suture. At the same time, it is important to constantly monitor the position of the edges of the wound surface, which will prevent the formation of surgical pockets.
Also during the process, it is important to ensure that a roll-like deformation does not form along the edge of the seam, which can cause scarring.
If a median colporrhaphy is performed, it involves the simultaneous application of sutures to the anterior and posterior walls of the vagina, which are aligned with each other.
At the final stage, the vaginal cavity is dried, treated with an alcohol solution and a tampon with a disinfectant is inserted.
Perineoplasty
To select the most optimal method of plastic correction of the intimate area, the patient undergoes a preliminary consultation with a gynecologist. The operation is performed using epidural anesthesia or general anesthesia. The method of anesthesia is determined by the anesthesiologist individually in each individual case.
The duration of surgery is from 60 to 90 minutes. Self-absorbable materials (vicryl) are used for suturing. They allow you to achieve maximum elasticity of the scar without deformation of the perineal tissue.
Recovery period
As a rule, the duration of the rehabilitation period is no more than five days. When using general anesthesia, the patient must be under constant supervision of specialists for one day. If her general health worsens, she is transferred to the intensive care unit.
There will be some soreness in the first few days after surgery. To reduce the severity of discomfort, the attending physician prescribes narcotic and non-narcotic painkillers, as well as non-steroidal anti-inflammatory drugs.
The duration of pain in the perineum, which may accompany the recovery period, will depend on the individual characteristics of the human body and the amount of work performed.
Since the operation is performed under general anesthesia, during the next day after the procedure you need to adhere to a special diet. Only semi-liquid, easily digestible food is allowed for consumption. Over time, the diet can gradually be supplemented with other products.
In general, all patients are prescribed a special diet, which involves preventing the occurrence of increased gas formation and constipation. The menu is calculated in such a way that the first trip to the toilet will generally only be towards the end of the 2nd day.
When performing posterior colporrhaphy with levatoroplasty, it is important that in the first week and a half there is semi-formed stool.
In the first few days after plastic surgery, it is recommended to empty the bladder every two hours. In this case, there may be no obvious urge to urinate, which is often explained by a violation of the sensitivity of the receptors, which is often caused by swelling of the soft tissues. In acute urinary retention, the bladder is emptied using a catheter.
For a week, after each urination, the perineum must be irrigated with antiseptic solutions. This could be Miramistin, Chlorhexidine or Chlorophyllipt. In this case, movements should be performed smoothly without strong mechanical impact. In addition, the seams are treated with antiseptics and anti-inflammatory agents several times a day. After this, a bandage soaked in Levomekol ointment is applied to them.
Also during the rehabilitation period it is necessary to use antibacterial suppositories. If there is a risk of developing complications of an infectious-inflammatory nature, then systemic treatment with antibiotics is carried out.
Sutures are removed approximately on the sixth day after surgery. The patient is discharged no earlier than two weeks later.
In general, full recovery takes about two months. To make this period as successful as possible, it is recommended to follow certain instructions from your doctor.
First of all, constipation should not be allowed to occur, which can trigger the re-development of the pathological process. You should also avoid foods that increase gas formation. Hygienic procedures for caring for the genitals should be carried out regularly. For 10 days you need to douche with a solution of Chlorhexidine.
If intestinal disorders occur, they should be addressed immediately, since diarrhea can cause bacterial contamination and lead to irritation of the mucous membrane.
To prevent the sutures from coming apart, do not sit for the first 7-10 days. After 2 weeks, you can gently squat.
You must abstain from sexual intercourse for 2 months. At the same time, sexual arousal is also not recommended in the first 3 days.
During menstruation, the use of menstrual cups and tampons is not allowed.
You also need to exclude trips to the bathhouse, sauna, swimming pool and solarium.
Complications
Side effects after colporrhaphy in most cases occur due to the fault of a specialist who did not follow the technique of performing the operation. The most common consequences include suture dehiscence and scarring, as well as recurrence of prolapse of the vaginal walls.
Against the background of suture dehiscence, a hematoma or bleeding may begin to develop. In the absence of deviations, discharge is observed for several days. If such a symptom persists for more than four days, you should consult your doctor.
Hematomas are not serious complications and go away on their own after a certain period of time. If it is noted that it begins to increase and is accompanied by painful sensations, then qualified assistance from a specialist will be required.
Septic complications include wound infection. Suppuration provokes failure of the sutures, which can lead to an abscess, lymphadenitis and widespread infection.
Levatoplasty: postoperative period
The period after levatoroplasty with posterior colporrhaphy may be slightly painful due to muscle trauma, but the discomfort is temporary and can be easily relieved with painkillers. The main rule of recovery: after levatoroplasty and colporrhaphy, refrain from sitting at a right angle for up to 7 days and squatting for up to 14 days. This will prevent the seams from coming apart and ensure a good result. Complete rehabilitation takes 2 months, after which you can return to sexual activity.