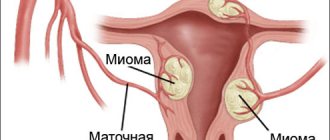
One of the common causes of female infertility is uterine pathology. In some women, this organ is underdeveloped or completely absent. Since it is in the uterus that the gestation of the fetus occurs, in former times a woman with the corresponding problems could not even talk about giving birth to a child. All childless families could count on was adoption.
Uterus transplants have been successfully performed in more than 10 countries around the world.
But today, thanks to the development of medicine, uterine pathologies are not a death sentence. At the same time, there are two approaches to solving the problem of female infertility associated with uterine diseases. The first of them is possible only if the woman has healthy ovaries capable of producing viable eggs. In this case, the fertilized egg is placed in the womb of the surrogate mother, where the fetus develops. This method of dealing with infertility is not suitable for all families. In addition, it is unacceptable for women who have problems not only with the uterus, but also with the ovaries.
Another approach is to transplant a donor uterus that does not have pathological changes. This method allows a woman to bear and give birth to a child herself, and thereby feel like a full-fledged mother. In addition, transplantation can solve the problem of infertility even when surrogacy is not applicable, since today it has become possible to transplant the uterus and ovaries.
When is a uterus transplant needed?
A woman’s inability to conceive, bear and give birth to a child is usually caused by the following reasons:
- Obstruction of the fallopian tubes;
- Congenital anomalies;
- Ovarian dysfunction;
- Absence of certain reproduction organs.
Transplantation of a donor uterus makes it possible to make a woman with similar problems capable of childbearing.
A donor uterus transplant lasts on average 10-12 hours
The main indication for transplantation is the absence of the uterus from birth or as a result of its surgical removal due to cancer, excessive bleeding or septic lesions.
If the uterus was removed due to a malignant tumor, the issue of transplantation must be approached very carefully. After all, a transplant requires the use of immunosuppressants. This weakens the body's protective functions and increases the risk of cancer recurrence.
The congenital absence or underdevelopment of the uterus with formed and functional ovaries is called Rokitansky-Küstner syndrome. This pathology is quite rare and occurs in one in 4.5-5 thousand newborn girls.
What is it for?
Uterus transplantation is one of the ways to combat infertility. In this case we are talking about surgical intervention. During the operation, a donor uterus is transplanted into the body of a woman whose organ has pathologies. If there are problems with it, the patient, as a rule, experiences some difficulties and cannot get pregnant.
Currently, uterus transplantation is considered as an alternative to surrogacy. This kind of surgical intervention allows the fair sex to carry and give birth to a healthy baby themselves.
Possibility of pregnancy after uterus transplantation
A uterus transplant operation is a rather complex surgical procedure, since the transplanted organ has an abundance of nerves and blood vessels that require connection to the patient’s nervous and circulatory system. In addition, the surgical site is difficult to reach for the surgeon.
Uterus transplantation
The main tasks during the operation are:
- Preservation of the anatomical structure.
- Ensuring normal blood supply to the organ.
- Ensuring that the organ can fill with blood is proportional to its increase as the fetus develops.
In a uterine transplant, the fallopian tubes are not brought into the transplanted uterus. This measure reduces the risk of infection of the recipient by pathogenic microorganisms that may be located in the donor organ, but makes it impossible to conceive as a result of natural copulation.
In order for a woman with a transplanted uterus to become pregnant, artificial insemination is used. In this case, the eggs intended for fertilization are removed from the patient’s ovary before the operation and are stored frozen.
The need for such a measure is due to the fact that in the postoperative period and during pregnancy the woman must take drugs that suppress the immune system, otherwise there will be a high probability of transplant rejection. These drugs can negatively affect heredity and cause genetic abnormalities in the unborn child. Preoperative extraction of germ cells eliminates the harmful effects of immunosuppressants on them.
At least a year must pass between the transplantation and the placement of the fertilized egg in the uterus. Only after this period can doctors judge how well the organ has taken root and how ready the patient is to bear a child.
After a uterus transplant, a woman constantly needs drug therapy, which can negatively affect the condition of the body. Therefore, Swedish doctors believe that if the family plans do not include the birth of another child, then it is advisable to remove the transplanted organ after childbirth.
Despite all the difficulties, a number of successful operations have already been carried out in world practice, giving patients the opportunity to become mothers.
First successful uterus transplants
For the first time in the world, a successful uterine transplant followed by the birth of a child was performed by Swedish doctors in 2013. The introduction of this method of solving the problem of infertility into practice was preceded by long-term research by scientists, which showed that a uterus transplant is possible.
The first practical application of the research results was the transplantation of the uterus into nine women in Gothenburg. For five of them, organ donors were their mothers, and for four, women who were closely related to them were organ donors.
Two project participants had to have their transplants removed: one due to blood clots, and the other due to an infectious complication. In the remaining seven women, the transplanted uterus took root. Their own embryos were placed in their transplanted organs.
A successful birth of a child occurred in only one participant in the project - a thirty-six-year-old woman suffering from Rokitansky-Küstner syndrome. Previously, treatment for women with this diagnosis consisted only of ensuring their ability to engage in natural sexual activity. The only opportunity for them to have their own children was to use a surrogate mother.
A participant in the project received a uterus transplant from a friend of hers, an elderly mother of two children who had already passed childbearing age. After organ transplantation, the patient underwent a year of therapy with immunosuppressants and was under constant medical supervision. A sign that the donor uterus had taken root was the appearance of monthly cycles in the patient.
Even before the operation, doctors took eggs from the woman and performed artificial insemination. As a result, eleven embryos were obtained, one of which was subsequently placed in the patient's uterus.
The likelihood that the embryo will take root in the transplanted uterus is less than in a normal situation. Therefore, to increase the chances of success, you must first prepare at least ten viable embryos.
During pregnancy, the woman was at risk of fetal rejection three times, but doctors always managed to prevent pregnancy failure with steroid therapy.
A uterus transplant operation is possible - this has been demonstrated to the public more than once.
At the end of the eighth – beginning of the ninth month of pregnancy, the patient’s condition deteriorated sharply. According to doctors, the reason for this was that the woman was missing one kidney from birth. Therefore, it was decided to resort to a caesarean section. The child born as a result of this operation was quite healthy and weighed about 1.8 kg. This was the first case in world practice of the birth of a living child from a transplanted donor uterus.
The second case of successful uterine transplantation was the transplantation of the uterus of a woman who had died shortly before to a 21-year-old resident of Turkey. Like the Swedish patient, the young Turkish woman had no reproductive organ from birth. When 1.5 years had passed after the operation, Turkish doctors placed an embryo into the transplanted uterus, which appeared as a result of artificial insemination of the patient’s egg with her husband’s sperm. The woman managed to carry and give birth to a child.
In November 2021, the first baby after a uterus transplant was born in the United States. The birth occurred at Baylor University Medical Center in Dallas, Texas. The first 4 uterus transplants in the United States failed, despite the fact that the team included renowned transplant surgeons who had previously trained on animals. The United States performed the first such transplant operation in 2012.
How did the operation take place?
The robotic arms that hold surgical instruments are controlled by two surgeons, one on each side of the patient. Each surgeon sits at a personal workstation a few meters away. Manipulation is performed using a joystick-like tool and a magnified 3D image on a screen, allowing for greater precision when working deep inside the lower abdomen. Toward the end of the procedure, another incision is made so that the uterus can be removed. The donor's uterus is then immediately transplanted into the recipient using open surgery.
“In the future, we will also be able to transplant the uterus using a robot-assisted keyhole technique,”
says Niclas Kvarnström, a transplant surgeon who performs the difficult task of connecting the vessels in the recipient uterus.
Uterus transplantation in Russia and in the world
Among the countries where uterus transplants have ever been performed, Sweden today leads the way. To date, eight organ transplants have been performed in this country with successful pregnancy and birth of a child. Following the Swedes, successful uterine transplantation operations were carried out by Turkish specialists. American doctors and scientists from Saudi Arabia subsequently joined research in this direction.
In addition to these countries, the UK also currently has a license for uterine transplant operations.
Uterus transplantation is not currently performed in Russia. There are no clinical sites or specialists who could perform this procedure.
In Russia, not a single uterine transplant has been performed yet. Russian doctors approach this issue cautiously and believe that it is initially necessary to study all the possibilities of dangerous complications of such a complex and risky procedure. Nevertheless, the beginning of research into the problems of uterus transplantation is included in the immediate plans of Russian scientists, since the number of women in need of such an operation is quite large.
More than 30 uterus transplants have been successfully completed worldwide, including in Brazil, China, the Czech Republic, Germany, Sweden, India, Saudi Arabia, Turkey, and two clinics in the United States.
Medical Features
Penis transplantation is a much more complex task than, for example, kidney transplantation. The organ consists of different tissues: muscles, skin, blood vessels, nerves (Fig. 2). Its transplantation requires a different approach than the transplantation of entire internal organs - vascularized composite allotransplantation (VCA; Fig. 2), in which an entire functional unit with a connection of nerves and blood vessels is transplanted. For example, face or limb transplants fall into this category.
Figure 2. For a penis transplant (especially with a scrotum), a vascularized composite allotransplantation is required , which requires the connection of nerves and blood vessels. This operation required the removal of damaged recipient tissues and the connection of three arteries, four veins, two nerves and the urethra to the donor tissues
Devon Stuart for Johns Hopkins Medicine
VCAs are performed much less frequently than solid organ transplants. Since 1998, the first successful VCA, more than 200 people have received similar allografts [1]. Although today's rare surgeries are successful, they need to be studied more thoroughly in animal models, including the development of safer protocols for the long-term use of immunosuppressive drugs. Ex vivo models for testing drugs on individual cultured tissues of the body are already emerging, such as the work of Nikolai Sopko and colleagues in 2021 [2].
Despite the successes of both conventional (solid organ) transplantation and VCA, the need for immunosuppression remains one of the most important factors slowing progress in this field. According to the American Society of Transplantation (AST), this type of allograft requires not only rapid restoration of blood flow and careful selection of the donor-recipient pair, but also individualized immunotherapy: the transplanted tissues differ in immunogenic and functional characteristics. Statistically, the incidence of acute organ rejection after VCA in the first year is 80%, compared with approximately 10% for renal allografts [3].
In the case of functional unit transplantation, long-term systemic therapy that suppresses graft rejection (translated as graft; editor's note) can lead to diabetes mellitus, nephrotoxicity, osteonecrosis, leukopenia, hypertension, hyperlipidemia, and opportunistic viral and bacterial infections.
If, during a transplantation of, for example, a heart, a person’s life depends on the operation, then it is impossible to objectively answer whether the game is worth the candle in the absence of a penis or uterus: this is not life-threatening. This is due to the ambiguous attitude of doctors and the public towards such a procedure (more on this below). In the end, only the patient himself can decide this for himself. And the doctor can help him make the most informatively informed decision.
Unlike solid organ transplantation, some types of VCA provide a unique opportunity to avoid systemic immunosuppressive therapy by delivering the drug locally to the transplanted organ. Strategies referred to include superficial local and transdermal therapies, subcutaneous injections, and intravascular administration. Naturally, this will help avoid side effects on other organs and the body as a whole. The drug, according to experts, should inhibit such immunological processes as activation of antigen-presenting cells (APC), priming of T-lymphocytes, involvement of B-lymphocytes, transendothelial migration of activated B- and T-lymphocytes and immunological reactions in nearby lymph nodes. In addition, local drugs can prevent ischemic and reperfusion injury to tissues.
Unfortunately, the immediate introduction of these methods into clinical practice cannot be expected, since the effectiveness of local immunosuppression for VCA in clinical settings remains unproven [1].
Immunological certificate
It is immediately worth noting that the general biological processes that occur during VCA largely coincide with those occurring during transplantation of solid organs. Modern methods of immunosuppression cope effectively with their direct task and control cases of acute transplant rejection [3].
But still, VCA has its own peculiarities. The size of the transplanted organ can also influence biological responses. Different tissues respond differently to transplantation: for example, skin is more likely to be rejected than other tissues, while muscles are more sensitive to ischemia and reperfusion injury [4].
Overall, the response to VCA is the result of a complex interaction between innate and adaptive immune responses. These processes are very complex, and we will only focus on their main stages.
Recent evidence suggests that the adaptive immune system senses specific antigens and subsequently activates the innate immune system, increasing the response to the allograft. Of all the VCA components, skin is usually the one that causes the most problems. According to one hypothesis, the skin reacts more sensitively to rejection. However, according to the generally accepted concept, it itself is more immunogenic, and it is precisely because of the molecular processes occurring in it that graft rejection most often occurs. There was even a special term - “split tolerance”, when the musculoskeletal tissue takes root, and the epidermis is rejected [1]. This is another “plus” to the hypothetical use of topical immunosuppressive drugs - fortunately, applying them to the skin will not be a problem [1].
Briefly, innate immune cells, as part of their response to “danger,” recognize damage-associated molecular patterns (DAMPs) that appear in the allograft as a result of transplantation. The release of chemokines and P-selectin recruits leukocytes to the transplant site. Attracted macrophages in turn produce proinflammatory cytokines: IL-1 and IL-6, which potentiate the antigraft response and recruit antigen-presenting cells into the response. Theoretically, the innate response will be activated (albeit to a lesser extent) even if the genome of the transplanted organ cells matches the DNA of the recipient - due to molecules released during surgery and "danger" signals [3].
Many immune processes in vascularized composite allotransplantation overlap with inflammatory conditions of the skin. The main participating cells are endothelial cells of the dermis and dermal APCs with keratinocytes. The latter, unlike other allograft cells, express the major histocompatibility complex (HLA class two) and activate T lymphocytes during inflammation. The unique innate response of skin-containing VC allografts is also associated with cutaneous alarmins, molecules from the DAMP group. They are generated endogenously by keratinocytes and resident leukocytes of the skin after various stresses.
Intuitively, one can assume that it is the recipient’s immune cells that reject the allograft. However, there is evidence that in the case of VCA this is not entirely true: the donor’s skin cells, according to the results of studying biopsies after transplantation, also contain many immune cells. Such “transplanted” foreign cells can also influence rejection [4].
Uterus donation: the ethical side of the issue
Like all organ transplant operations, uterine transplantation requires legal regulation. The procedure requires the mandatory presence of a donor, and therefore the question of its admissibility is morally ambiguous. That's why some countries prohibit this type of surgery.
In states where uterine transplantation is permitted, different approaches to the issue of uterine donation are practiced. Swedish doctors are proponents of using living women, preferably relatives of the patient, who voluntarily agreed to donate their organ, as uterine donors.
American doctors, on the contrary, consider it acceptable to take a uterus for transplantation from deceased women. However, in practice, attempts to use a corpse as a donor, as a rule, did not lead to positive results due to infectious complications that arose.
In Muslim countries, only living organ transplants are allowed.
To resolve the issue of uterus donation from living people, in 2013, the Canadian city of Montreal adopted criteria according to which a person can act as a donor or recipient of an organ. Their essence is as follows:
- The woman acting as the recipient must be genetically female. She must have no medical contraindications to organ transplantation and other types of infertility treatment have not given the desired results. In addition, she must not agree to such methods of solving the problem as using a surrogate mother or adopting a child. She must also not have any factors limiting her rights to motherhood (mental disorders, drug addiction, etc.). A woman who decides to undergo a transplant must be aware of the need for treatment and all the risks and possible consequences of the operation.
- A woman of childbearing age who does not plan to have any more children can act as a donor. The use of the wombs of deceased women is permissible only if they have their consent to this, legally recorded during their lifetime.
A necessary condition for the ethics of uterus transplantation is full consent to the procedure, both on the part of the donor and on the part of the recipient of the uterus.
From the history of the issue
Over the past hundred years, medicine has not only stepped forward, it has literally soared to previously unimaginable heights.
Just think - the first human-to-human organ transplant was performed less than 100 years ago, in 1933. The first kidney successfully changed hands in 1954 when, thanks to J. Murray, one twin brother shared his kidney with the other. 2 years later, in 1956, Thomas Starzl successfully transplanted a liver, and 10 years later, Christian Barnard performed the first successful heart transplant. In 1983, doctors learned how to transplant lungs.
Why did research into the possibility of uterus transplantation begin only at the end of the twentieth century?
It’s simple: if a person cannot live without a heart, liver, lungs, at least one kidney, then without a uterus this is quite possible; it is not a vital organ. And it is located in such a way that it is difficult to carry out the operation. And the functions of this organ are very complex: not only does the uterus need to take root, it is necessary that a human embryo can develop normally in it.
Therefore, when in 1998, in one of the Gothenburg hospitals, a patient with a uterus removed due to cancer asked doctors about the possibility of transplanting a new uterus to her, doctors perceived her idea as completely crazy. But after a year, research was very active. And last year, 2021, the first child born in a transplanted uterus was born in Sweden.
9 women were selected for the first operations. All donor organs were obtained from living donors, 5 of whom were mothers of recipients, the rest were relatives or friends. 2 uteruses had to be removed soon, as complications began. The first mother was a Swedish woman who received a uterus transplant from her close friend. The baby was born at 31 weeks via caesarean section. The baby weighed only 1800 g, but immediately screamed and was quite viable. After 10 days, the happy mother and baby were discharged home; the child is developing normally.
By the end of 2021, Swedish doctors expect several more children to be born. Another woman with a transplanted uterus underwent an IVF procedure in Turkey, and the pregnancy has so far proceeded without any particular complications. UK doctors have received permission to perform a uterus transplant, and preparations are underway for similar operations in the USA. They even say that in a few years the uterus will be able to be transplanted not only into women, but also into men.
How much does a uterus transplant cost?
Due to its complexity, uterus transplantation is a very expensive operation. In Sweden, for example, its price is about one hundred thousand dollars. Using a surrogate mother is much more affordable - it costs no more than thirty thousand dollars, taking into account payments to doctors and the cost of necessary medications.
The cost of uterus transplant in India is approximately US$18,000-20,000 while the cost in US. close to $70,000. The duration of the procedure is about 12 hours.
Uterus transplantation actually offers hope to thousands of infertile women. Scientists and governments must work together to make this procedure available to everyone who needs it.
Share link:
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Skype (Opens in new window)
- More
- Click to print (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share posts on Tumblr (Opens in new window)
- Click to share posts on Pocket (Opens in new window)
Similar articles on the topic of transplantation
- Lung transplant: indications, cost.…
- Kidney transplant: operation, cost
- Egg (oocyte) donation: cost, consequences
- Pancreas transplant in Russia: price
- Donor Day in Russia in 2021
- Donor Day in Russia in 2021
First Person: First American Recipient
The patient, who became a penis and scrotum recipient in 2018 at Johns Hopkins University, wished to remain anonymous. It is only reported that his loss of an organ is related to military service.
Tom Manning, the first American patient to receive a penis transplant at Massachusetts General Hospital several years ago (his quote practically opened the article); does not hesitate to talk about himself and his history of failures. Or, as he now believes, on the contrary, stories of success. Because everything could have been much worse.
In 2012, Tom had no idea that he would become famous throughout the world. It was his usual working day. Suddenly he slipped while unloading boxes and knocked over a heavy cart of papers. Despite the blood, pain in the groin area and swelling of the genitals, he did not go to the doctor - neither that day nor for the next two months. Eight weeks later, Manning finally sought medical help - but in addition to the injury, he was also diagnosed with penile cancer, which led to a penectomy.
Curtis L. Cetrulo, a specialist in plastic and reconstructive surgery, and Dicken Ko, a urosurgeon working at Massachusetts General Hospital, had long been passionate about the idea of a penis transplant. This was prompted by cases of combat injuries to the genitals received by American soldiers in Iraq and Afghanistan. At the same time, Johns Hopkins University was also planning to perform a penile transplant. Primacy depended only on who could be the first to complete all the necessary approval processes for the operation and find a suitable donor and recipient pair.
By the time of the transplant, Tom Manning had been living with an amputated penis for more than four years, and although doctors could not guarantee the complete success of the operation, he still took a risk. Thirteen surgeons participated in the fifteen-hour transplant (Fig. 4). The result was successful - doctors described it in a 2021 publication [14]. Within six months after surgery, Tom regained penile sensitivity, partial erectile function, and urination [7]. The side effects of immunosuppressant drugs can be frustrating, but Tom Manning remains optimistic. He told Esquire magazine that if he had a date with a sequel, the first thing he would do would be to run to call Ko and Cetrulo, shouting, “He's come to life!” In addition, the patient was already wondering whether the woman with whom he shared a bed would be considered to be sleeping with two men at the same time: with himself and with the donor?
Figure 4. Medical team from Massachusetts General Hospital
This is the story of America's first penis transplant
Doctors are confident that such a phenomenon as the loss of the penis should not be kept silent. Only openness will allow society to understand the need for the operations being carried out and change the skepticism and rejection that exists in the public consciousness. Patients who have undergone a successful penis transplant are unanimous in their opinion: they need the penis for a normal life. “This is a terrible injury. […] When I woke up [after the operation], I finally felt normal again,” is how the recipient of the penis and scrotum put it in a press release. Johns Hopkins University even organized a symposium in 2014 about military victims who lost their genitals in service. The problem was discussed not only with the victims, but also with their relatives and medical workers. The topics of self-perception as a person, self-esteem and personal relationships were raised.
“This surgery has the potential to change lives,” Dr. Richard Redett said in an interview. “If you meet a soldier like our patient and learn his story, you will understand why we did the transplant.”