Causes of retrocervical endometriosis
Retrocervical endometriosis is the spread of endometriotic tissue along the rectovaginal tissue (the space between the rectum and the posterior wall of the vagina and cervix).
The cause of the disease has not been fully established.
According to the embryonic theory, the rudiments of endometrioid cysts in various tissues and organs are formed in the prenatal period as a result of disruption of tissue differentiation processes. Also, the implantation mechanism of the occurrence of retrocervical endometriotic growths is not denied - the reverse flow of menstrual fluid into the uterus and abdominal cavity.
The following risk factors predispose to the development of retrocervical endometriosis are identified:
- Operations and diagnostic manipulations on the cervix and body of the uterus (diagnostic and therapeutic curettage, various methods for examining the patency of the fallopian tubes, abortions).
- Difficult childbirth, accompanied by cervical ruptures.
- Chronic inflammation (vaginitis, cervicitis, endometritis) of various etiologies.
- Diseases accompanied by disruption of the hormonal function of the ovaries (tumors, inflammation of the appendages, polycystic ovaries, pathologies of the hypothalamus and pituitary gland).
- Autoimmune diseases.
- Family history of endometriosis.
How to eliminate pain with endometriosis
Pain from endometriosis can be eliminated after the disease has been cured or stable remission has been achieved. Patient management tactics depend on the location of the pathology, severity, age and other factors, and therefore are developed on an individual basis.
For grade 1-2 endometriosis, drug therapy is most often used, in particular hormonal drugs, which, when properly selected, reduce or completely eliminate the pain response. Also, the patient may be additionally prescribed sedatives, painkillers, antispasmodics and restorative drugs. Surgical interventions performed to remove endometriotic lesions also help restore organ function and lead to the disappearance of adverse symptoms.
Pathogenesis
An important role in the development of retrocervical endometriosis is played by hormonal imbalance and disruption of the immune system. Elevated levels of estrogen enhance the growth of the endometrium in cysts, while reduced immunity cannot recognize pathological cells and destroy them.
The spread of endometrioid cells from the primary focus is carried out through blood and lymphatic vessels, as well as by contact. Pathological formations have receptors for sex hormones, so the symptoms intensify during menstruation - the endometrium in cysts, just like in the uterus, is rejected, and hemorrhages occur in the cystic cavities.
The main signs of endometriosis of the uterine body
The first sign of this disease is heavy and extremely painful menstrual bleeding, as well as intermenstrual bleeding, which can also be quite significant. In some cases, endometriosis of the uterine body is congenital. In such a case, pain in the girl’s lower abdomen may appear approximately two to three years before the onset of her first period. And the first menstruation is often accompanied by heavy bleeding. The presence of congenital endometriosis can be suspected if the mother has this disease or in the case of abnormal development of the genital organs in a girl (for example, if the structure of the uterus is abnormal).
Classification
To determine the stage of retrocervical endometriosis, the depth and area of the lesion are determined. This classification allows you to choose the optimal treatment tactics and give the most accurate prognosis for recovery and the development of complications. The following stages of retrocervical endometriosis are distinguished:
- Pointed endometriotic formations in the rectovaginal tissue without cyst formation.
- The formation of small endometrioid cysts in the cervix and vagina.
- Damage to the ligamentous apparatus of the uterus, transition of the process to the rectum.
- Multiple cysts affecting the intestinal mucosa, ureters, peritoneum and causing adhesions.
Symptoms of retrocervical endometriosis
The first stage of endometriosis of the retrocervical region can occur without pronounced symptoms. As the endometrium grows in the rectovaginal tissue, a characteristic clinical picture develops.
The main complaint made by patients with endometriosis of this localization is pain. Aching or cramping pain occurs in the sacrolumbar region and radiates to the rectum, perineal area, and genitals. In this case, the maximum severity of the syndrome is observed during menstruation and during sexual intercourse. After sex, it is not uncommon to experience slight bleeding from the vagina.
When endometrioid tissue grows into the rectum, pain occurs during bowel movements. This often causes constipation. During menstruation, bloody discharge may appear from the anus.
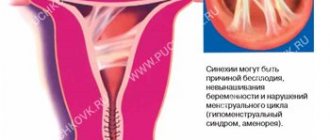
With the retrocervical form of endometriosis, spread to the peritoneum and appendages, infertility occurs. It is associated with adhesive deformation of the fallopian tubes and damage to the ovaries.
Endometriosis turns into cancer - prevention of degeneration
It is important to understand that any cystic neoplasm in the area of the uterine appendages is an indication for a thorough and attentive examination: one cannot be sure of the absence of oncology until a histological examination of a biopsy from the tumor is done. Even if the ultrasound examination and CA-125 level are encouraging. Really working preventive measures include:
- Tubal ligation, which prevents menstrual blood from entering the uterine cavity into the appendage area;
- 2 or more babies born;
- Long-term breastfeeding (up to 1.5 years);
- Long-term use of hormonal contraceptives (at least 5 years).
You need to be especially careful in relation to women who have blood relatives in the family with cases of severe forms of endometrioid disease or ovarian cancer. When the duration of endometrioid disease is more than 10 years and when the disease worsens in patients aged 45 years and older. It is better to carry out an additional examination than to miss carcinoma: endometriosis rarely turns into cancer, but malignant degeneration occurs where there are favorable conditions for this.
Complications
Regular hemorrhages in retrocervical endometrioid cysts and their damage during sex and bowel movements leads to anemia. Its main symptoms are:
- Weakness.
- Dizziness.
- Frequent fainting.
- Dry skin, brittle nails and hair.
- Perverted appetite - the desire to eat earth, ice, chalk, starch.
Retrocervical endometriosis, which extends to the rectum, causes constipation and, in severe cases, mechanical intestinal obstruction. This condition requires mandatory surgical intervention.
Endometriotic growths are the cause of female infertility in more than 30% of cases.
When the peritoneum is damaged, adhesions occur that affect the uterine appendages. Also, the development of endometrioid cysts in the ovaries damages the follicular apparatus of the glands, which disrupts the processes of egg maturation.
Chronic pelvic pain and dyspareunia seriously impair the quality of life of women suffering from retrocervical endometriosis. This leads to psycho-emotional disorders, depression, and in severe cases, suicidal intentions.
Pathological growths of the endometrium can become a background for cancer. Transformation of retrocervical endometrioid cysts into clear cell and endometrioid carcinomas occurs in 0.6-11.4% of cases.
Localization of pain in endometriosis
Endometriosis, depending on the location of the lesions, is divided into internal and external, genital and extragenital. Forms of the disease are accompanied by pain of a different nature:
- Pain in uterine endometriosis (adenomyosis) is cramping and highly intense, it is felt constantly, is located in the lower abdomen and spreads to the lumbar and pelvic area;
- Pain due to ovarian endometriosis varies in intensity during menstruation and is often accompanied by nausea and vomiting. Rupture of an endometrioid ovarian cyst causes severe and acute pain and threatens the patient’s life;
- Pain with vaginal endometriosis is the most severe and causes maximum discomfort. If the lesions damage only the superficial layers, then the pain reaction is moderate, but in advanced cases it becomes more intense. If the wall adjacent to the bladder is involved in the process, then the pain may intensify when urinating. The condition also worsens during sexual intercourse and gynecological examination;
- Pain in extragenital endometriosis is associated with intestinal obstruction, damage to the nerve plexuses, irritation of the peritoneum and retrocervical space. They are diffuse in nature, but can be clearly localized. They often form a picture of an “acute abdomen,” causing difficulties in diagnosis.
It is worth noting that pain, menstrual irregularities, and hormonal disorders are always signs of gynecological diseases. It is very important to promptly identify the existing pathology and begin treatment, as this will not only eliminate unpleasant symptoms, but also prevent serious consequences. You can undergo a full examination of the body at the IVF Center clinic in Kursk.
Diagnostics
The initial step in diagnosing the retrocervical form of endometriosis is a gynecological examination. When visualizing the cervix, bluish endometrioid lesions are observed in the mirrors, which begin to bleed upon contact with them. Soft elastic formations can be felt by palpation in the posterior fornix. Mobility of the uterus and appendages is difficult.
To clarify the localization of lesions and the extent of the process, an ultrasound examination of the pelvic organs is performed. Heterogeneous round cysts of various diameters with uneven contours are visualized. To detect endometrioid growths on the uterine ligaments, rectum and pelvic walls, additional computed tomography or magnetic resonance imaging (CT, MRI) is performed.
Important! If you suspect involvement of the rectum in the process, a consultation with a proctologist is required. The doctor first palpates and then uses endoscopic methods (sigmoidoscopy, colonoscopy) to determine the degree of damage to the intestinal mucosa and rectovaginal tissue.
Laparoscopy allows detection of dissemination of endometrioid cysts throughout the peritoneum. During the operation, it is possible to remove pathological areas and dissect adhesions.
Is scraping a necessary procedure or an anachronism?
“I was cleaned or I had a cleaning done” - I often hear this phrase from my patients, and it sounds to me as unbearable as the movement of foam plastic on glass.
We colloquially call “cleaning” “uterine curettage” - the most common procedure performed in gynecology in the vast majority of cases without any indication for it.
In our country, where “gynecological paramedicism” prevails, scraping is the main primitive tool for conducting “medical activities.” I will make separate material on the topic of “gynecological paramedicism,” but for now I will briefly explain this term.
“Paramedicism” refers to “treatment” based on the principle of “a pill for the head, a pill for diarrhea,” that is, a lack of knowledge about the nature of the disease, its features and nuances of its course, and, as a result, the inability to take a differentiated approach to treating the patient. Actually, according to history, paramedics came from barbers who did not heal, but bled and set dislocations.
The very name “purge” that has taken root reflects a rough, clumsy and primitive approach to solving the problem.
By the way, the term smoothly passed from medical jargon into the vocabulary of many women who even believe that they need to “get clean” or “get clean” from time to time.
Perhaps they put the same meaning into this as into the notorious “cleansing the body of toxins”, suggesting that “dirt” accumulates in this organ too...
Before continuing the story, it is necessary to explain what exactly we are talking about.
Curettage is an outpatient medical procedure performed under intravenous anesthesia, during which the uterine mucosa is removed (scraped) using a special curette.
The procedure is called therapeutic and diagnostic because it removes disease-modified tissue (if any), which can be examined under a microscope and an accurate diagnosis made.
From the previous sentence it is clear that curettage is carried out not only in the presence of a disease, but when it is suspected, that is, for the purpose of making a diagnosis.
So far everything is clear, logical and obvious. However, there is another side to this manipulation. The procedure is performed with a sharp iron curette, with the help of which the mucous layer of the uterus is actually “torn off” and inevitable injury to the uterus itself occurs.
As a result, there is a risk of several serious complications: damage to the growth layer of the endometrium (impairing its growth in the future), the appearance of adhesions in the cavity, and the development of inflammation.
In addition, this procedure contributes to the development of diseases such as adenomyosis (endometriosis of the uterus), due to the violation of the boundary between the layers of the uterus, which contributes to the growth of the endometrium into the muscle of the uterus. As a result, undergoing curettage can lead to problems with conception or trigger the development of adenomyosis.
It is quite obvious that such a procedure must be done strictly according to indications and the benefit-risk ratio must be seriously assessed. But this is possible anywhere, but not here, and this is very sad.
I think that in more than 80% of cases, curettage is carried out in vain, that is, either without any indication at all or in cases where the problem can be solved with medication or through a simple outpatient procedure.
Here are situations in which you may be asked to perform curettage:
- You have been bleeding for a long time or have had uterine bleeding
- During an ultrasound, you were discovered to have an endometrial polyp, endometrial hyperplasia, adenomyosis, uterine fibroids and chronic endometritis
- You are planning to undergo surgical treatment for uterine fibroids
- You suspect an ectopic pregnancy
- You complained that you have heavy menstruation, intermenstrual spotting or brown spotting before and/or after menstruation.
In general, people are sent for “cleaning” very often, even in the absence of the reasons that I listed above. Curettage often accompanies any surgical treatment in gynecology. It’s as if they are always trying to do it “at the same time” in order to “check, just in case,” whether everything is normal. It shouldn’t be this way; this is too frivolous an attitude towards a rather traumatic procedure.
So, instructions on how to avoid scraping.
- If you do not have heavy uterine bleeding (as they say = pours down your legs), but just prolonged bleeding and pregnancy (uterine and ectopic) is excluded, check with your doctor about the possibility of stopping the bleeding with medication. Yes it is possible. While taking the drug (I will immediately warn you that this is a hormonal drug, but it is safe), the bleeding may stop and your condition will need to be re-evaluated after the next menstruation. In many cases, the treatment provided will be sufficient and nothing more will need to be done.
- If during an ultrasound you are found to have a polyp or endometrial hyperplasia, do not rush to agree to curettage. Ask the doctor about the possibility of prescribing the drug for you in this cycle and then repeat the ultrasound after the end of the next menstruation - if a polyp or hyperplasia is confirmed - alas, curettage under the control of hysteroscopy must be done, but you have a very high chance that after menstruation there are no indications for the procedure will.
- A little about polyps and hyperplasia: a polyp is a growth on the mucous membrane of the uterus (looks like a finger or a mushroom), most often benign. There are polyps that are rejected during menstruation and those that grow from the germ layer. The latter require removal. Hyperplasia is a thickening of the mucous membrane of the uterine cavity. There are two types: simple and complex. “Simple hyperplasia” occurs most often, it is not dangerous, for its development there must be a mandatory reason (a functional cyst in the ovary, polycystic ovary syndrome and several more). Usually, 10 days of taking the drug is enough for it to go away and not recur. “Complex hyperplasia” is bad hyperplasia, an error in the structure of the endometrium, usually occurs after 35 years, more often against the background of excess body weight, is treated initially by removal of the mucous membrane (curettage) and then by a multi-month course of hormonal drugs or by installing the Mirena intrauterine hormonal device. An accurate diagnosis is only possible with histological examination.
- If you are offered to have it scraped only for diagnostic purposes before surgery or to clarify the condition of the mucous membrane, ask the doctor to start with an “endometrial biopsy” (another name is “pipe biopsy” or “aspiration biopsy”). This is a simple outpatient procedure that does not require any anesthesia. A thin tube is inserted into the uterine cavity and a small amount of tissue is sucked in, which is then sent to the laboratory for examination. This is a fairly informative analysis. It is important that the material obtained as a result of curettage or biopsy is only the mucous membrane of the uterus, that is, it does not carry any information about other diseases. The fact is that curettage is often prescribed for the purpose of assessing uterine fibroids for its characteristics - so, curettage will not provide any information.
- Remember, almost all modern ultrasound machines allow you to evaluate the uterine mucosa and identify signs of pathology in it. If the doctor writes during an ultrasound that the endometrium is not changed, and you do not have heavy menstruation or intermenstrual bleeding, the likelihood that you have a pathology that requires curettage is close to zero
- In general, the main manifestations of endometrial pathology (curettage is aimed only at this tissue) are bleeding, heavy menstruation and intermenstrual spotting. That is, if you don’t have this, discuss with the doctor how justified his desire to perform curettage is.
- “Chronic endometritis” is a common diagnosis with ultrasound and in the results of histological findings after curettage. We are talking about “chronic inflammation of the uterine mucosa.” So, in the West there are no generally accepted criteria for making this diagnosis using ultrasound. Simple histology also cannot reliably confirm this diagnosis. Often, with overdiagnosis, this diagnosis is made where it does not exist, since they focus on “leukocytes”. A reliable diagnosis is possible only by conducting a special type of study - immunohistochemistry. This test is not available in all laboratories. Yes, and the material for it can be obtained by biopsy, rather than by curettage. I think it’s now clear that curettage is not necessary to confirm the diagnosis of “chronic endometritis.” In general, treatment and diagnosis of this endometrial disease makes sense only within the framework of the problem of infertility and miscarriage.
In what situations should you agree to scraping?
- Severe uterine bleeding - yes, curettage is a way to stop it
- Suspicion of ectopic pregnancy (difficulties in making a diagnosis)
- Polyp or endometrial hyperplasia that did not disappear after menstruation (drug treatment)
- Remains of the membranes (after abortion, miscarriage, pregnancy)
- Any spotting after menopause
Now I hope you have reliable instructions on how to avoid a possibly unnecessary operation for you. Don't be afraid to ask your doctor questions. Offer alternatives (endometrial biopsy, medication).
Ask to justify the need for curettage. The answer “that’s how it’s done here” is not worth accepting.
Of course, all this applies only to those situations in which there is no threat to your life and health (excessive bleeding).
Source: https://www.sovetginekologa.ru/blog/vyskablivanie-neobhodimaya-protsedura-ili-anahronizm/
Treatment of retrocervical endometriosis
The main goals of treatment for retrocervical endometrioid cysts are: restoration of reproductive function and improvement of the patient’s quality of life. The most effective is considered a combined approach to treatment, i.e. combined use of medical and surgical methods for eliminating endometriosis.
Conservative therapy
The basis of drug therapy for endometriotic growths is the prescription of hormonal drugs. Their long-term use suppresses the production of their own sex hormones in the ovaries. This stops the growth and spread of endometrioid tissue and suppresses its cyclic changes. After surgical removal of pathological growths, hormones are used as a means of preventing relapses. Drugs prescribed for hormonal treatment include:
- Combined oral contraceptives.
- Synthetic progestins.
- Antigonadotropins.
- Gonadotropin releasing hormone agonists.
For the symptomatic treatment of retrocervical endometriosis, anti-inflammatory drugs (Diclofenac, Nimesulide), hemostatic agents (etamsylate, tranexamic acid) and iron supplements are used to treat anemia.
Prevention of adhesions is carried out by prescribing enzyme preparations. Wobenzym and Longidaza prevent the formation of adhesions in the abdominal cavity, reducing the consequences of retrocervical endometriosis for a woman’s reproductive health.
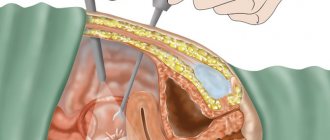
Surgery
When endometrioid cysts are located retrocervically, conservative and radical operations are performed using laparoscopic access. Organ-preserving interventions involve excision of areas of affected rectovaginal tissue and dissection of peritoneal adhesions. Such operations are performed on patients of reproductive age with a non-advanced form of the disease.
In case of total damage to the pelvic organs, radical operations are performed: hysterectomy or total hysterectomy, rectal resection. They do not preserve a woman’s reproductive function, but eliminate the symptoms of the disease, significantly improving the quality of life.
Principles of hormonal therapy for internal diffuse endometriosis
The most effective treatment for endometriosis is hormonal therapy. Drugs used to treat endometriosis can temporarily stop the activity of endometrial cells. However, this method of treatment has a significant disadvantage, which is its duration. However, the use of such therapy makes it possible to completely restore the functionality of the functional layer of the endometrium without surgical intervention (although in some patients conservative therapy remains ineffective).
Features of the effect of hormonal therapy on the body of a woman suffering from diffuse endometriosis are:
- It is worth noting that hormonal imbalance is one of the main provoking factors that adversely affect a woman’s health. Hormonal therapy is aimed at stabilizing the concentration of hormones and keeping them from levels under the supervision of a specialist.
- Only the use of hormonal drugs will help achieve the necessary positive dynamics. The fact is that endometrial cells work cyclically. Therefore, in the absence of ovulation and menstruation, they are in a state of rest.
- If endometrial cells do not fulfill their functional purpose, they gradually begin to decrease in number. In the absence of a nodular form of the disease, the female body can independently cope with the pathology.
- As a rule, the use of hormonal therapy in patients of reproductive age lasts no more than six months. However, in some situations it may be extended.
The main thing is to remember that the selection of drugs and dosage is carried out individually, so any adjustments to the treatment plan should be discussed with the attending physician.
Prognosis and prevention
The prognosis for retrocervical endometriosis is favorable. Complete restoration of reproductive function is possible if the disease is detected in the first and second stages and complex treatment using surgical methods and hormonal therapy. In case of severe disease in pre- and postmenopause, radical surgery is recommended to eliminate all symptoms and prevent relapses.
There is no specific prevention. To prevent the development of retrocervical endometriosis, it is recommended to abandon unnecessary diagnostic interventions on the body and cervix of the uterus and uterine appendages. Timely treatment of inflammatory processes in the reproductive system will help reduce the risk of its occurrence. Regular gynecological examinations and ultrasound of the pelvic organs can identify retrocervical foci of proliferation of endometrioid tissue at an early stage.
Features of the procedure
The first stage of treatment for pathology is taking hormone-containing drugs that cause medicated menopause. As a result, eggs are not formed and further growth of the endometrium stops.
Curettage of the uterus for endometriosis is done if hormonal therapy does not bring results within six months. Various methods are used. The most popular is laparoscopy - the most non-traumatic type of intervention, during which electrocoagulation or laser is used. This procedure is always performed under anesthesia, as it is very painful.
Surgical curettage is used if heavy bleeding is observed or an infiltrative form of pathology is diagnosed. A total hysterectomy is often performed to remove the ovaries to prevent recurrence of endometriosis.
Preparation
Before the endometrial curettage procedure, preparatory measures are necessary:
- Pelvic ultrasound and other ultrasound diagnostic methods;
- blood test for tumor markers (CA-125);
- hysteroscopy;
- determination of hormonal status.
Also, before cleaning, a woman is recommended to avoid intimacy for at least three days, use neutral baby soap as a cleanser for intimate organs, and avoid vaginal suppositories and douching.
Immediately before the procedure, it is necessary to refuse water and food to reduce the likelihood of nausea and vomiting during anesthesia.
Carrying out the procedure
The operation is performed in a hospital on a regular gynecological chair. In most cases, general intravenous anesthesia is used. After complete anesthesia, a vaginal wall dilator is used, which maximizes the lumen and makes the cervix accessible for visualization.
The cervix is supported using a surgical instrument, and a probe with a rounded end is inserted into it. It expands the canal, which is necessary for examining the inner layer of the mucosa with a hysteroscope.
Cleaning is carried out in two stages:
- The surface of the cervical canal is cleared of accumulated mucus. In the second phase of the cycle, the secretion acquires a thick and viscous structure, which can make inspection difficult. Various thinning solutions are used for cleaning. The uterine cavity is treated in the same way.
- Curettage is performed - scraping. The tool for this manipulation resembles a spoon with a thin long handle. A curette is used to clean off the top layer of the uterine mucosa, which is transferred to a prepared sealed container. The tissue will be sent to the laboratory for histological examination.
The whole procedure takes no more than 20 minutes. Additionally, other surgical procedures can be used - dissection of synechiae, fibroids, polyps. The operation is scheduled immediately after the end of the critical days. It is during this period that hypertrophied foci of the mucous membrane are most pronounced.
The procedure is carried out before menstruation and at any period of the cycle only as an emergency in case of heavy bleeding.
Postoperative rehabilitation
To exclude possible complications after surgery, antibacterial drugs are prescribed, and, if necessary, hemostatic agents. Menstruation after curettage begins 20–30 days later. If menstruation after curettage does not occur after this period, a transvaginal ultrasound is performed to determine the cause.
Pathologically scanty or abundant discharge after curettage is a reason for a visit to the doctor. You should also be wary if they acquire an unusual odor, a yellow or green tint, or if there are inclusions of clots.
If no complications arise during cleaning, the woman can return to her normal life after a week. In the first days, pain and bleeding may be observed, the volume of which will gradually decrease. Sexual intercourse after cleansing is prohibited for 10–14 days. Physical activity, the use of intravaginal products and douching, the use of a hot bath, shower, visiting a bathhouse, hypothermia are also not recommended