Vaginal sanitation is a procedure for treating the external genitalia with antiseptic drugs. Such manipulations are carried out for various indications. The procedure is prescribed by the attending physician. At the same time, sanitation in gynecology is part of anti-inflammatory therapy. In some cases, such procedures are performed before surgery.
Is rehabilitation really necessary?
Modern technologies make it possible to produce more effective drugs to combat many diseases. However, the number of women suffering from vulvo-vaginal diseases does not decrease every year. As statistics show, almost 2/3 of patients who seek help from specialists have pathogenic microflora of a mixed nature. In this case, an integrated approach is required in the treatment of inflammatory processes.
What is rehabilitation? In gynecology, during pregnancy and some infectious diseases, the external genitalia is treated. This eliminates the possibility of pathogenic microorganisms penetrating the woman’s reproductive organs. For the treatment of infectious diseases with mixed microflora, several drugs are used at once.
How long does treatment last?
Therapy can last up to 3 weeks. First you need to destroy the pathogenic microflora and relieve inflammation. After this, the vagina is seeded with bacteria that benefit the female body. For this purpose, probiotics are used, which include bifidobacteria and lactobacilli. These medications can be taken orally. With bacterial vaginosis, many women may experience intestinal dysbiosis. If it is not cured, the inflammatory process in the vagina may begin again.
One of the procedures often used in gynecology is therapeutic and preventive sanitation.
The high prevalence of vulvovaginal infections and the difficulties of diagnosing mixed forms of the latter determine the “popularity” of this manipulation.
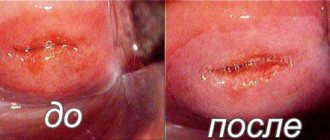
The essence of the method is to treat the vagina and cervix with antiseptic agents or other means.
The goal is to eliminate pathogenic microorganisms.
During research
Sanitation in gynecology is used to prepare organs for certain studies that involve penetration into the uterine cavity. This allows you to avoid inflammatory processes. This preparation is carried out before:
- oncocytology;
- colposcopy;
- hysteroscopy.
In addition, the procedure is carried out before any type of surgical intervention, as well as before the introduction of an intrauterine device.
Preparation
Before sanitizing the vagina, a woman must undergo a full range of all necessary examinations. First, you need to establish the nature of the process that has arisen in the organs of the reproductive system and assess all possible risks. Doctors recommend the following tests, such as:
- a blood test to determine the presence of antibodies to certain infections, as well as markers of inflammation;
- urogenital smear for microflora;
- collection of cells from the cervix to determine the presence of possible oncological pathologies;
- analysis of secretions;
- polymerase chain reaction;
- examination of the walls of the vagina and cervix using a special magnifying device - a colposcope.
Sanitation during pregnancy
If there are certain medical indications, sanitation can be performed during pregnancy. Most often, the procedure is prescribed when a urogenital infection is detected. Sanitation is especially relevant in cases where there is a high probability of pathogenic microorganisms entering the uterine cavity. This kind of treatment can be carried out even in the early stages of pregnancy.
It is worth noting that in the third trimester, at approximately 35-36 weeks, the candida fungus begins to actively multiply in a woman’s vagina. During this period of pregnancy, the use of systemic drugs is contraindicated, as they can damage the birth canal and also cause swelling of the mucous membranes.
However, a woman must get rid of thrush. Otherwise, when the baby passes through the birth canal, infection may occur. It is for this reason that sanitation is carried out before childbirth. The procedure is carried out as a therapeutic manipulation.
Sanitation is carried out on an outpatient basis using proven medications and sterile instruments. At the same time, a comfortable environment is created for the pregnant woman.
How to do it
If you are diagnosed with a genitourinary infection shortly before giving birth, you should not panic. There are many effective means for sanitizing the vagina. They should be selected exclusively by a doctor after accurately establishing the species of the pathogenic microorganism. The optimal time frame for this is considered to be 34-35 weeks.
pregnancy. Drugs used for sanitation usually have a local effect on infectious agents. The use of suppositories for sanitizing the vagina and vaginal tablets is especially popular:
- The drug terzhinan is very effective against many pathogenic microorganisms. It is used for fungal and bacterial infections of the genitourinary organs;
- Hexicon has an antiseptic effect, but is ineffective against fungal infections of the genitals;
- Polygynax is used to combat candidiasis and inflammatory processes in the vagina of various etiologies;
- Fluomycin is considered a very effective drug against various pathogens, including fungal ones. Available in the form of vaginal tablets;
- Sanitation of the vagina with miramistin is effective against a wide range of microorganisms (fungi, viruses, bacteria, protozoa). The drug also has a local immunostimulating effect on the vaginal mucosa;
The medicinal substances included in the above drugs act quickly and effectively. During vaginal sanitation, it is necessary to use drugs that restore the natural microflora of the vagina.
It is important to strictly adhere to the doctor's instructions. If a woman has an infection with severe clinical symptoms, then she should not stop taking the medications on her own immediately after the main manifestations of the disease go away.
Typically, complete sanitization of the vagina before childbirth requires 1-2 weeks.
Sometimes a pregnant woman may need to have an obstetric pessary installed. This is necessary if there is a risk of premature birth. If a woman has a pessary installed, then she needs especially careful monitoring, since an obstetric pessary is a foreign object in the internal environment of the body, and it increases the risk of infectious pathology. Sanitation of the vagina with a pessary involves the need to take a smear for flora every 2 weeks and, if indicated (detection of an infectious agent), hexicon suppositories or an antiseptic - miramistin - are prescribed. It is possible to use special gynecological baths to prevent the development of infection.
In other cases, the use of antibacterial and antiseptic agents not only has no practical benefit, but can also harm the health of the reproductive organs due to changes in the normal balance of natural microflora.
Sanitation of the nasal cavity must be carried out during the cold season, especially during the period of increasing viral infections and influenza. This procedure involves constant monitoring of the condition of the nose and, if necessary, treatment of emerging pathologies. It is completely safe even for pregnant women.
Sanitation is as important for the body as daily cleansing of the face, body, and teeth. Since up to 80% of pathogenic microorganisms that are in the environment can settle on the mucous membrane. The nasopharynx is considered a conductor not only to the respiratory system, but also to the brain.
Sanitation is measures aimed at cleaning the nasal cavity from accumulated dust particles, salivary secretions, and harmful substances.
It helps reduce the concentration of pathogenic microorganisms and remove mucus clots.
In a healthy state, the nasal mucosa produces up to 500 ml of mucus secretions every day.
, which contains the necessary elements that neutralize and render harmless viruses and bacteria.
If its production is insufficient, swelling will occur and cracks will form in which pathogenic agents settle, causing respiratory diseases.
The mistake of many people is to use them, which only eliminate the symptom of nasal congestion, but do not get rid of the main cause of the disease.
What should the drugs be?
Preparations for sanitation in gynecology are selected individually for each patient. Such medicines must have the following qualities:
- a high rate of drug activity should not be stopped by the presence of pathological blood or purulent discharge;
- the product must have a pronounced effect against protozoan microorganisms;
- have a broad spectrum antiviral, antimicrobial and antifungal effect;
- act efficiently and quickly.
Main groups of antiseptics
Sanitation in gynecology is carried out using antiseptics. Such drugs are divided into three main categories:
- drugs with a narrow spectrum of therapeutic activity: antifungal medications, metronidazole and clindamycin;
- multicomponent drugs that have the disadvantage of inhibiting the growth of lactobacilli;
- drugs that have a nonspecific effect and act selectively. May provoke an allergic reaction.
What drugs are popular?
Recently, a drug such as Chlorhexidine has often been used in gynecology. This substance is used for sanitation before surgery, as well as for the treatment of inflammatory processes. The drug actively affects pathogenic microorganisms, providing antiviral, bactericidal and antimycotic effects. It does not inhibit the growth of lactobacilli. This medicine is used in a hospital setting.
Not long ago, a new drug, Hexicon, appeared on pharmacy shelves. This medicine has a wide range of actions. It is produced in the form of suppositories for intravaginal use. In addition, it is much more convenient to use than Chlorhexidine. In gynecology, suppositories for sanitation are allowed to be used at home.
Methods for performing the procedure
Among the proposed options, separate categories can be distinguished.
Medication
In this case, antiseptic medications are used. They are divided into three groups:
- narrow spectrum therapeutic direction;
- products with a multicomponent composition;
- drugs with non-specific effects.
The most universal remedy is Chlorhexidine. It is an antiviral, antifungal medicine, including the fight against specific viruses. It does not affect lactobacilli, the natural microflora is preserved.
For home sanitization purposes, Hexico vaginal suppositories are sold. They do not require medical intervention and are easy to use.
In addition, there are vaginal tablets, creams, ointments. Only a gynecologist can decide which form to choose and what it helps with.
A properly selected medicine can quickly help and have a number of necessary qualities, which are based on the following components:
- fast action;
- protection against fungi and microbes;
- antiviral effect.
Due to the components, the vaginal surface is effectively cleaned and dead cells are exfoliated. This is a kind of medical and cosmetic treatment. It is enough to do it once by a doctor, and then you can do it yourself at home.
Treatment with medical devices
For more effective cleaning, instrumental sanitation methods are offered.
Vacuum processing is a procedure carried out using an instrument method. Due to vibration, unhealthy cells are removed and the infection is washed away. Recommended for detection of chlamydia, candida, mycoplasma. After exposure to vacuum, the surface layers are cleaned, the medicine penetrates and acts faster.
Ultrasonic sanitation using small oxygen bubbles. They effectively exfoliate cells, cleanse, and revitalize. Recommended for acute colpitis, in cases of endometritis, vulvovaginitis.
Contraindications: pregnancy, cystitis, salpingitis. Prohibited for vaginal bleeding.
Types of rehabilitation
Sanitation in gynecology is carried out not only with the use of creams, tablets, suppositories and solutions. There are other methods that allow you to treat the external genitalia:
- ultrasonic sanitation;
- vacuum sanitation.
These types of procedures are safe for women’s health and painless. However, the methods have their contraindications. For example, vacuum sanitation cannot be performed before childbirth, during pregnancy, and also in case of certain diseases: salpingitis, cervicitis, allergic reactions, endometritis and cystitis. The ultrasound method is not used during vaginal bleeding.
What is vacuum sanitation
It is carried out using a special vacuum device. The unit creates vibrations and has a directional effect. When carrying out this procedure, broad-spectrum drugs are also used.
Thanks to the device, desquamated and dead cells of the mucous membranes are carefully removed, and medicinal solutions penetrate more deeply into the inner layers of tissue. This method of sanitation allows you to wash out the infection. Most often, the procedure is performed for mycoplasmosis, gardenerellosis, candidiasis, chlamydia and when the human papillomavirus is detected.