Video: Treatment of colpitis, cervicitis and erosions with natural suppositories
Basic rules for using vaginal suppositories for cervicitis:
- The combination of drugs or variety should only be selected by a doctor.
- It is advisable to put suppositories at night.
- During therapy, you should avoid sexual intercourse, or, as a last resort, use condoms.
- You should take a break during menstruation. In some cases, you can switch to rectal placement. But it is better to choose the beginning of therapy so that it can be completed before menstruation.
- Under no circumstances should suppositories be taken orally as tablets.
- When introducing suppositories, basic hygiene rules should be observed.
- You should be prepared for the fact that even during a night's sleep or in the morning, part of the suppository may come out of the vagina - it is recommended to use disposable pads.
Benefits of using candles:
- The vaginal mucosa is capable of absorbing drugs at a rate comparable to that observed when taking drugs orally.
- The introduction of suppositories avoids the unpleasant taste of tablets and the need to swallow them.
- Suppositories help create a high concentration of the active substance in the vagina, the site of inflammation.
- The load on the gastrointestinal tract and liver is minimal.
- The frequency of side effects with them is less than with tablets or capsules.
However, in some cases, using only them may not be enough , for example:
- If there is dysplasia, cicatricial deformation of the cervix.
- If sexually transmitted infections are detected.
Cervical dysplasia
Typically, suppositories for cervicitis are only part of a treatment regimen , which includes antibiotics, drugs to restore microflora, anti-inflammatory drugs, baths or douching.
Combination suppositories are usually used one at night for 5-10 days. Popular and effective ones include the following:
| Name of candles | Description |
| Terzhinan |
These are vaginal tablets. One of the advantages of Terzhinan is that it can be taken even on menstruation days.
The composition includes ternidazole (has an effect against pathogenic bacteria, as well as Trichomonas), neomycin (has an antimicrobial effect), nystatin (inhibits the proliferation of candida fungi), prednisolone (relieves signs of inflammation, itching).
Indications and contraindications
Only a doctor can prescribe the use of healing suppositories after cauterization of cervical erosion or for girls whose disease has begun to develop. Before taking the medicine, you must study the restrictions on use.
Table - Who can and cannot be treated with suppositories
Indications
Contraindications
- Initial degree of damage;
- unrealized motherhood;
- infectious process;
- irregular periods;
- inflammation of the uterus;
- mucosal injury;
- after and before cauterization of cervical erosion
- Individual intolerance to the components of the drug;
- large-scale damage to the mucosa (if the defect is more than 2 cm);
- dysplasia 3rd degree;
- high risk of malignancy.
Basic rules for treating acute and chronic cervicitis with suppositories
Suppositories are one of the effective methods for treating inflammation in the vagina. However, despite the many advantages, this dosage form cannot always completely overcome the disease - it is necessary to supplement the treatment with oral medications, for example, antibiotics.
The basic rules for using vaginal suppositories for cervicitis are as follows:
- The combination of drugs or variety should only be selected by a doctor.
- It is advisable to place suppositories at night to prevent the components from leaking out when they dissolve.
- During therapy, you should avoid sexual intercourse, or, as a last resort, use condoms. However, suppository components may increase the likelihood of suppository rupture, and protection against infection is not as reliable.
- During menstruation, you should take a break, since the effectiveness of the suppositories decreases, and some of them may simply be washed off along with the discharge. If this is allowed by the instructions, then you can switch to rectal placement, for example, for suppositories with Diclofenac, Interferons, this is possible. But it is better to choose the beginning of therapy so that it can be completed before menstruation.
- Under no circumstances should suppositories be taken orally as tablets.
- When introducing suppositories, you should follow basic hygiene rules - toilet the external genitalia, wash your hands thoroughly.
- You should be prepared for the fact that even during a night's sleep or in the morning, part of the suppository may come out of the vagina - it is recommended to use disposable pads so as not to spoil the underwear.
And here is more information about how chronic cervicitis occurs and is treated.
Traditional treatment
1. For candidiasis:
take 20 grams of juniper, sage, tansy, birch buds, 10 grams of yarrow, eucalyptus, alder cones. Brew two tablespoons of the mixture with 200 ml of boiling water, steam in a sealed container for 10 minutes, set aside from heat for half an hour, pass through a sieve and consume 70 ml in the morning, at lunch and in the evening after a meal. Duration of treatment is 4 – 12 weeks. For douching at night, add 10 ml of an alcohol preparation of eucalyptus or calendula to the prepared decoction. Do the procedure every day for 14–21 days.
2.
For viral etiology:
take 20 grams of mint, thyme, raspberry leaf, juniper cones, 10 grams of wormwood and adonis.
Brew 2 tablespoons of the collection into 400 ml of boiling water, keep covered for 60 minutes, pass through a sieve and consume orally the day before. It can be combined with oral tincture of Eleutherococcus, 40 drops twice a day ( not at night
) for a month.
3.
Take the same amount of wormwood, oak bark, bird cherry flowers, twice as much strawberry leaf and three times as much rose hips. Grind everything in a coffee grinder, take 1 liter of boiling water for 2 tablespoons of the mixture, and leave in a thermos for 8 hours. Drink 100 ml three times a day on an empty stomach. Duration of treatment is 12 – 16 weeks.
Do they always help?
Suppositories are almost always used in the treatment of cervicitis in gynecology. Their main advantages are as follows:
- The vaginal mucosa is capable of absorbing drugs at a rate comparable to that observed when taking drugs orally. This is possible thanks to the extensive network of blood vessels in this area.
- Inserting suppositories into the vagina avoids the unpleasant taste of tablets and the need to swallow them, so it does not matter what they smell or taste.
- Suppositories help create a high concentration of the active substance in the vagina, the source of inflammation.
- The load on the gastrointestinal tract and liver is minimal.
- The frequency of side effects with them is less than with tablets or capsules for oral administration.
However, in some cases, using them alone may not be enough. For example, in the following situations:
- If there is dysplasia or cicatricial deformation of the cervix, additional surgical treatment is often necessary, for example, conization.
- If sexually transmitted infections are detected, appropriate antibiotics should be added to the treatment regimen.
Treatment
1.
Elimination of the pathogen (
acyclovir, metronidazole, diflucan, terzhinan, doxycycline
),
2.
Hormonal drugs (
more often prescribed for chronic forms
).
The most commonly prescribed is Ovestin
in the form of vaginal suppositories, creams or tablets.
The drug normalizes the condition of the tissue of the cervical mucosa; it is used according to the following scheme: Ovestin 0.5 mg once a day for 21 days in a row. Next, 0.5 mg once every 3 days for 21 days, then 0.5 mg once every 7 days, 3.
Correction of vaginal microflora with the help of eubiotics and immunocorrectors (
hilak-forte and imudon
).
4.
If erosion is present, cryotherapy, laser therapy or another method of treating erosion is indicated. But this stage is started only after the inflammatory process has been completely suppressed.
Vaginal suppositories for cervicitis in women
Various suppositories can be used to treat inflammation in the cervix. According to their spectrum of action, they are divided into the following:
- antibacterial - often they contain antibiotics;
- antimicrobial - include substances that also have a detrimental effect on microbes, but have a different principle of action;
- antiviral - used if the viral nature of cervicitis is confirmed.
Based on the principle of action, we can distinguish anti-inflammatory, aimed at correcting microflora after treatment, painkillers, and healing.
There are monocomponent suppositories and combined ones. The latter include two or more active substances that have multidirectional effects and can also enhance the overall effect of use.
Watch this video about the treatment of cervicitis:
Combined
The course of treatment usually involves the use of one suppository at night for 5-10 days. Popular and effective suppositories for the treatment of cervicitis in women include the following:
| Name of candles | Description |
| Terzhinan |
These are vaginal tablets, but women often confuse them with suppositories, but their principle of action and methods of use are similar. One of the advantages of Terzhinan is that it can be taken even on menstruation days. The manufacturer assures that the effectiveness of vaginal tablets does not suffer from this.
Terzhinan contains ternidazole (has an effect against pathogenic bacteria, as well as trichomonas), neomycin (has an antimicrobial effect), nystatin (inhibits the proliferation of candida fungi), prednisolone (relieves signs of inflammation, itching).
Before inserting the vaginal tablet, it is recommended to moisten it with water. This will make it easier to do.
These are torpedo-shaped candles. Many women note that after dissolution, a significant part of the suppository still leaves the vagina even after 10 hours of sleep, so you should be prepared for vaginal discharge.
The composition of Polygynax suppositories is similar to Terzhinan - it includes neoomycin, nystatin and neomycin (has an antibacterial effect).
Preparations for the destruction of pathogenic microorganisms
- antiviral;
- antibacterial;
- antifungal.
Antiviral suppositories include Viferon, Acyclovir. The mechanism of action of the drugs is aimed at increasing a woman’s immunity, which will help destroy viruses. Most often, such suppositories for the treatment of inflammation due to herpes, HPV are prescribed in complex therapy. The course of treatment lasts up to 14 days.
Antibacterial drugs help eliminate bacteria of different groups. Before prescribing an antibiotic, a woman must be tested for sensitivity to various groups of antibiotics, so as not to waste time on treatment with drugs to which these bacteria have developed resistance. Examples of antibacterial drugs are Terzhinan, Hexicon, Metronidazole and others. The course of treatment is 7-14 days, depending on the degree of progression of the pathological process.
When the cervical canal is damaged by bacteria or viruses, changes in the flora occur, as a result of which a woman’s cervicitis is complicated by thrush and the rapid proliferation of fungi of the genus Candida. In this case, only antifungal drugs are effective. They are mainly used for thrush, which causes the development of an inflammatory process in the cervix.
Means aimed at destroying fungi include Livarol, Pimafucin, Candizol, Lomexin and others. The active ingredients in them are clotrimazole, miconazole, econazole, sertaconazole or ciclopirox. The course of treatment is 7 days (can be increased on the recommendation of a doctor).
When are rectal suppositories needed in gynecology?
In addition to the use of vaginal suppositories, rectal suppositories also help in the treatment of cervicitis, but their prescription is always determined by a doctor. It can be:
- Based on interferons . They increase nonspecific antiviral immunity, therefore they are used when the cervix is affected by HPV or HSV. In addition, they increase the effectiveness of treatment with other drugs for chlamydia, therefore they are prescribed in complex regimens.
- Anti-inflammatory. For example, suppositories with Diclofenac. They help reduce inflammation and also have an analgesic effect.
You can use rectal suppositories simultaneously with vaginal suppositories. Place them once or twice a day.
And here is more information about what suppositories are used for vaginitis.
Treatment of cervicitis should be comprehensive and competent. Almost always, various types of suppositories are included in the regimen, including those containing several components at once, which helps to increase the effectiveness of therapy. The choice must be made by the doctor based on the clinical situation and examination data.
For inflammatory diseases of the female reproductive system, including cervicitis, vaginal suppositories are widely used. This is due to their high efficiency with minimal negative effects on the body.
Immunomodulatory drugs
Immunomodulators must be used when the cervix is damaged by viral agents. This allows you to increase the local defenses of the body and suppress the replication of viruses. Suppositories with immunomodulatory effects are the main component of complex therapy for human papillomavirus infection and genital herpes in women.
The suppositories contain interferon. Its purpose is completely justified, since when viruses are integrated into the genome of a cell, they block interferon produced in the body; the introduction of this substance from the outside allows the body to quickly and easily suppress the effect of viral agents.
If a woman does not have vaginal dysbiosis, chronic infections of the genital canal and other disorders, then the viruses will not enter the cervical mucosa, since when they enter the vaginal mucosa they will be phagocytosed and the disease will not occur. If the balance of microflora is disturbed, then the likelihood of developing a viral infection increases many times.
In case of HPV and HSV, the administration of immunostimulating drugs is necessary due to the risk of cancer development, since viral agents integrate into the cell genome and provoke its active reproduction.
Important! The action of immunomodulatory drugs is aimed at regulating and correcting the process chains of the body's natural defenses, while immunostimulating suppositories activate the immune system.
In the first case, to eliminate inflammation of the cervix, immunomodulatory suppositories are suitable - Viferon, Laferobion, Genferon, Cycloferon and others. Such drugs are prescribed in long courses (several months). They contain leukocyte interferon obtained from donors.
The most famous drug with an immunostimulating effect is Polyoxidonium. The duration of the course in this case will be 10-20 days, and after a few months the course must be repeated. Suppositories for cervical inflammation with effects on the immune system can be used both vaginally and rectally.
Features and benefits of vaginal suppositories
Inflammation of the cervix is best treated with the help of vaginal suppositories. There are many medications that are available in the form of suppositories.
In addition to the main active ingredient, they contain natural fats and glycerin. Due to this, when it enters the vagina, fat melts and the main components are quickly absorbed by the mucous membrane. The active substances are also absorbed into the blood vessels. Within 30 minutes after administration, symptoms decrease.
When using other dosage forms based on the same components, the effect occurs much later and in a smaller volume. Most of the components are absorbed into the blood in the gastrointestinal tract and distributed throughout the body. Due to the method of administration, they have a local effect.
Considering the described features, we can highlight a number of advantages of using vaginal suppositories:
- local action directly at the lesion;
- effectiveness - due to absorption within 30 minutes after administration, a decrease in the manifestation of the disease is observed;
- high concentration of the main substance in the affected area;
- minimal load on the gastrointestinal tract, liver and kidneys;
- minimum of adverse reactions.
The low risk of adverse reactions and reduced impact on other organs and systems of the body make vaginal suppositories an effective drug for combating cervicitis in pregnant women. This dosage form is more suitable for patients prone to allergies, with diseases of the gastrointestinal tract, liver or kidneys, and the presence of severe chronic pathologies.
In most cases, inflammatory processes in the cervix lead to the development of a number of unpleasant symptoms: itching, swelling, pain, unpleasant odor, heavy discharge and others. To eliminate this, glucorticoids, NSAIDs, and painkillers are often used.
Of course, it is not always possible to eliminate the disease with such treatment alone. Severe forms of the disease with complications and chronic course require an integrated approach.
Important! Only a gynecologist can determine the treatment strategy for cervicitis. Before this, he carries out a series of diagnostic measures.
Options
The concept of “erosion” includes several types that differ from each other according to different criteria. To determine their features, it is necessary to consider the structure of the cervix.
The cervix is a muscular tube between the organ cavity and the vagina. It consists of two parts:
It is worth noting that the supravaginal part of the cervix is not accessible for examination. During a gynecological examination, the doctor palpates only the vaginal part. This area got its name due to the localization features.
In the speculum, the vaginal part of the cervix is defined as a pink, smooth area of the mucosa. Such external signs are caused by flat stratified epithelium.
The cervical canal is located inside the cervix, the surface of which is significantly different from the area adjacent to the vagina. The cervical canal is quite narrow, and its surface is lined with single-layer cylindrical cells, giving the mucosa a reddish color and velvety texture.
The cervical canal performs an important function. Thanks to the presence of the cervical canal, it becomes possible to reject and remove menstrual blood and promote sperm after sexual intercourse. One of the functions of the cervical canal is to protect the sterile uterine cavity from infections that can enter from the vagina. This is achieved by the activity of the glands that produce a special secretion.
Quite often, women are diagnosed with erosion in the form of ectopia, which involves the replacement of squamous multilayer epithelium with columnar single-layer cell elements. Ectopia can be either congenital or acquired.
- Congenital erosion has long been considered a pathology. The defect is detected in girls and women, which regresses on its own over time. Thanks to the introduction and use of modern research methods, scientists have established that congenital ectopia is one of the stages in the development of the reproductive tract. During the development of the female genital organs, the vaginal part of the cervix is lined with columnar epithelium. With the onset of puberty and the influence of hormones on the cervical epithelium, ectopia begins to regress. By the age of 25, the spot should completely disappear. However, estrogen deficiency is observed in various hormonal disorders. In this case, the defect disappears later and infection may occur.
- Acquired erosion is a consequence of the pathological condition of the cervix, in which a wound is initially formed. Violation of the integrity of the cervical epithelium occurs due to various traumatic factors that have a detrimental effect on the mucous membrane. This wound, called true erosion, lasts for about two weeks and then heals. The wound often shows signs of inflammation. When such an ulcer begins to heal, the recovery process is disrupted. The surface of the ulcer is covered with cells of the cervical canal, forming an ectopia. Acquired ectopia in most cases is accompanied by other diseases, in particular infectious ones. Therefore, remediation is necessary before eliminating such a defect.
The following factors lead to different types of erosion:
- hormonal fluctuations;
- infections;
- injuries of the cervical epithelium;
- weakened immunity;
- heredity.
How to choose the right drug?
The main cause of cervical lesions is infection. Pathogenic microorganisms that infect an organ lead to an acute reaction. This may be accompanied by unpleasant symptoms such as itching, burning, and pain. During the examination, the doctor may detect hyperemia, swelling, ulcerations and other changes on the surface of the uterus.
Prescription of medications occurs only after a thorough examination of the woman. An important step is to determine the infection that caused the disease. Infectious cervicitis is caused by various bacteria, viruses and fungi. Based on this, the doctor selects an active substance that fights the identified microflora.
Also, it is necessary to relieve pain and relieve swelling. NSAIDs are used for this. These can be non-steroidal anti-inflammatory drugs, medicines based on medicinal herbs and plants.
The cause of inflammation can be injuries that occur after childbirth, aggressive sex, or damage during diagnostic interventions. To restore the mucosa, regenerating medications are administered, which accelerate the healing of affected tissues.
Their use is not recommended without a doctor's prescription. It is impossible to determine the cause of the pathology without examination and consultation with a specialist. For example, the use of antibiotics will only worsen the health condition if the disease is caused by a viral infection. Only a proper medical examination, with instrumental and laboratory diagnostics, will allow one to determine an effective anti-inflammatory drug.
Erosion concept
Ectopic cervix is characterized by damage to the mucous membrane and the formation of defects in the form of ulcers. It can develop in absolutely any woman, but girls aged 25–45 years are more susceptible to the pathology.
There are many causes of ulceration. The appearance of erosion is caused by:
- early onset of sexual activity;
- penetration of pathogenic microflora - gonococci, trichomonas, chlamydia;
- organ injury;
- hormone imbalance.
Stress, overwork, and excessive physical activity also lead to the formation of a defect.
The pathology occurs latently for a long time, which leads to the development of complications. Since uterine disease is prone to transformation into cancer, it is recommended to undergo an examination at least once a year. Only through examination can changes be detected and consequences prevented.
While the ulcers have no minor manifestations. As erosion grows, the following occurs:
- painful periods;
- discomfort during intimacy;
- copious discharge.
If you notice such signs, you should consult a doctor. After clarifying the diagnosis, if the lesion is small, the doctor will prescribe suppositories for erosion
Don't hesitate to visit the hospital. Refusal to treat a disease on the cervix, ignoring the manifestations, is fraught with malignancy, malfunctions of the reproductive and reproductive systems, and infertility.
Hormonal suppositories
Female sex hormones estrogens do not stop the acute process. Often, they are indicated for hormonal imbalances, dysfunction of the ovaries and atrophy of the mucous membrane of the cervical canal. Often such conditions occur before menopause and during menopause.
The chronic course of cervicitis is often accompanied by hormonal dysfunction due to depletion of the mucosa. Hormones will help restore a woman’s hormonal levels, which will lead to restoration of the endometrium and normal functioning of the glands that produce cervical mucus. Names of suppositories that are most often prescribed by gynecologists for the hormonal nature of cervicitis:
Note! Hormonal suppositories are rarely used as monotherapy, and more often complement a complex of therapeutic measures.
Classification
Endocervicitis is a disease that has its own classification. Thanks to the existing classification, it is possible to more accurately determine the disease, which will subsequently allow the selection of adequate treatment methods.
Endocervicitis can be based on the nature of the clinical manifestations of the disease:
- acute enocervicitis, which suddenly appeared with clear clinical manifestations;
- subacute enocervicitis, with less severe symptoms, but not in remission;
- chronic endocervicitis has an unclear clinical picture with periodic stages of exacerbation.
Classification of endocervicitis according to the type of provoking agent:
- specific exocervicitis (chlamydial, gonococcal and others), the causes of which are STIs;
- nonspecific exocervicitis, the cause of which in most cases is opportunistic flora (fungi, bacteria). These are bacterial, candidal and other types of endocervicitis. Basically, the name of the pathology is consonant with the provoking agent.
Considering the activity of development of the inflammatory process of the mucous membrane of the cervix, endocervicitis is divided into:
- minimal endocervicitis, characterized by its minimal manifestations (asymptomatic);
- moderate endocervicitis, when the clinical picture is erased, but still exists, causing anxiety in women;
- pronounced endocervicitis occurs with pronounced clinical manifestations characteristic of the acute phase.
According to the distribution of the inflammatory process, endocervicitis can be:
- focal endocervicitis, an inflammatory process affecting certain areas of the mucous membrane of the cervical canal. In most cases, focal endocervicitis is characteristic of the acute stage of the disease;
- diffuse endocervicitis affects the entire mucous epithelium of the cervical canal and leads to the development of an inflammatory process in other pelvic organs;
- Atrophic endocervicitis is characteristic of age-related changes in cervical tissue, in particular thinning of the mucous epithelium of the cervical canal.
It is worth noting that with a larger area of affected tissue, the clinical picture of the disease is much brighter and more characteristic, which facilitates diagnosis. Separately, I would like to highlight acute endocervicitis, which in most cases occurs against the background of concomitant pelvic pathologies of an inflammatory nature. The acute form of the disease is the cause of many points in the classification. In the absence of treatment or when it is incorrectly selected, the acute phase passes into the subacute stage, when the manifestations subside, but the disease does not go away. And in the future, with self-medication or lack of effective treatment, chronic endocervicitis develops.
Regarding the use in the classification, moderate endocervicitis mostly refers to the chronic stage of the inflammatory process
It is worth noting that not all recommended classifications have a scar-adhesive form of endocervicitis, which occurs as a result of the completion of chronic inflammation. This is a form of endocervicitis in which there are no clinical manifestations, and the pathogen is not detected
When examined in the speculum, scar tissue will be visible on the cervix that has arisen as a result of the disease and its treatment.
This is a form of endocervicitis in which there are no clinical manifestations and the pathogen is not detected. When examined in the speculum, scar tissue will be visible on the cervix that has arisen as a result of the disease and its treatment.
Classification of the disease allows gynecologists to determine a more accurate diagnosis. A correct diagnosis is the key to a successful therapeutic effect.
Antiviral
A common cause of inflammation is an exacerbation of viral infections, such as herpes. In such situations, medications with an antiviral effect or that increase and strengthen the immune system are prescribed. They improve the local immune response thanks to the interferons they contain.
In gynecology, for viral infections, the following anti-inflammatory suppositories are most often used: Viferon and Genferon.
There is no etiotropic treatment against most types of the virus. Often, viral diseases require an integrated approach.
Diagnostics
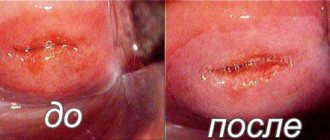
The main way to determine cervicitis is an examination by a gynecologist using speculum.
This method is simple and does not cause any discomfort. When examined, the mucous membrane is swollen and may be covered with small hemorrhages and erosions. If the cause of inflammation is an infection, specific discharge is observed. Signs of the chronic form:
In the treatment of the chronic form, along with antibiotics, an important place is occupied by physiotherapeutic methods, as well as exposure to liquid nitrogen, laser, diathermocoagulation ( cauterization
).
Antifungal
A common cause of inflammation of the genital organs in women is candidiasis. It occurs as a result of infection or overgrowth of the opportunistic candida fungus. Normally, it is acceptable in small quantities in the vagina. With a decrease in immunity, poor personal hygiene, or unprotected sex, the fungus spreads to the cervix. A sign of the disease is the appearance of cheesy discharge, itching, and pain. The use of drugs with local action will minimize the negative impact of the active substance on the body.
Antifungal suppositories are intended to relieve thrush in pregnant women, women with gastrointestinal pathologies, and liver failure. The mild course of the disease also allows you to relieve inflammation without pills.
The most commonly prescribed drugs are:
The therapeutic effect occurs quite quickly. Within a few hours after administration, the amount of fungus decreases and symptoms decrease.
Important! This group is effective only against fungal diseases. Only a gynecologist can establish a diagnosis and select the necessary treatment after examination and laboratory diagnostics.
How to treat cervicitis?
Mix in equal proportions wormwood herb, birch leaves, dandelion roots, knotweed roots, lilac flowers, fireweed leaves, celandine herb, St. John's wort herb, flaxseeds and sage herb;
The ointment is prepared in the following way: 50 g of herbal collection is crushed to a powder, pour in 0.5 liters of water, evaporate the mixture in a water bath by half, add 50 g of butter and cook for a quarter of an hour. After this, add 50 ml of glycerin or honey, mix everything and cool. Then we apply a thick layer of ointment to the strip of bandage, roll it into an oblong candle, leaving the end of the bandage free by about 6 cm. Before going to bed, such a candle must be placed in the vagina overnight.
Antimicrobial
Inflammation caused by bacteria does not stop unless the microbes are eliminated. For this purpose, suppositories with antimicrobial action are prescribed. Considering what kind of infection was determined in the patient, the doctor selects a drug that fights the detected microorganisms. It is important to complete the full course of therapy, the duration of which is determined by a specialist.
For maximum effect, they are often prescribed in combination with other antibacterial medications. The most commonly prescribed types are:
- Trichopolum is an antibacterial agent. The main component, metronidazole, is effective against many STIs;
- Hexicon is an antiseptic based on chlorhexidine. Indicated for infection with chlamydia, trichomonas, opportunistic microflora. Allowed during pregnancy;
- Betadine based on iodine. Fights opportunistic flora, chlamydia, trichomonas. Not contraindicated during pregnancy and breastfeeding.
Sea buckthorn candles
Popular effective antimicrobial agents are sea buckthorn suppositories. They consist of natural sea buckthorn oil, which is an antiseptic, anti-inflammatory and healing substance. It is used to eliminate cervicitis that occurs after childbirth. The antiseptic effect prevents infection of lesions on the mucous membrane and eliminates many types of microbes. Sea buckthorn suppositories are allowed during pregnancy and breastfeeding.
This pharmaceutical group is not effective for viral diseases. They do not have a pronounced anti-inflammatory effect. But, the elimination of pathogenic microbes leads to a significant improvement in the condition, up to complete recovery.
Use during pregnancy
There are few drugs that are allowed to be used during pregnancy. Among the harmless ones are sea buckthorn candles. If the erosion bleeds, it is possible to prescribe methyluracil suppositories. All other remedies are prohibited for pregnant women, especially during the first three months. The use of Livarol, Suporon, Terzhinan, Betadine can have a detrimental effect on the course of pregnancy and the condition of the baby.
The use of Clotrimazole, Depantol and Hexicon is possible, but only if absolutely necessary.
Bloody discharge from suppositories
The use of suppositories for ectopia should not be accompanied by such a symptom. The sign may indicate infection or the presence of a concomitant disease (endometriosis, cyst). If, during the treatment of ulcerations on the cervix, bleeding appears, the use of the drug should be discontinued. To find out the exact cause, you need to consult a doctor.
Combined suppositories
This group includes women's suppositories consisting of several active components. Depending on the composition, they are used when infected with several types of infection at the same time, such as bacteria and fungus. For such conditions, there are antifungal medications with antibacterial components. A combination of components is also often used, which, in addition to fighting infection, have anti-inflammatory and regenerative effects. Examples are the following medications:
- Polygynax – antimicrobial and antifungal action;
- Terzhinan – eliminates fungi and bacteria. Also, the composition includes prednisolone, which relieves inflammation;
- Mikozhinax – antibacterial, antimicrobial, antifungal. In addition, the composition contains dexamethasone, which eliminates itching, swelling, and inflammation;
- Klion-D – antibacterial and antimicrobial effect with analgesic effect.
Their use is possible only after laboratory testing. Self-administration or non-compliance with the gynecologist’s recommendations can aggravate the disease and lead to its transition to a chronic course.
Comparative characteristics
Viferon can be included in the complex therapy of pathologies in children, including infants and premature babies. Indications for its use:
- ARVI, including influenza (including those complicated by bacterial infection);
- pneumonia (caused by bacteria, such as chlamydia, viruses);
- inflammation of the brain (caused by bacteria, viruses);
- sepsis.
Genferon can be used in monotherapy for viral diseases without additional medications.
Viferon can be included in the complex therapy of pathologies in children, including infants and premature babies.
The basis of Genferon and Viferon is the same component - interferon alpha.
Genferon suppositories have anesthetic properties due to the content of benzocaine. Pain relief is not typical for Viferon.
Suppositories should not be used if you are hypersensitive to the components
Genferon is prescribed with caution to patients who suffer from allergies or autoimmune diseases in the acute phase
The price of the drugs is almost the same, since both are produced in the Russian Federation.
| Main active ingredient | Interferon | |
| Form | Vaginal and rectal suppositories | Ointment, gel, suppositories |
| Mode of application | Women - vaginally, men - parenterally | Into the rectum - rectally |
| Purpose | Disorders in the urogenital system | Therapy of viral infections and diseases caused by protozoa and atypical microbacteria |
| Use by children and pregnant women | Pregnant women after 12 weeks, children - from the first days of birth. | Included in the complex of therapy for infectious and inflammatory diseases in newborns and premature infants, young children and pregnant women. |
| Duration of result | 10-12 hours | |
| Safety | Does not cause harm to the body when used | |
| Manufacturer | Domestic developments | |
| Analogs | An analogue of Genferon is Viferon, Kipferon, Genferon Light. | Genferon, Interal P, Altevir, Vagiferon can replace Viferon. |
Before using any medication, it is recommended to become familiar with its characteristics.
Restoration of microflora
The vagina contains beneficial bacteria - lactobacilli. They ensure the normal functioning of organs. They maintain acid-base balance, which is important both for conceiving a child and for eliminating germs. Disturbance of the microflora occurs against the background of decreased immunity, taking medications: antibiotics, glucocoticoids, after childbirth and sanitization of the vagina and genital organs.
Lactobacilli are used to restore microflora. Acylact, Bifidumbacterin, Laktozhinal, Vaginorm and others are often prescribed.
They are often prescribed after the main antibacterial therapy for cervicitis.
Conservative therapy
The basis is anti-inflammatory oral and local agents. These are vaginal suppositories, tablets, ointments. When bacteria are detected, antibiotics are required. If tests detect HPV or herpes virus, then therapy includes antiviral agents.
The following may also be prescribed:
- Antiseptics.
- Immunomodulators.
- Vitamin and mineral complexes.
- Physiotherapy.
- Hormonal agents for the atrophic form of the disease.
When an STI is detected, it is advisable to consult a doctor not only for the woman, but also for the sexual partner. During treatment, sexual rest is recommended.
The first stage is always aimed at combating the underlying cause of cervicitis. Only then is the consequences eliminated. The chronic form requires long-term medication and an integrated approach. Subsequent tests are required to assess the effectiveness of therapy and a repeat colposcopy is required.
A course of drug therapy can only cope with the initial form of the disease. When there is no positive dynamics, the doctor recommends surgical methods.
Surgery
Modern medicine offers gentle and low-traumatic ways to get rid of the consequences of cervicitis - ectopia, condylomas, adhesions. These methods do not require long recovery or preliminary preparation.
Cryodestruction
Involves exposure to low temperatures (liquid nitrogen) on the pathological focus.
Diathermocoagulation.
Prescribed only to women who have given birth. Cauterization occurs using an electric current of the required strength. At the moment, the method is considered obsolete.
Using laser or radio waves
Advanced painless methods. Can be used by young girls planning pregnancy.
Sometimes chemical cauterization using special solutions is prescribed for young girls.
During the rehabilitation period, it is recommended to refrain from sexual contact and maintain careful intimate hygiene. It is safer to take a shower rather than a bath. It is not recommended to lift weights or perform active physical exercises. If there is discharge, use pads without fragrances or fragrances.
The optimal result when using surgical treatment methods can be obtained if antiviral and antibacterial therapy has been previously carried out. If a pathogenic pathogen remains in the body, then a relapse will not be long in coming.
Basic rules of use
The main rule of use is that it is prohibited to use them without a specialist’s prescription.
Most suppositories should not be used during menstruation. This is due to the fact that the dissolved suppository does not have time to be absorbed and excreted from the vagina with menstrual blood. This significantly reduces the effectiveness of the medication. Often, it is recommended to start administration no earlier than 3 days after the end of menstruation. But, in some cases, menstruation is not a contraindication, so you should check with your doctor about the nuances of their use.
The recommended time of administration is in the evening, after a shower before bedtime. This will ensure maximum absorption of the active components. Maintaining good personal hygiene will prevent microbial contamination during administration.
The suppository must be administered according to the instructions for use. It must be included with the medication. It is recommended to adopt a comfortable body position that will ensure maximum relaxation and correct insertion.
Once in the vagina, the suppository dissolves, part of it can be removed from the vagina, so it is recommended to use sanitary pads.
You should abstain from sexual intercourse for the entire period of therapy. Often, this is at least 10 days.
Important! If rashes, itching or any signs of allergy occur, you should stop treatment and seek medical help.
Prevention
Basic preventive measures should be aimed at identifying, sanitation and pharmacotherapy of foci of chronic infection
Particular attention is paid to the health of the urinary and reproductive systems, which are closely related anatomically and physiologically
Timely screening diagnostics and preventive medical examinations by a gynecologist guarantee the absence of STDs and other infectious infestations in the patient. Increasing the level of sex education among the population will help stop the spread of latent sexually transmitted infections around the world. Unprotected sex with gonococcal cervicitis and other forms of STDs is prohibited. However, the use of barrier methods also does not guarantee complete safety, therefore, during treatment you should refrain from sexual contact with your sexual partner.
What do you need to remember?
- Vaginal suppositories act locally, maximally affecting inflammation.
- Treatment with suppositories can only be prescribed by your attending physician.
- Which suppositories will be prescribed will depend on the cause of cervical inflammation.
Used Books
- Bykovskaya O.V. Cervicitis in patients with ureaplasma infection, clinical picture, diagnosis, treatment./ Abstract. diss. Ph.D. honey. Sci. M., 2003.
- Diseases of the cervix, vagina and vulva (clinical lectures). / Ed. V.N. Prilepskaya. M.: Medpress, 1999. - pp. 281-289.
- Non-operative gynecology. Smetnik V.P., Tumilovich L.G. 2005 Publisher: MIA.
- CDC guidelines for treatment of sexually transmitted infections. CDC 2007 Publishing house Media Sphere, Moscow.
- Treatment regimens. Obstetrics and gynecology. Edited by Kulakov V.I. and Serov V.N. 2007 Publisher: Litterra.
| Polygynax | |
| Mikozhinaks | Also multi-component suppositories contain metronidazole (sweat is active against many bacteria, as well as trichomonas), nystatin (acts on candida fungi), chloramphenicol (antimicrobial effect), dexamethasone (this is a hormonal component, relieves signs of inflammation, itching, swelling). |
| Meratin Combi | The suppositories also consist of 4 components - ornidazole (an analogue of metronidazole), nystatin, neomycin and the hormone prednisolone. |
| McMirror | These are two-component suppositories that contain an antifungal component (nystatin) and an antimicrobial component (nifuratel). There are 8 candles in a package. |
| Gynokaps | Contains miconazole and metronidazole. It has antifungal and antimicrobial effects, including against protozoa (Trichomonas). Similar in composition - Rumizol. |
| Klion-D | It contains metronidaol and miconazole. An analogue in composition is Neo-penotran. And Neo-Penotran Forte additionally contains lidocaine for an analgesic effect. |
Terzhinan and Polygynax: vaginal capsules with combined action
The drug called Terzhinan contains several active components: nystatin, neomycin sulfate, ternidazole. This wide range of antibacterial agents is distinguished by its activity against:
- Staphylococcus;
- Streptococci;
- Gram-negative organisms;
- Yeast-like candida.
The dosage is selected by the doctor individually for each patient, and only based on test results. Standard instructions prescribe the use of no more than one vaginal tablet per day.
The duration of therapy for cervicitis should not exceed 10 days.
For chronic inflammation of the cervix, Terzhinan can be used for prophylaxis (a course lasting 6 days).
Polygynax vaginal capsules consist of neomycin, polymyxin B, nystatin. Just like Terzhinan, Polygynax is effective in the fight against fungal organisms, gram-positive and gram-negative bacteria. Most often, these 2 types of vaginal capsules are prescribed as part of complex therapy for nonspecific vaginitis.
It is very easy to use Polygynax: it is enough to place one capsule deep into the vagina once a day. The duration of treatment should not exceed 12 days. During therapy, it is recommended to wear only cotton underwear and avoid using tampons and condoms. But during menstruation you should not interrupt the administration of capsules.
Causes and development factors
Inflammation of the cervix is caused by various infections in combination with disturbances in the functioning of the immune system.
Among the factors that provoke inflammation are:
- concomitant diseases of the genital area;
- age-related disorders associated with insufficient production of hormones;
- endocrine imbalance;
- traumatization of epithelial tissue by various surgical interventions;
- long-term and regular use of chemicals for contraception;
- sexual life with several sexual partners.
In order for inflammation characteristic of cervicitis to develop, several factors must be present.