Endometrial ablation
— destruction of the endometrium by controlled thermal or laser exposure. Endometrial ablation is an organ-preserving minimally invasive intervention alternative to radical hysterectomy. During the ablation process, complete destruction of the endometrium (including its basal layer, glands) and the superficial layer of the myometrium occurs, which is accompanied by the onset of secondary amenorrhea. Pregnancy after destruction of the endometrium is also impossible.
- Indications for ablation
- Contraindications to ablation
- How is uterine ablation performed?
- Prices in Moscow
Before the endometrial ablation procedure, hysteroscopy with RDV (or endometrial biopsy) is performed, on the basis of which the need for intervention is determined.
Endometrium
This is what I’m doing now with the help of ketonal suppositories. Only NVPS, I read, spoils E., so in the 1st phase it is not allowed, in the 2nd phase only if you are sure that B is absent.
Please note that in the English article there is a mention of inflamosomes, as discussed by Doctor of Medical Sciences
“At the same time, there are observations on the use of NSAIDs (as a replacement for antimicrobial and hormonal drugs) to eliminate the inflammatory process and restore the function of the atrophic endometrium in women without the pathogen [60]. "
*60.Trautmann GM, Kip KE et al. Do short-term markers of treatment efficacy predict long-term sequelae of pelvic inflammatory disease ? // Am J Obstet Gynecol 2008. P. 1-7.
So I need to do some sensitivity testing for these immunomodulators. Someone has already mentioned Lykopid positively.
Galavit, I remembered, I used kurush in the eco topic together with avelox - the e. began to grow, but in cryo during the blockade there was a span without implantation.
“Correction of immune status. It has been established [6] that when infection persists in the body, the use of interferonogenesis inducers is of particular importance. This promotes antimicrobial protection as well as
inhibits the development of clinical forms of some viral infections. Since there is evidence of a connection between inducers of interferonogenesis and the immune system [6], the use of these drugs to stimulate the immune response becomes clear. Thus, based on data from studying the immune and interferon status of patients with CE, correction of immune disorders is carried out using many drugs: galavit [13, 24], immunomax, polyoxidonium, lycopid [19, 31].
There is an opinion [19] that complex therapy, including such immunotropic drugs as lycopid and polyoxidonium, in women with nonspecific CE helps restore the sensitivity of the endometrium to hormonal regulation, reduce the subpopulations of lymphocytes in the endometrium (CD16+ and CD56+ MK-, B-cells, and lymphocytes expressing ILA-ALR+), which indicates the extinction of the topical chronic inflammatory process. "
Here’s about ZB and what the doctor of medical sciences said about the Barcelona Congress, about which Kamenetsky, the great theorist, is silent, whose ecology clinic has below-average compulsory medical insurance results:
“In conclusion, we note that for the most part, CE is a clinical and morphological concept. This is explained primarily by the fact that often the main and only clinical sign of the disease is reproductive dysfunction. It is chronic autoimmune endometritis that remains a cause of miscarriage that is 2 times more significant than progesterone deficiency, found in no more than 12% of women with early miscarriages [10; thirty].
This connection is of global importance, and at the plenary meeting of the World Congress of Obstetricians and Gynecologists (FIGO, 2006) the problem was discussed first. Later, at the congress “Contraversions in Obstetrics and Gynecology” (Barcelona, 2007), it was decided to make a diagnosis of CE if there is a history of at least one undeveloped pregnancy. "
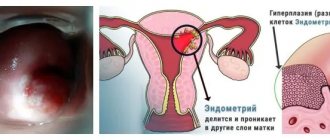
“ The group with nonspecific chronic endometritis (NCE) included patients with histological signs of NCE: the presence in endometrial samples of inflammatory infiltrates, consisting predominantly of plasma cells and lymphoid infiltrates (focal mononuclear infiltration), focal stromal fibrosis and sclerotic changes in the walls of the spiral arteries. The morphological state of the endometrium was characterized by heterogeneity. In the majority of women with NCE (n=246, 89.5%), a predominance of topical inflammation (TI) was observed, which was manifested by the severity of MNI of the endometrial stroma and the presence of functional polyps.
In the majority of women with NCE (n=246, 89.5%), a predominance of topical inflammation ( TI ) was observed, which was manifested by the severity of MNI of the endometrial stroma and the presence of functional polyps.
In the remaining patients (n=29, 10.5%), stromal fibrosis ( SFS ) predominated in the endometrium.
In 12.7% of women, NCE was combined with autoimmune thyroiditis (AIT). To exclude the influence of AIT on the state of local and systemic immunity, these patients were allocated to a separate group.
…
In women with NCE on days 19-23 of the cycle, in 46.7% of cases, a developmental delay of the endometrium was detected,
- in 20.6% - functional PE (polyp E.),
in 8.5% - GGE (presence of glandular endometrial hyperplasia)
…
In women with an ovulatory cycle without AIT, the levels of E2 and progesterone in the serum were comparable to the control group, but the expression of receptors significantly exceeded normal values.
In the group combined with AIT, the level of E2 in the blood was significantly reduced , the expression of receptors exceeded the values of the control group.
…
Features of the group of women with NCE in combination with AIT were an increase in the number of T-helper cells, the level of AEA, which was twice as high as that in the group without AIT , a decrease in the number of B-cells in the blood, as a result of their differentiation into plasma cells—producing autoantigel, which was confirmed direct correlation between the number of B cells in the endometrium and the level of AEA in the serum... "
(Note: I previously posted Ott’s research about this AEA and patented method for determining autoimmune endometritis in the blood.
In short, AIt autoimmune disease appears to be associated with autoimmune endometritis. AIT is diagnosed when AT to TP is higher than normal, and this is my disease.)
And here is the treatment plan for NCE:
“Complex therapy for NCE included physiotherapeutic methods, systemic enzyme therapy (Wobenzym 5 tablets 3 times a day, 400 tablets per course of treatment) and immunomodulators.
The following physiotherapeutic methods were used: electric pulse therapy, low-frequency magnetic field, laser radiation. Laser therapy was carried out with the LATON-100 device (semiconductor laser of low-intensity radiation with a wavelength from 760 to 820 nm). The duration of irradiation was from 3 to 5 minutes, the laser radiation power was 100 mW, the course of treatment included 8-10 procedures, therapy was carried out in combination with antioxidants.
The therapy for NCE included immunotropic drugs that have pronounced antioxidant and membrane-stabilizing effects that reduce autoimmune inflammation: drugs of microbial origin (lykopid) or a high-molecular compound (polyoxidonium). Likopid was administered orally at a dose of 1 mg 2 times a day for 10 days in two courses with a 10-day break. Polyoxidonium was used in the form of rectal suppositories of 6-12 mg every other day in 2 10-day courses with a break of 10 days. The total duration of treatment was 2 months.
A peculiarity of the treatment of women with NCE and PFS was the prescription of drugs with an immunomodulatory effect. Likopid was prescribed orally at a dose of 10 mg once a day for 10 days in two courses with a 10-day break.
In women with NCE, when combined with AIT, therapy included the administration of systemic enzyme therapy; immunostimulants included drugs that reduce immune inflammation (polyoxidonium).
Hormonal correction of ovarian failure in combination with a chronic inflammatory process was carried out with progestins, both derivatives of 17a-hydroxyprogesterone (oxyprogesterone) and 19-nortestosterone (dydrogesterone) in a cyclic mode and continued after the end of combination therapy.”
https://medical-diss....em-beremennosti
Note: dydrogesterone is duphaston
“The pathogenetic complex therapy carried out at the stage of pregnancy planning made it possible to achieve pregnancy in 30.9% of women within a year (in 65 women in the group with TV (Note: out of 246, i.e. 26%, 12 with PFS (Note. : out of 29, i.e. 41%), 8 with a combination of NCE with AIT (note: out of 35 (?), i.e. 23%), of which 68.9% had term birth (Table 5) .
Conclusions:
In the pathogenesis of nonspecific chronic endometritis, the decisive role is played by post-infectious autoimmune syndrome, manifested by a sharp increase in the blood serum levels of autoantibodies to the endometrium and cytokines...
In nonspecific chronic endometritis with a predominance of fibrous changes in the stroma in the endometrium, there is no infiltration of CD16+, CD56 + IF-, B-cells and activated HLA-B11+ lymphocytes and a change in the sensitivity of endometrial stromal receptors to hormonal effects is observed. Identified violations of systemic immunity indicators: a decrease in the number of specific cytotoxic lymphocytes CD8+, an increase in the number of T-helpers...
8. Complex therapy of nonspecific chronic endometritis, including physiotherapeutic methods, systemic enzyme therapy, immunomodulatory agents (lycopid, polyoxidonium) and progesterone, leads to the restoration of endometrial sensitivity to hormonal regulation, suppression of the inflammatory process...
PRACTICAL RECOMMENDATIONS
5. In the presence of nonspecific chronic endometritis with topical signs of inflammation (prevalence in the endometrium of CD 16+, CD56+ NK-, B-cells and lymphocytes expressing HLA DR+), as well as in combination with glandular endometrial polyps, it is necessary to carry out repeated bacteriological and virological examinations in order to identify a possible pathogen and prescribe etiotropic antibacterial therapy.
6. When nonspecific chronic endometritis is combined with glandular endometrial polyps after curettage of the uterine cavity, the administration of gestagens, systemic enzyme therapy drugs (Wobenzym) and immunomodulators (lycopid, polyoxidonium) is indicated.
8. Treatment of nonspecific chronic endometritis with a predominance of stromal fibrosis should be comprehensive and include immunotropic drugs (Licopid 10 mg), proteolytic enzymes, angio-oxidants, and physiotherapeutic methods of treatment.
«
Modified on October 12, 2021 by Toffeeskiska
Endometrial ablation - where to do it?
Ablation of the endometrium refers to minimally invasive gynecological interventions in which the mucous layer of the uterus, the endometrium, is removed. It refers to methods of treating uterine bleeding associated with benign diseases. This procedure is not recommended for the treatment of uterine bleeding in patients who are planning a future pregnancy. To carry out endometrial ablation today, laser radiation, high-frequency radio waves, cryoablation - “freezing”, and thermoablation - thermal exposure are used. The choice of ablation method depends on various factors. Some patients may experience endometrial regrowth after endometrial ablation and may require repeat surgery.
Indications for endometrial ablation
This minimally invasive treatment method is indicated for the treatment of gynecological conditions associated with uterine bleeding that are not caused by a malignant tumor. In such cases, more radical interventions are required. An important feature of endometrial ablation is that it should be used in patients who do not plan a future pregnancy, since after it there is no endometrial tissue into which the embryo is implanted. Also, endometrial ablation is not used in patients with an active infectious-inflammatory process. This treatment method is not considered first-line therapy for severe uterine bleeding and is indicated only if conservative drug and hormonal treatment is ineffective.
Endometrial ablation is indicated for the treatment of uterine bleeding in postmenopausal or perimenopausal women with a normal endometrial cavity. It is also used to treat postmenopausal bleeding of benign origin.
Potential candidates for endometrial ablation include patients with anovulatory bleeding and bleeding associated with uterine fibroids, but it is important to understand that ablation itself does not affect ovulatory function of the ovaries and does not remove the fibroids themselves. Therefore, such patients are at high risk of unsatisfactory treatment results.
How is endometrial ablation performed?
Before performing any minimally invasive procedure, incl. in gynecology, a complex of studies is carried out, including laboratory tests and instrumental diagnostic methods. It is important to perform an endometrial biopsy before endometrial ablation to rule out cancer. For this purpose, hysteroscopy with endometrial biopsy can be performed. It also allows us to identify some causes of uterine bleeding (polyps, fibroids, endometrial hyperplasia, cancer). This method allows you to assess the need for endometrial ablation; for example, with endometrial fibroids or polyps, there is no need for ablation of the entire endometrium. Before endometrial ablation, it is important to rule out pregnancy and remove the IUD.
A week before endometrial ablation, hormonal therapy is recommended, especially in young patients, in order to reduce endometrial tissue, which significantly affects the success of the procedure. The thinner the endometrium, the higher the efficiency of ablation.
The procedure is performed on a gynecological chair. First, the cervical cavity is expanded with special bougies. After this, the ablation procedure itself is carried out. To do this, a special electrode is inserted into the uterine cavity, which opens like a mesh umbrella and is pressed against the entire surface of the endometrium, after which high-frequency radio waves are applied through it, due to which ablation of endometrial tissue occurs. The process of such exposure itself lasts about 1.5 minutes.
The endometrial ablation procedure is performed under anesthesia. The choice of anesthesia depends on the patient's condition and other factors. Usually, intravenous anesthesia is sufficient, from which the patient can quickly recover, which allows endometrial ablation to be performed on an outpatient basis, without the need for the patient to be hospitalized in a clinic.
Currently, other methods of endometrial ablation have been developed using cryosurgery , laser radiation, and thermal effect. The endometrial ablation procedure is considered a fairly effective and safe method for treating uterine bleeding and is successfully used in foreign clinics. Patients from Russia have rightfully chosen today the best and most famous clinics in Austria, Italy, Germany, Switzerland, Israel, America, India, Turkey and South Korea. This is due to the high experience and qualifications of foreign specialists, much better equipment compared to domestic clinics, comfortable conditions in the wards, as well as the high efficiency of treatment abroad.