Indications for suturing the cervix during pregnancy
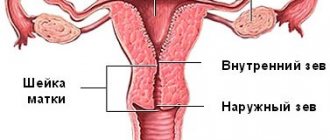
Diagnosis of ICI involves the following obstetric examinations:
- gynecological examination of the pregnant woman’s cervix using vaginal examination using a speculum;
- Ultrasound examination to determine the length of the neck;
- conducting a test to determine the degree of likelihood of premature birth in the patient.
Based on the data obtained, the gynecologist will determine a program for correcting the identified pathology in order to preserve the health of the unborn child and prevent the risk of premature birth.
Suturing the cervix is considered a surgical method for treating ICI. Such an intervention requires mandatory preparation of the female body for the operation. Swabs from the genital tract are taken from the expectant mother and the blood is examined. The decision to apply sutures is usually made in critical situations. The reasons for surgical treatment may be the following:
- significant softening of the cervix, detected by vaginal examination;
- shortening of the cervix up to 3 cm;
- pregnancy period up to 20 weeks;
- opening of the cervical canal up to 9 mm.
Timely identification of alarming symptoms will allow you to make a decision about suturing the cervix to save the pregnancy.
What are the differences between different types of cerclage?
In gynecological practice, many options for cerclage have been developed. Access to the cervix can be:
- vaginal – the manipulation is carried out in the standard Trendelenburg position on a chair, local anesthesia or spinal anesthesia is used;
- abdominal cerclage - access to the cervix is carried out through the anterior abdominal wall; initially, a laparotomy incision was made for this, but after the development of laparoscopy, several punctures in the abdominal wall are sufficient for suturing.
Vaginal cerclage is performed in one of three ways recommended by the clinical protocols of the Ministry of Health:
- Macdonald cervical cerclage without tissue dissection.
- Double U-shaped intramucosal suture in the area of the internal os according to Lyubimova’s method modified by Mamedalieva.
- High cervical suture using the Shirodkar method.
When performing MacDonald cerclage, the suture is placed as close as possible to the junction of the cervix with the vaginal vault. No tissue dissection is performed in this case.
A U-shaped suture is placed in the place where the mucous membrane of the anterior vaginal vault passes into the exocervix. Synthetic threads are used for work. The puncture is made 0.5 cm to the right side of the midline through the entire thickness of the neck, with the needle exiting on its back side. Then they puncture through the posterior vaginal fornix to the left of the midline, the puncture passes through the front of the cervix. The second stitch is applied symmetrically. Each seam is tightened with a separate knot.
The Shirodkar method is used less frequently due to the high risk of complications and trauma. The bladder and rectum are first separated from the vaginal tissue. The advantage of this technique is that the seam can be placed as close as possible to the internal pharynx. The threads are gradually tightened in front and behind to tighten the neck and incisions in the mucous membrane.
According to studies, none of the methods has any visible advantages in preventing premature birth, but Shirodkar’s method is often accompanied by the following complications:
- bleeding;
- bladder injury;
- hematomas;
- infection.
A transabdominal suture is applied with silk or monofilament thread. Cerclage of the cervix with mersilene tape has become widespread; currently this material is more preferable, but the choice always remains with the operating doctor. The manipulation is carried out no later than 25 weeks. Also, the woman should not have signs of infection, and according to the results of screening in the 1st trimester, the child is healthy and without genetic abnormalities.
For laparoscopic cerclage, several incisions 2.5-3 cm long are made on the anterior abdominal wall, through which video equipment and manipulators are introduced into the pelvic cavity. The operation is almost bloodless. Mersilene tape or threads are sewn as close as possible to the internal pharynx and provide reliable fixation. The suture tension is adjusted so that a No. 5 Hegar dilator passes through the cervical canal.
Indications for installing a pessary on the cervix during pregnancy
A pessary is a specially made ring made of high-quality flexible silicone or plastic, which is installed on the cervix to redistribute pressure on the organ. This measure prevents premature dilatation and eliminates the threat of miscarriage. Installation of an obstetric ring is effective in the early stages of identified pathology, when the cervix has not yet fully opened.
The advantages of this method are obvious:
- lack of surgical intervention;
- painlessness;
- speed of the procedure.
Installation of a pessary for ICI is recommended in a number of the following cases:
- weakening of the uterine walls;
- signs of cervical shortening;
- opening of the uterine pharynx;
- multiple pregnancy;
- the presence of stitches on the cervix;
- signs of the inflammatory process;
- urinary incontinence;
- bladder hernia.
The need to install a ring arises in cases where a pregnant woman has had a difficult birth in the past. Possible reasons may be pathology of the development of the genital organs and frequent abortions in the past.
Contraindications for installing a pessary on the cervix during pregnancy
The procedure for installing an obstetric pessary is contraindicated in a number of cases:
- presence of discharge with signs of blood;
- protrusion of the membranes;
- somatic pathologies in severe form;
- chronic inflammatory processes;
- signs of frozen pregnancy;
- functional disruptions in the functioning of the bladder.
A pessary is not installed in women at the last stage of ICI, since its use in this case is ineffective.
Reviews of women using a pessary for the cervix during pregnancy
And what do the women themselves say who used the ring as a way to maintain a pregnancy? Below are patient reviews:
- Anastasia, 25 years old: “My second pregnancy was not entirely easy. The gynecologist diagnosed ICI, which scared me terribly. After the examination, they installed a ring from a German manufacturer. As a result, she not only reached the deadline, but also passed. Girls, don't be afraid of the pessary. There was no pain or discomfort, and the baby was born full-term and absolutely healthy.”
- Veronica, 36 years old: “At 20 weeks, the doctor said that I had problems: the cervix was shortening ahead of schedule. They put a ring on it. Everything went away in literally five minutes and was not accompanied by pain. The result is a preserved pregnancy and a healthy baby.”
- Oksana, 30 years old: “I was threatened with termination of pregnancy at 22 weeks of pregnancy. They offered to put a ring on me, which really scared me. But if this is necessary for a child, you don’t have to choose. I reached 38 weeks with him and gave birth successfully. Now I’m pregnant with my second child.”
Possible complications
The most common complications of surgical treatment of ICI are:
- cutting of sutures (with increased tone of the uterus, incorrect performance of the operation or with severe inflammation of the cervix);
- addition of a bacterial infection;
- ruptures and fistulas of the cervix;
- amniotic sac injury (occurs during surgery);
- endotoxic shock;
- sepsis;
- difficulties in childbirth.
However, in most cases, if all the rules of the operation and the postoperative period are followed, pregnancy ends with the birth of a healthy baby at the right time.
But most importantly, remember that if you have received stitches, this does not completely exclude ICI during pregnancy and does not remove the threat of premature birth. Therefore, you need to be extremely attentive to your feelings, and if unusual symptoms appear (pain in the lower abdomen, in the perineum, discharge, fever), you should immediately contact your doctor to exclude the development of complications.
I was observed by a gynecologist-endocrinologist for many years. She independently studied and tested homeopathy, herbal medicine and other non-traditional methods of therapy. Mother of natural twins, who went through a difficult pregnancy and difficult postpartum period.
Reviews of women who preferred stitches on the cervix during pregnancy
- Elena, 45 years old: “The third pregnancy was simply terrible for me. From the very beginning everything went wrong and the fear of not carrying the child to term was constantly accompanying me. Threat of miscarriage, premature birth, and so on... They put stitches on my cervix, which was not the most pleasant procedure. Constant stay in the hospital, sexual rest and as a result I gave birth to a boy weighing 2.5 kg at 37 weeks. Now he is already 15. Everything ended well.”
- Polina, 27 years old: “They sewed it up at 25 weeks. Complete rest and sick leave until the end of pregnancy. A week before giving birth, the stitches were removed and I gave birth at 38 weeks. I suffered, of course, but the preserved pregnancy is worth it.”
- Anna, 39 years old: “I had a stitch at 32 weeks. I didn’t work, but I didn’t lie on the couch either: I walked, did household chores. Periodically I suffered from pain in the cervical area. Thank God it was all over soon and my baby was born. Thank you doctor.”
How is the recovery period going?
To reduce the risk of complications after surgery, a woman should stay in the hospital for 5–7 days, she is prescribed antibiotics, antispasmodics, and the vagina is treated with antiseptic solutions. For several days, a pregnant woman may be bothered by pain in the lower abdomen and the discharge of ichor - such phenomena are not considered pathological and most often go away on their own.
On the first day after surgery, strict bed rest is indicated; in the future, the woman will have to pay increased attention to nutrition and daily routine in order to avoid complications. The stitches are removed at 37 weeks.
What you can and cannot do after suturing:
- Do not lift heavy objects;
- Doctors recommend abstaining from sexual intercourse until childbirth;
- proper nutrition should be aimed at preventing constipation - the diet should contain more vegetables and fruits, the amount of sweet, fatty foods, and baked goods should be limited;
- Eating dried fruits regularly will help normalize stools and saturate the body with all the necessary microelements.
After surgery, a woman needs to promptly treat all emerging diseases, avoid stress, and follow hygiene rules.
Suturing the uterine cervix is a safe and effective way to preserve pregnancy in case of premature opening of the pharynx. Most women tolerate the operation well, complications rarely occur, you just need to strictly follow all the doctor’s instructions.
Doctors' opinion about installing a pessary for the cervix during pregnancy
Doctors have an ambiguous attitude towards installing a pessary. Russian gynecologists consider the installation of an obstetric ring to be the optimal way to prevent premature birth in a patient. Timely measures taken and correct installation of the pessary have saved more than one pregnancy from early resolution. The ring is removed at 37 weeks, when the baby is ready to meet his mother. But this is not a direct indication for childbirth - a woman can stay at home until her water breaks. According to doctors, a pessary is the optimal method to preserve pregnancy in a number of cases and there are no contraindications for installation.
But not all doctors think so. Here is the opinion of Elena Berezovskaya, a practicing obstetrician-gynecologist who lives and works in Canada:
“Pessaries are practically not used abroad, because their ineffectiveness has been proven. In addition, this is a foreign body that is constantly in the vagina and irritates the cervix, which is not desirable for ICI. Most often, only our post-Soviet doctors choose, because suturing requires skills and conditions. And handing a woman a pessary and assuring her that this is what will help her is as easy as shelling pears. Abroad, the choice is only in the technique of suturing, but usually the doctor knows only one type of such technique.”
Predictions and consequences
The pregnancy rate after cerclage is quite high - more than 80%. Prognosis depends on the degree of cervical insufficiency and the reasons why the woman was indicated for surgery. If after the operation she follows all the doctor’s recommendations, then the chances of carrying the child to 36-37 weeks increase significantly.
Types of pessaries for the cervix during pregnancy
To maintain pregnancy, obstetric pessaries are used, of which there are 3 types:
- Domed. The device is shaped like a bowl and has small holes around the perimeter. Their function is to drain vaginal secretions. Doctors use this pessary for premature shortening of the cervix.
- Annular. Made in the shape of a ring with 4 dents on different sides. This allows the cervix to be compressed. Recommended for dilation of the uterine pharynx in a pregnant woman.
- Unloading. Its main purpose is to redistribute and reduce the load on the lower part of the uterus. The ring creates reliable support for the reproductive organ and prevents its displacement.
Important! The obstetric pessary is made from materials that do not cause allergic reactions.
Examinations before using a pessary on the cervix during pregnancy
During pregnancy, women have an increased risk of developing cervical pathologies under the influence of hormones.
If women have previously had gynecological diseases or are predisposed to them, it is necessary to undergo examinations to prevent serious complications at an early stage. The examination includes not only cytology and tests, but also colposcopy of the cervix.
Many pregnant women are hearing about such an examination for the first time, and as a result, they have questions about the safety of the procedure.
What is colposcopy and how is it done during pregnancy?
Colposcopy is an examination of the cervix using a special illuminated colposcope, which allows you to identify a large number of diseases at an early stage. This procedure does not lead to soft tissue injury.
Colposcopy allows you to examine in detail not only the cervix, but also the vaginal walls, as well as collect smear fluid and biomaterial for histology or cytology.
Today, this procedure is the most accurate and accessible in gynecology.
Colposcopy is performed on a gynecological chair using a special device. The device can be either a regular optical one or a special one – connected to a monitor to display the image on the screen. If there are any suspicions, the doctor conducts an extensive examination, applying special solutions - Lugol or acetic acid - to the affected cervical tissue.
Colposcopy is a painless procedure that does not require the use of painkillers and does not cause discomfort to the woman.
Is it possible to do colposcopy during early pregnancy?
Ideally, colposcopy should be done at the planning stage of pregnancy. This will help the specialist obtain the necessary information to determine the woman’s health status and make a prognosis regarding future pregnancy. Unfortunately, only a few people think about this.
When registering for pregnancy, the gynecologist at the first examination refers women to colposcopy. There is no point in doubting or refusing such an inspection. This procedure will not harm you, but, on the contrary, will at least allow you to identify ordinary erosion, which can develop into severe dysplasia. If the pathology is not diagnosed in time, there is a chance of rapid development of cancer in a pregnant woman.
But it is worth noting the fact that colposcopy in the early stages of pregnancy is prescribed only in cases where the pregnancy proceeds without complications. If there is a threat of miscarriage or the period of conception is no more than two weeks, such an examination is carried out in extreme cases.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice. Always trust your doctor first!