07.05.2018, 13:37
Good afternoon.
Woman, 32 years old, weight 62 kg, height 168 cm. Menstruation since 12 years, regular (28 days), normal in volume, painful. There were no gynecological diseases.
Infertility for 5 years (male factor) Previous topics
[Only registered and activated users can see links] [Only registered and activated users can see links]
1 IVF pregnancy in 2021, froze at 6-8 weeks. The fetal karyotype is trisomy 21. Vacuum aspiration. 2 hysteroscopies were performed.
Last menstruation - 12/08/2017, currently 2 IVF-induced pregnancy 21-22 weeks.
At 20 weeks, cervicometry revealed a V-shaped expansion of the internal os up to 8 mm, and the length of the undilated portion of the cervical canal was 27 mm. The length of the cervix is 31 mm. Three days later (exactly at 21 weeks), a suture was placed on the cervix, no antibiotics were used, and she was discharged from the hospital on the third day after the operation with a free regimen.
Currently prescribed: duphaston, noshpa, magnesium, papaverine at night. A visit to the doctor is scheduled after May 14.
After discharge (in the evening of the 3rd and in the morning of the 4th day after surgery), several times there was a mucous brown discharge in the form of clots of mucus, after which there was a brown “spotting” discharge with small flakes. Today is the 5th day after the operation, the discharge is lighter, but still light brown, it has become more abundant, and the consistency resembles normal. Otherwise I feel good.
Questions: 1. Is this normal discharge or should I go to the doctor earlier (difficult, since the doctor I trust is on vacation, that’s why this is the date)? 2. how long should you drink duphaston? Does it make sense to switch to utrozhestan? 3. Are suppositories or antibiotics needed for prevention? 4. Do I understand correctly that there is no need for bed rest if nothing bothers you?
07.05.2018, 16:25
Hello.
3. No, if there is no colpitis. 4. Yes, that's right.
07.05.2018, 16:47
Hello. 1. May be normal. Were the stitches examined upon discharge? 2. Duphaston is not needed, the need for morning is doubtful. 3. No, if there is no colpitis. 4. Yes, that's right.
Thanks for such a quick response!
1. Upon discharge, she was examined, but not in mirrors, but manually. They said that everything was fine, my cervix was going back, there would be discharge for a few more days, but I didn’t think to ask about consistency, etc. 2. Duphaston was prescribed before the appointment, if the doctor cancels it in person, then after 22 weeks? 3. That is, if the “flakes” and brown color finally disappear, there will be no strange color and itching, and you won’t have to worry about the discharge?
07.05.2018, 19:17
No progesterone needed
12.05.2018, 17:37
No progesterone needed
Please tell me how often you need to visually inspect the stitches, go for an ultrasound, and whether you need to take smears (and if so, which ones?)
And could frequent, painless urination be associated with stitches?
13.05.2018, 18:27
27.05.2018, 17:58
One visual inspection is enough, 1-2 days after the suture is applied. Ultrasound, smears during screening periods or when complaints arise. Painful urination is not associated with stitches, do a urine test.
Urine tests showed no abnormalities; bacteria did not grow in the culture.
Now for a week I have been bothered by a pulling sensation between the navel and the line where pubic hair begins to grow. It's not pain, but it feels like muscle tension. The feeling can last for a long time, up to half a day. Intensifies with gases, pressure bands, movements (sometimes provoked by movements), a little easier in the knee-elbow position.
The doctor at the hospital said that the abdomen is soft at this time, she does not see any tone.
Should I insist on treatment or are these normal “pregnant” sensations?
28.05.2018, 10:31
May be the norm
12.06.2018, 13:07
May be the norm
Unfortunately, gestational diabetes mellitus was diagnosed. I interact with an endocrinologist (the diet does not reduce fasting sugar, Lantus was prescribed). But while on a diet and taking iron (Sideral Forte), difficulties with bowel movements began.
There was no long-term constipation, but once every two days there was voluminous, hard feces, after going to the toilet the whole day there was a pulling in the vagina, as if there were stitches.
I will continue to struggle with constipation, the questions are: are these really stitches? Do I need to go to the doctor to look at the stitches if the pulling sensation has passed and the nature of the discharge has not changed?
And one more additional question, now I’m 26 weeks, at 28 I’m planning an immunoglobulin injection, since I have 4-, the father of the child has 2+. I will buy the medicine myself, which one is better to choose?
12.06.2018, 15:04
12.06.2018, 15:38
If you have any complaints, check with a full-time doctor. Hyperrow, camrow, immunocedrion.
At the moment there are no complaints, so it’s not clear whether to go to an in-person appointment or not.
17.06.2018, 13:48
If you have any complaints, check with a full-time doctor. Hyperrow, camrow, immunocedrion.
Please help me with the regulatory documents of the Russian Ministry of Health. The situation is as follows: GTT results (with 75 g of glucose): fasting sugar 5.12 after an hour 10.65 after two hours 6.9
I went to see an endocrinologist at a paid clinic, take sugar measurements, and follow a diet. Unfortunately, on a diet, sugar after meals is still up to 7, but on an empty stomach it is above 5.1. I give Lantus injections at night (currently 8 units, but try 5.3 units in the morning).
However, the antenatal clinic sent me through compulsory medical insurance to a republican hospital, since with GDM it is necessary to plan birth in a specialized institution.
There, the head of endocrinology says that the results of my test are not diabetes, the readings are low, after an hour there was no need to look at all. He ordered me to donate glycated hemoglobin (for a fee) and blood without first injecting insulin on an empty stomach and then make a decision on the diagnosis. When I said that gestational and simple diabetes are different, he said no, they are the same thing.
What regulatory documents can be used in a new conversation with the manager, where the procedure for establishing the diagnosis of “gestational diabetes mellitus” is approved?
10.07.2018, 21:00
If you have any complaints, check with a full-time doctor. Hyperrow, camrow, immunocedrion.
Good afternoon.
At 28 weeks, hyperrow was introduced. I am currently 30 weeks 4 days. According to the results of the 3rd ultrasound: lag of coolant and expansion of the internal pharynx, health is normal, blood pressure is low (95/60), no edema, GDM is compensated (glargine), periodically pulls (painlessly) in the lower abdomen and on the right in the groin area. Is hospital treatment required? I have attached a photo of the ultrasound.
10.07.2018, 22:18
18.07.2018, 10:02
The width of the internal opening is permissible. Monitoring fetal growth after 10-14 days.
We were admitted to the hospital for a week, CTG was done every day, and on discharge: there were no signs of fetal hypoxia.
According to ultrasound, a week from the previous one (1450 g), the weight is 1740. Is this normal growth?
18.07.2018, 14:38
Normal
30.07.2018, 15:46
Normal
Hello. Now I am 33 weeks 3 days, with active movements the pain shoots into the bladder and into the perineum from different sides, and it radiates strongly to the clitoris. It is especially noticeable when walking. It goes by quickly.
Is this somehow connected with the cervix (I have had a circular suture since 21 weeks), should I go for cervicometry or urgently see a doctor?
Good afternoon
At week 17, the cervix was sutured (there was a miscarriage in the past at this time, dynamic shortening of the cervix and opening of the internal os). I re-read everything on the site about ICN and suturing and tocalytic therapy, and I still have a number of questions regarding which (due to great worries) I would really like to receive an additional answer. (The brains give in to panic in anxiety)
Do I understand correctly that after stitching:
1) there is no particular point in lying down, because according to research this does not affect the situation (except for multiple births)
2) there is no point in using any tocalytics, because there are no effective ones anyway (or are there some that are still justified? Do I need to take any special pills after stitching?
3) is it necessary to inject and drink antibiotics immediately after stitching? How many days? (It’s not healthy for a child, so it worries me a lot, I’ve been injected for 5 days now)
4) do the seams need to be rehabilitated? If yes, how often? Only immediately after application for a couple of days or then too?
5) is it true that the tone of the uterus during sutures is not dangerous, because whether it was tone at all was unknown (it is often misdiagnosed on ultrasound) and it is not a constant phenomenon. In addition, in fear, fighting tone is useless, since this is what it appears from. It's right? If not, then what about the tone at the sutures? How should we approach this issue? Is he dangerous at all?
6) Do I understand correctly that after suturing, smears and chair examinations and ultrasound are recommended every 2 weeks? What is actually checked during these procedures? The strokes are still somewhat clear, but the rest is not so clear. On smears they look primarily at leukocytes, right?
7) And in light of the question above. What dynamics of the neck length and opening of the internal pharynx should be after suturing (ultrasound)? Should everything lengthen and close? How fast? What if it shortens and opens further? Or is this an unimportant factor? Why then regular ultrasounds?
I beg your pardon for the number of questions, but I know the official answers of traditional gynecologists to them (even many options), but I don’t really trust them, because no one can really explain anything and they prescribe “because”. At the same time, sometimes even I can understand that the logic in the answers is broken and the person most likely does not understand what he is talking about. I got myself into trouble with this.
I really trust your site! I'll be looking forward to your answer!
THANKS IN ADVANCE!!!
Pregnancy is an important and responsible period in the life of every woman. Unfortunately, health problems are not uncommon at this time. And in some cases, the doctor recommends a special procedure to the patient, during which a suture is placed. Sutures are needed on the cervix during pregnancy to prevent miscarriage or premature birth.
On the other hand, surgery during pregnancy frightens women. So in what cases is such a procedure prescribed? What risks does it involve? What is the surgical procedure and how is the rehabilitation period? The answers to these questions are of interest to many patients.
What to pay attention to after suturing the cervix? What management is recommended?
At week 17, the cervix was sutured (there was a miscarriage in the past at this time, dynamic shortening of the cervix and opening of the internal os). I re-read everything on the site about ICN and suturing and tocalytic therapy, and I still have a number of questions regarding which (due to great worries) I would really like to receive an additional answer. (The brains give in to panic in anxiety)
Do I understand correctly that after stitching:
1) there is no particular point in lying down, because according to research this does not affect the situation (except for multiple births)
2) there is no point in using any tocalytics, because there are no effective ones anyway (or are there some that are still justified? Do I need to take any special pills after stitching?
Do you always follow doctors' orders?
Yes, they know us better.
43.38%
Not always, because more information can be obtained from other women in labor.
20.31%
I comply, but I check reviews and advice from various mothers.
36.31%
Voted: 325
3) is it necessary to inject and drink antibiotics immediately after stitching? How many days? (It’s not healthy for a child, so it worries me a lot, I’ve been injected for 5 days now)
4) do the seams need to be rehabilitated? If yes, how often? Only immediately after application for a couple of days or then too?
5) is it true that the tone of the uterus during sutures is not dangerous, because whether it was tone at all was unknown (it is often misdiagnosed on ultrasound) and it is not a constant phenomenon. In addition, in fear, fighting tone is useless, since this is what it appears from. It's right? If not, then what about the tone at the sutures? How should we approach this issue? Is he dangerous at all?
6) Do I understand correctly that after suturing, smears and chair examinations and ultrasound are recommended every 2 weeks? What is actually checked during these procedures? The strokes are still somewhat clear, but the rest is not so clear. On smears they look primarily at leukocytes, right?
7) And in light of the question above. What dynamics of the neck length and opening of the internal pharynx should be after suturing (ultrasound)? Should everything lengthen and close? How fast? What if it shortens and opens further? Or is this an unimportant factor? Why then regular ultrasounds?
I beg your pardon for the number of questions, but I know the official answers of traditional gynecologists to them (even many options), but I don’t really trust them, because no one can really explain anything and they prescribe “because”. At the same time, sometimes even I can understand that the logic in the answers is broken and the person most likely does not understand what he is talking about. I got myself into trouble with this.
I really trust your site! I'll be looking forward to your answer!
Elena Berezovskaya Doctor
1) correct. The woman is observed in the hospital for only a few days. If there are no complications, they are sent home.
2) After suturing, only short-term tocolytics are used, only once, i.e. immediately after surgery. This is either indomethacin or nitroglycerin, but if the period is too short, then nothing. Practically nothing else is used. Tocolytic therapy has its own strict indications, including strict pregnancy periods for use.
3) No one prescribes antibiotics abroad. Some doctors recommend the use of a short course of antibiotics only when applying an emergency suture to the cervix (later), because there is a high risk of chorioamnionitis. The approach is always individual.
4) How are you going to sanitize the seams? Of course not needed. And the less you pull the cervix, the better. Absolutely none of your concern, so to speak. They did the job and that’s all – just observation.
5) Tone is not dangerous, because the uterus is a muscular organ and constantly reacts to everything with contractions. But manipulations on the cervix can provoke strong contractions of the uterus like contractions and lead to termination of pregnancy.
6) Incorrect. This is an unreasonable overreach. I repeat once again: the less they go to the cervix with a suture, the better. Control ultrasound and its quantity depends on the condition of the cervix, i.e. its length. No additional smears are taken if there are no complaints about pathological discharge. Such a pregnancy is equated to a normal one, except that the woman continues to be at risk for premature birth.
7) The length of the cervix may not change, i.e. it can remain short. The internal pharynx may also remain in the same state. The point is that if there is no progress for the worse, i.e. the cervix does not shorten even more, there is no pain or discharge, the fetus is developing normally, this indicates the effectiveness of the operation. So, returning the cervix to normal length is not always necessary. An ultrasound, but usually no more than once a month, is performed to see if the cervix is contracting further and if there are other complications after the suture.
7) And in light of the question above. What dynamics of the neck length and opening of the internal pharynx should be after suturing (ultrasound)? Should everything lengthen and close? How fast? What if it shortens and opens further? Or is this an unimportant factor? Why then regular ultrasounds?
What if childbirth?
Regardless of whether you have a pessary or a suture, you need to see a doctor periodically. Moreover, the closer to the PDR, the more often. The gynecologist, based on the current condition of the cervix, will set a date for you to remove the “lock” from the uterus.
Of course, at the first suspicion of contractions, you need to run to the doctor. Otherwise, the consequences can be disastrous: up to cervical rupture. At the same time, you shouldn’t worry about every lost minute, especially if it’s your first birth.
There is a belief among women in labor: if, after removing a suture or pessary, labor occurs within a period of a couple of hours to three days, it means that it was really necessary to carry out the procedure of “closing” the cervix. If later, it means that the suture or pessary was a reinsurance measure. However, if you give birth a week after removal, do not rush to blame your gynecologist. Perhaps your cervix itself has undergone changes.
Asked by: Victoria
Female gender
Age: 37
Chronic diseases: not specified
Hello, I am worried about bloody, pink discharge 8 days after getting stitches on the cervix at 19 weeks. Since the previous pregnancy ended with the dilatation of the cervix and the rupture of water at 18 weeks, in this pregnancy I have been monitoring the cervix since 12 weeks. She was hospitalized as planned at 18 weeks; upon admission, the cervix was closed, 3.7 cm (in 2013 there was conization of the cervix), rather soft. Examination on the chair the day after the operation - the condition is satisfactory, vaginal ultrasound 7 days later - the cervix is closed, 3.4. During the operation, the doctor noted that the neck was plump, but short. Recommendations upon discharge: ginipral 0.5 every 6 hours with verapamil, utrozhestan to drink 3 times 200 times, sanitation with miramistin once every 2 weeks. Tell me, how long can the pink discharge last? Thank you!
Can the combination of Isoprinosine, Superlymph and Uro-Vaxom cause bleeding? Bleeds for 2 days. I have been suffering from heavy vaginal discharge for 2 years. They are white, transparent, dark brown all the time, regardless of the day of the cycle. The gynecologist tried everything she could, nothing helped, there wasn’t even a slight remission. She diagnosed cervical erosion (0.5 mm) 4 years ago. The tests were always consistently bad, with leukocytes and inflammation. The last time the smear for flora was good, but the cytogram showed inflammation of the cervix. Before this, I was tested for STDs, and only Ganderella was found. I went to another doctor. She said that there was no erosion at all, applied something and immediately diagnosed HPV. She prescribed me a course of treatment for HPV: 1) Superlymph suppositories at night for 20 days. 2) Immunomodulator Isoprinosin (I bought Groprinosin, they said it was the same thing). 28 days, 2 tablets. 3 times a day In addition, I visited a urologist because I have problems with urination. A urine culture tank showed E. coli 1x10 in 2 tbsp. The urologist supplemented the treatment with the drug URO-VAXOM (take it for at least a month). A simple analysis showed bacteria +++ and red blood cells unchanged 3-4 in the PZR. Before this, I was treated with Suprax-solutab, which gave temporary relief. On the 3rd day of taking these drugs together, I started bleeding. I continued therapy. On the 4th day I started bleeding more heavily, almost the same as during menstruation, with clots. Your period should come only in 2 weeks. Tell me, please, what could have caused such a reaction? Which drug should be discontinued? Or continue treatment? It also happened before that there was bleeding, but not so much. I'm very afraid of bleeding. Thanks in advance for the information provided!
What it is?
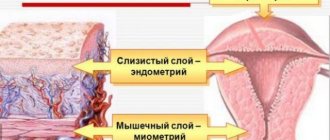
Putting sutures on the cervix is a necessary necessity, which gives a real chance to preserve and prolong pregnancy if the cervix for some reason cannot cope with its direct responsibilities. After conception has taken place, the cervix closes tightly. The cervical canal closes and fills with mucus. The task facing this part of the female reproductive organ is large and important - to keep the growing fetus in the uterine cavity and prevent it from leaving it prematurely.
In addition to retention, the cervix with a mucus plug prevents pathogenic bacteria, viruses, and other unpleasant uninvited “guests” from entering the uterine cavity from the vagina, which can cause intrauterine infection of the baby. This is dangerous, because infections suffered in the embryonic and later periods usually result in developmental defects and severe congenital pathologies, and intrauterine death of the baby.
If the cervix does not provide adequate protection to the growing baby, the likelihood of miscarriage and premature birth increases. If by this time the baby is not yet able to survive on his own in this world, then such a birth will end tragically. In order to strengthen a weak neck, doctors recommend in certain situations to sutured it so that the mechanical barrier in the form of sutures prevents it from opening prematurely.
Main indications for the procedure
Of course, there are situations when cervical stitches are simply necessary. Indications for the procedure are as follows:
- Isthmic-cervical insufficiency is a pathology that is accompanied by expansion or shortening. A similar phenomenon develops with anatomical defects of the cervix, which in turn can be associated with mechanical damage, previous inflammatory diseases, cancer, etc.
- Hormonal imbalances, because it is hormones that control the condition of the walls of the reproductive organ. A change in the amount of certain hormones in the blood can cause relaxation or contraction of the muscles of the uterus, and early opening of the cervix.
- If the patient’s history includes information about previous miscarriages or premature births, then the doctor will probably closely monitor the patient’s health and, if necessary, prescribe surgical intervention.
A suture on the cervix during pregnancy can ensure the normal development of the child. However, only an experienced obstetrician-gynecologist is able to decide on the procedure.
Indications
For this type of surgical intervention during pregnancy there must be strict indications and clear recommendations from the attending physician. These factors include:
- high risk of miscarriage or premature birth due to the presence of similar cases in the anamnesis;
- recurrent miscarriage in the 1st and 2nd trimesters of pregnancy;
- miscarriage in the third trimester;
- earlier shortening and opening of the cervix, expansion of the internal or external pharynx;
- dubious scars left as “memories” from previous births in which cervical ruptures occurred;
- any destructive changes in the cervix during the process of bearing a child, which are prone to further development.
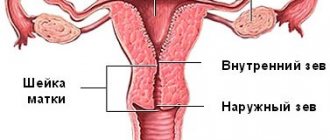
The doctor cannot make a decision that there is a need for such an extreme measure as suturing based on an examination on the gynecological chair alone. He needs comprehensive information about the condition of the lower segment of the uterus, which is the cervix. For this purpose, a full biometric examination , which includes colposcopy and ultrasound diagnostics, as well as laboratory smear testing.
Only after all risk factors have been identified, the length and width of the cervix have been measured, the condition of the cervical canal inside it has been assessed, as well as the patient’s personal history, can a decision be made about suturing the cervix.
When and why is the cervix sutured during pregnancy?
If pregnancy proceeds within normal limits, the cervix will open only after the baby is ready for birth, when all organs can function independently. If any pathological processes are observed in the body that lead to premature opening of the pharynx, then suturing the cervix during pregnancy will be the optimal solution.
Stitching during gestation has strict indications and, first of all, the situation is determined by the diagnosis of isthmic-cervical insufficiency (ICI). The pathology is characterized by weak muscles of the uterine pharynx, softening and shortening, which threatens the life of an unformed baby.
Reasons for the development of ICN:
- excess of androgens;
- congenital malformation;
- presence of previous births;
- numerous abortions.
As a result of the fact that the cervix becomes shorter and softer, the risk of infections entering the fetus increases significantly, and amniotic fluid begins to gradually leak. Therefore, from the 14th to the 25th week, the cervix is sutured.
Contraindications
Suturing this organ during pregnancy is possible only if, apart from a weak cervix, no other global problems have been identified in this pregnancy. If some concomitant pathologies are detected, the operation will have to be abandoned. Contraindications include:
- diseases of the heart and blood vessels, kidneys, which have worsened in the expectant mother due to pregnancy, the risk of death of the woman in the event of mechanical prolongation of pregnancy;
- bleeding, increasing in strength and character, as well as recurrent bleeding when there is a threat;
- gross malformations of the baby;
- hypertonicity of the uterine muscles, which cannot be reduced with medical conservative treatment;
- chronic inflammation of the female reproductive organs, the presence of sexually transmitted infections, STDs;
- late detection of cervical pathologies - after the 22nd week of pregnancy (the best time for successful intervention is considered to be the period from 14 to 21 weeks).
When and why is the cervix sutured during pregnancy?
If pregnancy proceeds within normal limits, the cervix will open only after the baby is ready for birth, when all organs can function independently. If any pathological processes are observed in the body that lead to premature opening of the pharynx, then suturing the cervix during pregnancy will be the optimal solution.
Stitching during gestation has strict indications and, first of all, the situation is determined by the diagnosis of isthmic-cervical insufficiency (ICI). The pathology is characterized by weak muscles of the uterine pharynx, softening and shortening, which threatens the life of an unformed baby.
Reasons for the development of ICN:
- excess of androgens;
- congenital malformation;
- presence of previous births;
- numerous abortions.
As a result of the fact that the cervix becomes shorter and softer, the risk of infections entering the fetus increases significantly, and amniotic fluid begins to gradually leak. Therefore, from the 14th to the 25th week, the cervix is sutured.
How is the operation performed?
The timing of the operation is of great importance. From 14 to 21 weeks, the child is not so large as to greatly stretch the walls of the uterus and the muscles of the cervix; at later stages, suturing is not recommended due to the fact that highly stretched tissues may not be able to withstand and the sutures will cut through with subsequent rupture.
The operation, which in medical language is called “cervical cerclage ,” is performed only in a hospital. It is not considered painful or excruciating because the woman is given an epidural or intravenous anesthesia.
There is no need to be afraid of it, because experienced anesthesiologists will calculate the dosage of drugs solely taking into account the gestational age, physique, weight and health status of the expectant mother herself and the developmental characteristics of her baby. The dose will be safe for mother and fetus.
The duration of the entire manipulation does not exceed a quarter of an hour. Depending on the condition of the cervix, the doctor will suture either the external or internal os of the cervix. The external one will not be touched if there is erosion, dysplasia, or pseudo-erosion on the cervix. The technique is very simple - surgeons suture the edges of the outer part of the neck together with strong surgical threads.
This method requires careful preparation. If there is an infection in the uterus, the consequences will be more than dire. Stitching will create a closed space inside the female reproductive organ in which any microbe can begin to multiply quickly. The woman is first treated with antibiotics, and the vagina is thoroughly sanitized. However, this does not always help.
There will be no closed space if the doctor decides to sew up the internal os of the cervix. In this case, specialists leave a small drainage hole. The sutures themselves are applied in different ways, each surgeon has his own favorite, and much depends on the anatomical characteristics of the patient.
The cerclage itself can be performed laparoscopically. It has many advantages - speed, fairly easy postoperative period, low blood loss, lower risk of complications.
Laparoscopic cerclage is indicated for women with congenital shortening of the cervix and those who have had unsuccessful vaginal suturing surgery.
Possible problems and complications
Like any surgical procedure, cerclage can also have its complications. The most dangerous are considered to be the addition of an infection, the development of an inflammatory process and an increase in the tone of the uterine muscles. Inflammation may develop due to an internal infection that could not be “defeated” in the preoperative period. Sometimes a woman has an individual allergic reaction to the suture material used by doctors.
Possible problems may be indicated by prolonged discharge after surgery, the appearance of a burning sensation, and mild pain . Moreover, inflammation can appear not only immediately after surgery, but also several weeks after suturing. This is why it is important to visit your doctor more often and monitor any changes.
Hypertonicity is also a reaction of the uterus to surgical intervention and suture material foreign to its structures. Some heaviness in the abdomen, slight tugging sensations may be quite normal in the first time after surgery, but subsequently they should disappear. If this does not happen, you should inform your doctor.
It’s not common, but it also happens that a woman’s body categorically refuses to accept a foreign body, which is surgical threads, and a violent immune process of rejection begins, which can be accompanied by high fever, atypical discharge, and pain.
In the later stages, cerclage can have another unpleasant consequence - the sutured cervix can be seriously damaged if labor has already begun and the stitches have not yet been removed. Therefore, it is important not to ask the doctor to “stay at home for another week,” but to go to the hospital in advance.
Reviews from doctors and patients about surgery
Of course, a lot of useful information can be obtained by talking with women who have had a stitch on the cervix during pregnancy. Reviews about the procedure, by the way, are mostly positive. Many experts argue that sometimes such surgical intervention is the only way to save a child’s life and give him enough time for normal development.
Women also leave positive reviews. The procedure is easy - only in the first days after the operation some discomfort is possible. Of course, there is a possibility of complications developing. Here, a lot depends on the competence, experience and skills of the doctor, and therefore pregnant women can only be advised to take a responsible approach to the choice of a specialist and strictly follow all his recommendations after suturing.
Removal of suture material is carried out without anesthesia - this procedure may not be very pleasant, but it is painless and quick. In most cases, birth occurs on the same day. But even if there are no contractions, the woman should be in a hospital setting.
Recommendations for the postoperative period
After the intervention, the woman needs to remain under 24-hour medical supervision in the hospital for several more days. She is prescribed antispasmodic drugs to reduce the muscle tone of the uterus, as well as strict bed rest. The vagina is sanitized daily to avoid infection. After this, the pregnant woman can be sent home. Discharge after the intervention continues for approximately 3-5 days.
Stitches on the cervix will require the expectant mother to reconsider her lifestyle until the very birth. Physical activity, prolonged standing in an upright position, and prolonged walking are contraindicated. Under no circumstances should you lift heavy objects. You should also abstain from sexual activity so as not to provoke hypertonicity of the uterus, which can lead to the cutting of sutures.
Until childbirth, a woman will have to monitor her stool - constipation is extremely undesirable, since pushing is prohibited. Therefore, you will have to go on a diet, introduce more fresh vegetables and fruits, juices into your diet, limit salt, an abundance of protein foods, as well as baked goods.
You will have to go to the doctor more often than women in an “interesting situation” usually do. The doctor will monitor the condition of the sutures, take smears for the vaginal microflora, and, if necessary, prescribe unscheduled ultrasound examinations, the purpose of which will be to measure the parameters of the cervix and evaluate its internal structures.
A woman with stitches on the uterus will have to go to the maternity hospital at 36-37 weeks . Around this time, the sutures are removed. Labor can begin at any time after this, even on the same day.
It is not painful to remove the sutures; there is no need to use anesthesia or other anesthesia methods.
Reviews
In general, women tolerate this intervention well. Reviews from those who have undergone cervical suturing are positive - they managed to deliver the long-awaited babies to the scheduled date. Among the disadvantages, women point out a large number of prohibitions that are imposed on everyday life after such an operation. Almost all patients note that the increased tone of the uterus persisted for a long time, which caused a lot of psychological and physical inconvenience and anxiety.
Not all of the pregnant women and young mothers who left reviews about cervical cerclage agreed to undergo the operation upon referral to a public hospital. Some consciously choose private and paid medicine. Many clinics in Russia perform such operations.
Their cost is around 50 thousand rubles, not counting preliminary tests, and quite a lot of them are required.
For those who are thinking about applying sutures to dilate the internal or external os of the cervix in a private clinic, experienced mothers advise choosing an institution that employs good specialists, because the outcome of the operation largely depends on the qualifications of the doctor. You should not make a hasty choice; you should carefully read the reviews about a particular clinic.
medical reviewer, psychosomatics specialist, mother of 4 children
- diseases of the heart and blood vessels, kidneys, which have worsened in the expectant mother due to pregnancy, the risk of death of the woman in the event of mechanical prolongation of pregnancy;
- bleeding, increasing in strength and character, as well as recurrent bleeding when there is a threat;
- gross malformations of the baby;
- hypertonicity of the uterine muscles, which cannot be reduced with medical conservative treatment;
- chronic inflammation of the female reproductive organs, the presence of sexually transmitted infections, STDs;
- late detection of cervical pathologies - after the 22nd week of pregnancy (the best time for successful intervention is considered to be the period from 14 to 21 weeks).
When is surgery prescribed?
Suturing the cervix is used as a result of lengthy diagnostics and additional studies (ultrasound, transvaginal sonography). To avoid putting either the baby inside the womb or the expectant mother at risk, many factors are taken into account when deciding whether to have surgery:
- length 20 mm or less;
- expansion and density of the internal pharynx;
- the gestation period is no earlier than 14 weeks and no later than 25;
- preservation of the amniotic sac and absence of leakage of amniotic fluid;
- absence of infectious diseases.
If the patient has poor blood clotting or bleeding is detected, then suturing will be contraindicated. In this case, drug therapy is used, the pregnant woman is put on hold, and maximum rest and rest are prescribed.