What size of ovaries during menopause are considered normal?
When menopause occurs, a woman’s body experiences many changes that are associated with hormonal changes. Most often, this process begins at 40-45 years of age and ends closer to 50. The functioning of the ovaries, which secrete sex hormones, stops gradually. Against the background of these changes, other unpleasant symptoms develop. Most often these are hot flashes, headaches, increased blood pressure, etc. When examining the pelvic organs (in particular, the ovaries), changes in their size, structure and other indicators are observed. On this basis, a conclusion is made about the presence of menopause and its normal or pathological course.
Correct interpretation of ultrasound of the pelvic organs
Ultrasound of the pelvic organs is the most accessible method for diagnosing many gynecological diseases.
Most often, a gynecologist advises to carry out this study if, after examining the patient, some points remain unclear, or if the woman is bothered by pain in the uterus, appendages, lower back, or if bleeding appears that is not associated with menstruation. In addition, such an examination of the pelvic organs is prescribed to confirm an intrauterine or ectopic pregnancy.
Ultrasound examination allows you to get a more accurate picture of the internal organs, as well as the tissues surrounding them. Moreover, it allows us to identify even the slightest deviations in their structure, which indicates the presence of a disease.
Today, ultrasound of the pelvic organs is performed using two methods: transabdominal and transvaginal. The latter type is characterized by high sensitivity and great accuracy.
Interpretation of uterine examination
It is worth noting that the correct interpretation of an ultrasound examination is the prerogative of the doctor, but the main parameters can be interpreted independently:
- The position of the uterus is normally slightly tilted forward (anteflexio). If the uterus is tilted back, this is an abnormal position and can cause some complications during pregnancy.
- External contours - in normal condition, the contours of the uterus should have smooth and clear outlines. If some vagueness is detected during the examination of the pelvic organs, this may indicate the presence of diseases: a tumor or fibroids. Blurred contours indicate inflammation of the surrounding tissues (parametritis).
- Dimensions of the uterus - it has been established that this organ is pear-shaped. In middle-aged women, the length of the uterus averages from 4.5 to 6.7 cm, thickness from 3.0 to 4.0 cm, and width from 4.6 to 6.4 cm. It is worth noting that in In the postmenopausal period, the uterus significantly decreases in size and after 20 years it can change significantly and have the following indicators: length up to 4.2 cm, thickness - 3.0 cm, and width no more than 4.4 cm.
- Structure - echogenicity of the walls of the uterus during ultrasound of the pelvic organs should be homogeneous. If hyperechoic formations were detected in the myometrium, this may indicate the presence of tumors or fibroids.
- Dimensions and structure of the cervix - length should be from 35 to 40 mm, anteroposterior size up to 30 mm. The cervical canal (endocervix) should be up to 3 mm in diameter. Enlargement of the cervical canal and uterus may indicate the presence of a very serious disease - cancer or endometriosis.
Condition and size of the ovaries
An ultrasound of the pelvic organs also demonstrates the condition of the ovaries. These organs are directly responsible for successful conception, since it is in them that the egg follicles mature, which are then fertilized by sperm.
Normally, the ovaries are the following sizes:
- width - 25 mm,
- length - 30 mm,
- thickness 15 mm.
- The volume of the ovary can vary from 2 to 8 cm cubic.
If an ultrasound of the pelvic organs shows an increase in these indicators, then we can talk about the presence of a disease such as polycystic disease or inflammation of the ovaries (oophoritis).
Due to the growing follicles, the contours of the ovary are uneven (lumpy), but at the same time their edges should be clear. The echostructure is homogeneous, with small areas of fibrosis. Changes in the echostructure of the ovaries and contours indicate an inflammatory process.
In healthy ovaries, a certain number of follicles with small sizes up to 6 mm should be detected during an ultrasound of the pelvic organs.
In addition, one dominant follicle should clearly differ in size (up to 25 mm), but it reaches this size only in the middle of the menstrual cycle.
If the transcript indicates that it is large in size, then this may indicate the presence of a follicular cyst.
Ultrasound of the fallopian tubes
Normally, during an ultrasound, the fallopian tubes are barely visible or not visible at all. If inflammation or thickening of the walls is observed, they are visualized during an ultrasound of the pelvic organs. They also become visible during an ectopic pregnancy.
Scanogram of the ovaries and uterus against the background of diseases:
Endometriosis - manifests itself during an ultrasound of the pelvic organs in the form of small bubbles in the muscular layer of the uterus, as well as in the cervix and fallopian tubes.
Myoma is a disease diagnosed using ultrasound. The uterus has an increased size, its contours are changed, and the presence of a node in the myometrium is also observed.
Malformations of the uterus (bicornuate, hypoplasia, saddle-shaped, etc.) are also diagnosed at the time of ultrasound of the pelvic organs. As a rule, the contours of the uterine body are greatly deformed, and pathological changes are observed in its cavity.
On an ultrasound of the pelvic organs, polyps are detected quite easily, since the contour of the uterus is changed, and formations are visible in its cavity.
Cancer - this disease is also diagnosed using an ultrasound scan of the pelvic organs. As a result of the study, a change in the contours of the organ is observed, as well as the presence of edema and space-occupying formation.
Endometritis is a slight increase in the size of the uterus, some thickening of the walls and slight swelling are also observed.
Cervical cancer – deformation and enlargement of the cervix.
Ovarian cyst - during an ultrasound of the pelvic organs, a formation with a diameter of up to 25 mm is noticeable, and a change in the contours of the ovary is also observed.
Polycystic ovary syndrome - an increase in the overall size of the ovary, thickening of the walls, and the formation of areas of fibrosis.
Inflammation of the appendages - ultrasound of the pelvic organs diagnoses thickening of the walls of the ovary, an increase in its size. Moreover, the edges of the appendages have unclear boundaries and their movement is limited.
Ovarian cancer – enlargement and deformation of the appendages.
It is worth noting that every doctor conducting a study must perform a procedure such as deciphering the results. However, for a more accurate diagnosis, just one study is not enough; you also need to carry out the necessary tests that will confirm or refute the result of the scanogram.
Source: https://delaiuzi.ru/organov-taza/rasshifrouka
Features of the functioning of the ovaries
The ovaries are paired glands that are designed to produce female reproductive cells (eggs). They are located on both sides of the uterus and are clearly visible during an ultrasound examination. The ovaries begin their work with the first onset of menstruation, when a girl reaches the age of 12-14 years. Every month, eggs mature in the ovarian follicles. Over the course of her life, a woman produces hundreds of germ cells, most of which remain unfertilized. In this case, the menstrual cycle will end with menstruation, which signals the process of resuming reproductive function.
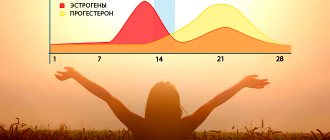
To ensure the process of childbearing, a woman's ovaries produce estrogen. Thanks to this hormone, the follicles where the egg is located matures. Higher concentrations of estrogen are observed in the first half of the menstrual cycle. Subsequently, a corpus luteum is formed at the site where the egg is released, which secretes progesterone. The combination of these hormones in optimal concentration ensures reproductive function, which is possible with normal ovarian function.
The onset of menopause occurs when this system begins to reduce the intensity of its work. This happens differently for every woman and is determined by many factors. It has been established that the duration of the functioning of the ovaries depends on their supply of eggs, which is called ovarian reserve. It is determined during intrauterine development at approximately 16 weeks of fetal life. Throughout a woman's life, the number of eggs decreases rapidly.
Menopause occurs when the ovarian follicular reserves are completely depleted. This is accompanied by a lack of eggs ready for fertilization. This process is influenced not only by the woman’s age, but also by many external factors. Some diseases, lifestyle, environmental conditions, dietary habits, stress and much more have a negative impact on the reproductive system.
Ovarian volume: normal, how to calculate, formula
Every woman takes care of her own health, especially during reproductive age. After all, if the functioning of at least one organ of the system is disrupted, the consequence may be childlessness. The ovaries are the gland of the reproductive system.
The organ is located at an equal distance on both sides of the uterus in the pelvis. The normal volume of ovaries in a healthy woman may vary. However, a discrepancy indicates some kind of disease.
Whether the organs are healthy can only be checked with an ultrasound.
Normal ovarian volume in women
Nature has endowed only female representatives with such organs. In them, eggs are fully formed, developed and mature. Every woman has a pair of ovaries in the pelvis on both sides of the uterus. This makes it easier for the doctor to work during an ultrasound examination.
If the girl is healthy, then the appendage has a slightly flattened shape, but it is quite dynamic and can be seen during examination. If the organs are pressed, then they function normally. The volume of the ovaries, right and left, is slightly different, this is quite normal.
This is especially evident in girls of reproductive age. But this does not prevent them from functioning normally.
The size of a woman's ovaries is determined by:
- Age.
- The number of pregnancies that result in childbirth.
- Stage of menstruation and taking oral contraception.
In relation to each other, the volume of female organs can vary greatly.
During reproductive age
The normal size in the ovarian zone is different for each woman. It depends on the effects of hormones and the health of the body. A difference between the right and left organs is possible, but only 2-3 mm.
An unexpected change in size may indicate the formation of a neoplasm or an inflammatory process.
Various circumstances throughout a woman’s menstrual cycle can also affect the parameters of the organ.
Normal volume in women according to ultrasound during childbearing age is expressed in the following figures:
- thickness – 15-21 mm;
- length – 19-36 mm;
- width – 17-29;
- Normal volume is 3-9 cm cubic.
In a normal state, sizes may differ, so to make a diagnosis, the doctor is guided by more than just one factor. For this, a full examination is carried out.
During menopause
Closer to menopause, reproductive function dies out, which is reflected in the volume of the organ. The glands become smaller, however, not both at once. With the onset of postmenopause, the appendages acquire the same size.
Standard sizes during menopause are as follows:
- thickness – 8-11 mm;
- width – 11-14 mm;
- length – 19-24 mm;
- volume – 2-4 cm cubic.
After menopause, over the course of several years, organs may change in size by 3 mm - an acceptable deviation. This is due to the continued production of single follicles.
How to calculate ovarian volume
In some cases, it is necessary to determine the size of the organ. The following formula will help you calculate the volume of the ovary:
0.532 × length × width × thickness = volume
In this way, the ovarian reserve in the female body is currently determined (the number of eggs ready for fertilization). For example, if the size is less than 8 cm, then the ovarian reserve is reduced. If the size is more than 12 cm, the indicator is high.
Normal size of the ovaries of a woman of reproductive age
In healthy women of reproductive age, the ovaries are oval in shape and have a developed follicular apparatus. During ultrasound diagnostics, the follicles are clearly visible.
Their characteristics largely depend on the day of the menstrual cycle. Approximately 8-9 days after the onset of menstruation, the dominant follicle is already visible, from which the egg will subsequently be released. It reaches a diameter of 15 mm, while the rest rarely exceed 10 mm. When ovulation occurs, the size of the dominant follicle is 18-24 mm.
The size of the ovaries in a woman of reproductive age is as follows:
- length – about 20-35 mm;
- width – 15-20 mm;
- thickness – 20-25 mm.
The size of the ovaries may vary slightly in one direction or another depending on the phase of the menstrual cycle.
Ovarian volume (right or left): normal, increase, how to calculate using the formula – Women’s question
On the other hand, in some cases there are women who even at the age of 25 have “low-quality” eggs and even need donor eggs.
These extreme examples, however, quite existing, led to the need for some way to assess the quantity and quality of eggs in women of different age groups.
It was for this purpose that the concept of “ovarian reserve” was introduced, since it became necessary to evaluate a woman’s reproductive age, not as the absolute number of years from the date of her birth, but as her real existing ability to become pregnant.
Ovarian reserve is the number of eggs in women at a given time that can be used for fertilization.
But how to count them, they are located in the ovaries? For this purpose, a number of functional tests have been proposed, which you can learn a little about in this section.
Ovarian volume: normal and abnormal
For every woman of childbearing age, it is very important to know the health of her internal organs, especially the ovaries. This is no coincidence, because a woman’s ability to have children depends on them. Let's consider the main parameters and indicators that the ovaries of a healthy woman should have.
Anatomical characteristics
Features of the structure of female ovaries
Only women are endowed with ovaries by nature, which is associated with the function of childbirth. The ovaries are a special type of female gland where the complete formation, development and maturation of eggs occurs. Every woman has two paired ovaries in her body, located in the abdominal cavity.
By location, the paired ovaries occupy a position on the sides of the uterus, due to which they become quite distinguishable during an ultrasound examination of the body. If, due to some circumstances, detection of one of the two ovaries becomes inaccessible, the doctor focuses on the area of the iliac vein.
Thus, under any circumstances related to a woman’s health, the ovaries are clearly visible in her body.
In a healthy woman, the shape of the ovary is somewhat flattened, but it is quite mobile and visible during examination. The flattened shape indicates their healthy condition. The size of the right and left ovary varies and this is normal. This is especially noticeable among representatives of the fair sex who are of reproductive age. At the same time, they fully perform the functions assigned to them.
The size of a woman's ovary is influenced by her age, the number of pregnancies with childbirth, the stages of menstruation and methods of preventing unwanted pregnancy by using oral contraceptives.
The size of one ovary relative to another can change and fluctuate significantly.
Features of the ovaries:
- The internal structure of the ovary has two layers: the cortex and the medulla. Both layers are clearly visible when examined in detail through special magnifying devices.
- On the outside, each ovary is covered with a special layer of the tunica albuginea.
- The outer or cortical layer of the ovary is characterized by the presence of follicles of varying maturity. These follicles are represented by two main types: primary immature, also called primordial, and mature, also called prevoulatory. All types of follicles perform certain functions in the female body.
With the help of ultrasound examination, specialists can identify changes occurring in their structural structure, including those of a negative nature. Typically, such procedures are carried out during the first week of menstruation.
When conducting this type of study, specialists pay great attention to the volumetric indicators of each ovary. After all, the health status of each ovary depends on their numbers, and the type of a particular pathology in the body is determined.
Size of a healthy woman's ovaries
Normal ovarian volume
In a healthy woman, the size of the ovaries is within the following limits:
- Volume ranges from 4 to 10 cubic centimeters
- Width varies from 18 to 30 millimeters
- Thickness ranges from 16 to 22 millimeters
- Length ranges from 20 to 37 millimeters
For a more detailed examination of the internal structure, the anatomy of the ovaries is examined taking into account the phases of menstruation.
In a woman in the early follicular phase, which falls between the fifth and seventh days of the menstrual cycle, ultrasound examination shows a white capsule with ten follicles located on the periphery, measuring up to six millimeters.
Already in the middle follicular stage, which falls on the tenth menstrual day, a dominant follicle is clearly visible, reaching a size of fifteen millimeters. This follicle does not end its development here, but continues to develop further.
The smaller follicular cells located nearby finish developing in the female body. This happens even if they have gained about ten millimeters.
The late follicular stage, which falls on the fourteenth menstrual day, is a period of active growth of the dominant follicle.
Sometimes the growth process of a given follicle becomes so active that the increase occurs by several millimeters every day.
When an actively growing follicle becomes eighteen millimeters in size, doctors note the rapid process of ovulation in the body.
This usually occurs when the follicle reaches eighteen millimeters in size. At the same time, the ongoing changes in the structure of its internal and external structure become noticeable.
In addition to the follicular stage, the luteal phases play a special role:
- So, in the early luteal phase, which falls on the fifteenth day, the corpus luteum is formed in the female body. Its dimensions range from fifteen to twenty millimeters. All this happens at the ovulation position.
- With the onset of the middle luteal stage, the active and rapid growth of the corpus luteum begins in the female body. Typically, this process occurs during the twentieth day of the menstrual cycle. The corpus luteum grows, acquiring size indicators ranging from 25 to 27 millimeters.
- Then the late luteal phase begins, ending on the twenty-seventh day. During its period, the process of reduction of the corpus luteum and its slow extinction are clearly evident. It becomes similar to a ten millimeter object. As soon as a woman begins menstruation, the fading corpus luteum completely disappears.
Source: https://iemc.ru/zabolevaniya-yaichnikov/obem-yaichnika-pravogo-ili-levogo-norma-uvelichenie-kak-rasschitat-po-formule.html
Ovaries at the onset of menopause
The first changes in the ovaries are observed during premenopause, when all the unpleasant symptoms of menopause appear. At this time, long delays occur, which is explained by a decrease in the concentration of sex hormones. At this time, connective tissue begins to predominate in the ovaries. It replaces the cortex, which is rich in follicles. The ovaries also become significantly smaller during menopause. During this period their size is as follows:
- length – no more than 25 mm;
- width – no more than 15 mm;
- thickness – about 9-12 mm.
Every month these parameters change even more downwards. Also, as menopausal processes progress, the difference between the sizes of the right and left ovaries is eliminated. In women, the reproductive organs are slightly different, which is quite normal.
Changes in the ovaries during menopause are even more significant. After the cessation of menstruation after 1 year, their volume does not exceed 4.5 cubic meters. cm. If the postmenopausal period lasts about 5 years, this figure is 2.5 cubic meters. cm, and after 10 years - 1.5 cubic meters. cm. When examining a 60-year-old woman, it is possible to reveal that the weight of one ovary on average does not exceed 4 g. For example, at 40 years old this figure is 9.5 g.
Also, with the onset of menopause, there is a gradual decrease in the number of follicles in the ovaries, after which they disappear altogether. Against the background of such changes, the female gonads become less susceptible to the effects of pituitary hormones (FSH, LH). Usually these substances are released in large quantities, but this does not lead to the maturation of the follicles.
They can be detected during ultrasound examination only at the beginning of menopausal changes in a woman’s body. In some cases, a certain number of follicles still remain in the ovaries even after prolonged menopause. However, they cannot develop normally, which eliminates the possibility of ovulation. In this case, when examining a woman’s urine, an increased content of estrogen is detected. Also, the function of producing this hormone in small quantities is carried out by the adrenal glands.
Ovarian reserve
A woman’s age is one of the important factors influencing the effectiveness of ART methods, since this parameter is directly related to the quality of the eggs located in the ovaries.
This parameter is not absolute, since a 45-year-old woman could have good quality eggs and still be fertile at this point - although this particular situation is more unusual than usual.
On the other hand, in some cases there are women who even at the age of 25 have “low-quality” eggs, even needing donor eggs.
These extreme examples, however, quite existing, led to the need for some way to assess the quantity and quality of eggs in women of different age groups.
It was for this purpose that the concept of “ovarian reserve” was introduced, since it became necessary to evaluate a woman’s reproductive age, not as the absolute number of years from the date of her birth, but as her real existing ability to become pregnant.
Ovarian reserve is the number of eggs in women at a given time that can be used for fertilization.
But how to count them, they are located in the ovaries? For this purpose, a number of functional tests have been proposed, which you can learn a little about in this section.
Counting the number of antral follicles
Antral follicles are small follicles (2-8 mm in diameter) that we can see, measure and count using ultrasound. Transvaginal ultrasound is the optimal method for counting these small structures.
The fact is that the number of antral follicles has a direct relationship with the number of primordial follicles, visible only during microscopic examination, located in the ovaries. Each primordial follicle contains a precursor to an egg, which may become one in the future.
Thus, counting antral follicles visible on ultrasound replaces microscopic examination of the ovaries for accurate assessment of the number of oocyte precursors.
Counting antral follicles using ultrasound is a simple and accessible method for assessing ovarian reserve.
Figure 1 on the left shows an ovary (outlined in blue) in which antral follicles were counted at the beginning of the menstrual cycle (outlined in red). In this projection of the ovary, 16 such follicles are visible.
What is the “good” number of antral follicles?
Based on a number of studies by foreign authors, the following pattern has been revealed:
| Number of antral follicles | Expected response to ovulation stimulation and the effectiveness of ART techniques |
| Less than 4 | Very low quantity. Poor or no response to stimulation. Enrollment in an IVF program should be seriously considered. Very low chance of pregnancy. |
| 4-7 | Low quantity. There may be a slight response to stimulation. It is preferable to use very high doses of FSH for stimulation. Unsuccessful attempts. |
| 8-10 | Slightly reduced quantity. A large number of unsuccessful attempts. |
| 11-14 | Normal (but average) amount. The response to stimulation is reduced, but, as a rule, sufficient. Group with a favorable prognosis for pregnancy. |
| 15-26 | Normal good quantity. Excellent response to ovulation stimulation. It is preferable to use low doses of FSH. Best efficiency. |
| More than 26 | A high amount characteristic of polycystic ovary syndrome. The use of low doses is necessary due to the risk of hyperstimulation syndrome. In some cases, the eggs are of low quality, which reduces the chance of pregnancy. |
follicle-stimulating hormone (FSH) on days 2-3 of the menstrual cycle
This indicator is also an important marker of the state of the ovarian reserve.
According to domestic data, the following concentration limits are distinguished:
- 3-8 IU/l is normal, a good response to stimulation is expected;
- 8-10 IU/l – the response can range from normal to moderately reduced;
- 10-12 IU/l – low ovarian reserve, reduced response to stimulation;
- 12-17 IU/l – poor response to stimulation and low pregnancy rate;
- More than 17 IU/l is a very poor response to stimulation.
Calculation of ovarian volume
The formula for calculating ovarian volume is as follows:
Ovarian volume = 0.532 x length x width x thickness.
What can data tell us about ovarian volume? If a woman has an ovarian volume of less than 8 cm?, then low ovarian reserve is assumed, if more than 12 cm? – high ovarian reserve.
anti-Mullerian hormone (AMH) and inhibin B
The most informative test is one that allows you to determine the content of anti-Mullerian hormone. In women, the production of this hormone occurs in granulosa cells and reaches a maximum in preantral and antral follicles 4 mm in diameter.
In larger follicles, as well as in follicles more than 8 mm in diameter, there is no secretion of this substance.
Figure 2 schematically shows the actions of AMH in the ovary:
The growth of follicles is shown schematically. It has been shown that anti-Mullerian hormone is produced by primary and preantral follicles and has mainly 2 types of effects on the ovary: 1 - suppresses the primary stages of follicular growth, 2 - suppresses FSH-dependent growth and selection of preantral and small antral follicles.
Based on a number of studies, it has been established that the content of AMH in the blood serum is directly related to the content of antral follicles, that is, based on the analysis data, the state of the ovarian reserve can be assessed. It has also been shown that the lower the content of this hormone in the blood, the worse the ovarian response to ovulation stimulation.
An interesting fact is that anti-Mullerian hormone can be used not only to assess the state of the ovarian reserve, but also to assess the pathophysiological state of the ovaries, for example, to confirm the presence of polycystic ovary syndrome, since in this disease the pool of small antral follicles is increased. This indicator can not only be a marker of the presence of the disease, but also a criterion that will allow assessing the severity of disorders in polycystic ovary syndrome.
The study of anti-Mullerian hormone content can be carried out on any day of the cycle, since its content practically does not change during the cycle.
According to other scientists, it is better to study the content of anti-Mullerian hormone on days 3-5 of the cycle.
These data can be used in preparation for ART in order to objectively assess the condition of the ovaries, as well as select the correct stimulation protocol.
Based on an assessment of a number of the above indicators, a conclusion can be made about the state of a woman’s ovarian reserve:
Low ovarian reserve is assumed if:
- the patient’s age exceeds 35 years;
- FSH level at 2-3 d.m.c. more than 10IU/l;
- the number of antral follicles is less than 10 mm in diameter at 2-3 d.m.c. less than 5 in each ovary;
- ovarian volume less than 8 cm³;
- low levels of anti-Mullerian hormone.
High ovarian reserve is expected if:
- the patient's age is less than 35 years;
- FSH level at 2-3 d.m.c. less than 8IU/l;
- the number of antral follicles is less than 10 mm. in diameter by 2-3 d.m.c. more than 10 in each ovary;
- ovarian volume more than 12 cm³;
- high levels of anti-Mullerian hormone.
Next: » Laparoscopy and IVF
See also:
Infertility treatment services at the “I’m Healthy!” Clinic
- Consultation with MD, professor of obstetrician-gynecologist
- Consultation with Ph.D. reproductive specialist
- Assessment of couple fertility and diagnosis of infertility factors
- Consultation with MD urologist-andrologist
- Examination of the spouse and preparation of a “fertility passport” in accordance with international standards
- Expert ultrasound of the pelvic organs with Doppler ultrasound
- Checking the patency of the fallopian tubes (ultrasonohysterography, hysterosalpingography)
- Assisted reproductive technologies (artificial insemination, IVF, ICSI, PIXI)
Step-by-step steps to diagnose infertility
Step-by-step steps for the IVF program
Source: https://www.ya-zdorova.ru/iskusstvennoe-oplodotvorenie/ovarian-reserve/
How can you prolong the functioning of your ovaries?
In some cases, doctors recommend artificially prolonging the functioning of the ovaries for a certain period. This is justified by the woman’s poor health, the presence of a large number of unpleasant symptoms that lead to partial or complete loss of ability to work. They also resort to drug therapy when a woman experiences menopause too early and wants to prolong her youth for a little while longer. In such cases, doctors prescribe the following drugs:
- in some cases, to ensure normal functioning of the ovaries, it is enough to change the diet to include foods containing phytoestrogens. They are present in many vegetables, fruits, and legumes. At the same time, it is recommended to completely avoid junk food – spicy, fatty, salty. It is also impossible to normalize the functioning of the ovaries without quality rest and reasonable physical activity;
- hormone replacement therapy. In especially severe cases, doctors recommend resorting to this to neutralize the imbalance in the body. Hormonal drugs are prescribed with caution and under close medical supervision, as they can cause dangerous side effects. When using the wrong product or the wrong dosage, the risk of developing tumors or other unpleasant diseases significantly increases. Popular hormonal drugs - Proginova, Divigel, Divina and others;
- preparations based on plant extracts. These drugs are prescribed by many doctors because there are no serious side effects when using them. They have a gentle effect on a woman’s body and help eliminate hormonal imbalances. Popular drugs from this group are Remens, Klimaktoplan, Klimadinon and others;
What causes the increase in ovarian size during menopause?
If, after ultrasound diagnostics, a significant increase in the size of the ovaries is revealed, it is necessary to undergo a more thorough examination. Normally, their volume should decrease due to the absence of follicles and the predominance of connective tissue. An increase in the size of the ovaries always signals the development of certain pathologies that carry potential danger.
These include:
- the appearance of cysts. Only in 30% of cases during menopause are two glands affected. Once menopause occurs, cysts are not functional. They are not able to resolve on their own. The only way to get rid of these cysts is through surgery. Most often they are epithelial, which are capable of malignant degeneration;
- polycystic ovary syndrome. This disease is characterized by the formation of multiple cysts. During menopause, polycystic disease develops more actively due to a critical decrease in estrogen levels and an increase in the concentration of male hormones. This negative process is facilitated by long-term use of oral contraceptives or hormone replacement therapy;
- cancer development. Ovarian cancer is the second leading cause of death among women of all ages. Most often, malignant processes begin precisely after the cessation of menstruation. In many cases, this is caused by the absence of childbirth, frequent abortions, and long-term use of hormonal drugs.
How to properly take care of your health during menopause?
With menopausal changes in the body, a gradual decline in the functioning of the ovaries occurs. But this is not a reason to neglect your own health. At this time, the woman is obliged to regularly visit the gynecologist for preventive examinations, which will help identify many dangerous diseases in the initial stages.
Also, diagnostic procedures should include ultrasound of the pelvic organs. It allows you to accurately determine the size of the ovaries, their structure, location and the presence of any neoplasms. Also, using this procedure, it is easy to identify other pathologies affecting the uterus, which is also not uncommon during menopause.
But sometimes it is very difficult to find the ovaries in a healthy woman and determine their condition during ultrasound diagnostics. Even with a full bladder, due to the lack of follicles, the gonads are almost not visualized. In this case, women are recommended to undergo a transvaginal ultrasound, which is more accurate.
The ovary is not visualized on ultrasound: why the organ is not visible during examination
Ultrasound diagnostics is an effective and accessible method for identifying pathology of the female genital organs. Read further in the article: the ovary is not visualized, what does this mean?
Localization of the ovaries
The ovaries are paired glands of the female reproductive system, located in the pelvis, on both sides of the uterus. Normally, the glands are located to the right and left of the midline of the abdomen in the groin area.
They are connected to the uterus and the walls of the small pelvis using connective tissue cords - ligaments in which the blood vessels and nerve fibers that feed them pass. The upper part of the glands is in contact with the fallopian tubes.
The collection of ovaries and fallopian tubes is called the appendages.
Although the gonads do not directly contact the abdominal cavity, loops of the large intestine are located above them. This localization feature often leads to the fact that the ovaries are not located during ultrasound examination of the pelvic organs due to shielding by the large intestine.
Features of structure and functioning
The ovaries are covered with a connective tissue membrane, under which the cortex and parenchyma of the organ are located. As the follicle matures, it moves to the edge of the ovary and during ovulation, the egg is released into the abdominal cavity where it is captured by the fallopian tubes.
The female gonads perform two main functions.
- Reproductive function . The ovaries contain eggs that mature during the monthly cycle. Unlike the male body, in which the formation of sperm occurs throughout life, the number of eggs in a woman is limited (about 1 million) and is laid during the period of intrauterine development. This is the so-called follicular reserve, which will be used up during the reproductive period of a woman’s life (from 13 to 55 years).
- Endocrine function . The gonads synthesize substances that determine the female hormonal profile: estrogens, progesterone, and also a small amount of androgens. The work of the ovaries is under the control of the hypothalamic-pituitary system, which produces luteinizing and follicle-stimulating hormones.
Normal parameters of the ovaries according to ultrasound
In the absence of pathological processes, the ovaries have a shape close to oval with smooth, clear contours. Their sizes average 19–40 mm in length and 16–30 mm in width. Changes in the boundaries of the gland are considered normal only at the time of ovulation and the release of the egg.
In addition to the size of the organ, the doctor evaluates the volume of the parenchyma and its structure. Normally, it has a uniform consistency and makes up approximately 2/3 of the total volume of the gland. The number of small follicles in the early stages of development is also counted.
For a successful pregnancy, their number must be at least 20. A decrease in their number is one of the evidence of depletion of the follicular reserve and the imminent onset of menopause.
Why are the ovaries not visible on ultrasound?
As a rule, ultrasound of the pelvic organs is performed in two ways: transabdominal and transvaginal.
During a transabdominal examination, the doctor places the device’s sensor on the anterior abdominal wall in the area where the uterus and appendages are projected onto it.
In some cases, to obtain a clearer picture, the study must be performed with a full bladder. To do this, an hour before the diagnosis you need to drink about a liter of liquid and after that do not visit the toilet.
During a transvaginal examination, the probe is inserted directly into the vagina. This method allows you to clearly visualize the appendages, uterus, and assess the condition of the endometrium. If there are contraindications for transvaginal examination, diagnostics can be performed by inserting a sensor into the rectum.
A specialist explains in this video what can be revealed during an ovarian ultrasound.
Possible reasons why the ovaries are not visualized on ultrasound
Let's consider the main reasons why the gonads are not visualized during diagnosis.
- Congenital malformations . The absence of one or both ovaries as a result of a genetic failure and underdevelopment of the glands. Pathology is detected in adolescence. The reason for visiting a gynecologist is the absence of menstruation.
- Ovariectomy . Surgical removal of glands if necessary to treat endometriosis, cysts, tumors, etc. The patient is usually aware of the situation and can inform the doctor about it.
- Significant reduction in the size of the glands . It is observed during menopause, when the process of involution (reverse development) and fatty degeneration of organs predominate in the female reproductive system. If a similar picture is observed in women of reproductive age, then this may indicate exhaustion of the reproductive system and early menopause.
- Abnormal location of organs . Most often, this situation is associated with some pathological process in the pelvis. Thus, with adhesive disease, one of the ovaries may be located behind the uterus or move upward, attracted by adhesions.
- Pregnancy . The increase in the size of the uterus, especially in late gestation, greatly complicates the visualization of the gonads.
- Screening with loops of the large intestine . The air environment is impenetrable to ultrasonic waves. A gas-inflated cecum is one of the possible reasons why the right ovary is not visualized during diagnosis.
Source: https://uzi.guru/mal-taz/womns/ov/fnmn/yaichnik-ne-vizualiziruetsya-chto-eto-znachit.html
How does the size of the ovaries change with the onset of menopause?
The ovaries play a very important role in the female reproductive system. Without their normal work, a lady will not be able to have children. During menopause, the ovaries stop working and decrease in size.
However, they are susceptible to various dangerous diseases, including the formation of cancerous tumors. In this publication we will look at how the size of the ovaries should normally change during menopause, what possible pathologies of this organ are possible, as well as methods for diagnosing its condition.
What functions do these organs perform?
The ovaries are oval-shaped organs of the female reproductive system. They are located on either side of the uterus. In the tissues of the ovaries there are special vesicles - follicles, intended for the development of eggs. They are clearly visible on ultrasound, and also produce female sex hormones: progesterone and estrogens.
From the first day of the menstrual cycle, the process of growth and maturation of follicles begins under the influence of estrogens. One follicle grows faster than the others. The egg matures in it, and it is called dominant. The growth of other follicles is slowed down. During ovulation, the follicle ruptures and the egg is released. The ruptured follicle transforms into the corpus luteum, which produces progesterone.
Under the influence of sex hormones, the reproductive function of a woman is ensured, and this is only possible with normal functioning of the ovaries. When the egg is fertilized, pregnancy occurs. If the egg is not fertilized, the menstrual cycle will end with menstruation.
A certain number of follicles are formed in the eggs of girls during intrauterine development. Over the entire reproductive period, hundreds of eggs mature, most of which remain unfertilized. When the supply of follicles in the ovaries is depleted, menopause occurs. Normally, menopause occurs at the age of 50.
How organ size changes during menopause
In women of reproductive age, the normal size of the ovaries has the following parameters:
- organ length – 20-35 mm;
- its width is 15-20 mm;
- thickness – 20-25 mm.
Both organs differ in size. This difference is considered normal. In a forty-year-old woman, the normal weight of one organ is 9.5 g.
During premenopause
The menopausal period has three stages, during which the ovaries change their size. The first stage is called perimenopause. It starts with the first symptoms of menopause - hot flashes, increased sweating, surges in blood pressure, excessive irritability and others. They are provoked by hormonal imbalance, which occurs due to the fact that the ovaries begin to produce fewer sex hormones.
During premenopause, the menstrual cycle is disrupted. It becomes shorter or longer, and the number of critical days and the abundance of menstrual flow also changes. Delays are more common in women. First for a few days, and then weeks and months. The amount of menstrual flow decreases and lasts fewer days.
The first changes in the ovaries occur in premenopause against the background of decreased estrogen levels. The number of remaining follicles decreases with each menstruation. The cortex, which previously contained follicles, is replaced by connective tissue.
The ovaries begin to decrease in size to the following parameters:
- length does not exceed 25 mm;
- width no more than 15 mm;
- thickness within 9-12 mm.
The ovaries are constantly decreasing in size. After a few months, both organs become the same size.
During menopause and postmenopause
During menopause, the last independent menstruation occurs. They can only be established retrospectively. Therefore, the diagnosis of menopause is made 12 months after menstruation, if there has been no menstrual flow. Throughout this year, the ovaries continue to decrease in size.
The following sizes of ovaries at menopause are considered the accepted norm:
- length is in the range of 20-25 mm;
- width – 12-15 mm;
- thickness – 9-12 mm.
The volume of the organ decreases to a value of 1.5-4 cm 3. In some women, the follicles in the ovaries during menopause still remain in small quantities, but they can no longer develop. Accordingly, ovulation does not occur. If a woman takes a urine test, it will reveal a high level of estrogen produced by the adrenal cortex.
Postmenopause is the final stage of the menopause. In postmenopause, menstrual function is completely absent. Many people are interested in what happens to the ovaries, the work of which is completely completed in the female body.
They continue to decrease in size. So, 5 years after the start of this stage, the volume of the ovaries will be approximately 2.5 cm3, and after 10 years - 1.5 cm3. The weight of the organ in a 60-year-old lady normally does not exceed 4 g.
How to calculate ovarian volume
The health of a woman’s reproductive system is very important for every representative of the fairer sex, especially if she plans to have children in the future. This is due to the fact that a disruption in the functioning of any organ will invariably lead to the development of various gynecological diseases, not excluding infertility.
The ovaries, which are glands, are responsible for the production of sex hormones, the process of egg maturation, as well as the release from the follicle.
Paired reproductive organs are located on both sides of the uterus, which in turn is located in the pelvis.
Some may be interested in how to calculate the volume of the ovary, since this parameter can change at different ages and the state of the female reproductive system.
Norms
Paired gonads in the form of ovaries are present only in females. Here, from beginning to end, the process of forming the development and maturation of eggs occurs. The most common method to check if there are any pathologies is an ultrasound examination of the pelvic organs.
What do the ovaries look like during ultrasound screening? Source: delaiuzi.ru
In the absence of diseases, the shape of the appendage will be slightly flattened. Since the organ is quite dynamic, it is well visualized during the examination, and if it is compressed, then we can say that it is functioning normally. It is worth saying that the volume of the right and left ovaries is definitely different, which is not a deviation.
The size of the gonad will be influenced by several factors: what age the woman is, how many pregnancies she has had that ended in labor, what period of the menstrual cycle is currently in progress, and whether oral contraception is used.
Reproductive age
Depending on the individual characteristics and structure of the female reproductive system, the size of the ovary will differ for each person. This indicator is also influenced by the general level of health, as well as the presence or absence of hormonal imbalance. As for the fluctuations between the sizes of the right and left appendage, they may differ by 2-3 mm up or down.
If this parameter significantly exceeds the normal limits, and this situation arose abruptly, then after an ultrasound examination the doctor will make a presumptive diagnosis, which will indicate a suspicion of the development of an inflammatory process or the formation of tumor formations.
The size of organs can change under the influence of various circumstances that occur to a woman throughout the menstrual cycle. When a girl is of childbearing age, the following parameters that correspond to the norm should be determined during an ultrasound:
- The thickness of the ovary can range from 15 to 21 mm;
- The length of the appendage should be between 19-36 mm;
- The width of the organ is 17-29 mm;
- The volume of the gonad should be from 3 to 9 cm3.
It is important to understand that if a woman has a normal level of reproductive health, then fluctuations in the size of the ovaries are not considered a pathology. To make a final diagnosis, the doctor must take into account several factors, which requires additional examinations.
During pregnancy
The period of bearing a child is associated with various transformations in a woman’s body, which definitely affect the reproductive system. The first thing that is clearly visualized is an increase in the size of all internal organs. This feature is inherent in every representative of the fairer sex in this state.
The ovaries are no exception, and changes in their parameters occur due to the acceleration of the blood circulation process. During pregnancy, the location of organs also changes. There is a displacement of the ovaries in the upper part of the small pelvis, as the uterus itself enlarges.
The volume of the gonad in women during pregnancy can range from one and a half to four cubic centimeters. The width of the organ reaches 12-15 mm, the length corresponds to 20-25 mm, and the thickness is 9-12 mm. All of these parameters are considered the norm for any healthy girl who is carrying a child.
During menopause
The menopausal period is also accompanied by serious changes in the body. First of all, the hormonal background changes, which is due to the decline of reproductive function. That is why women at this age experience a decrease in the volume of the gonads. The ovaries decrease in size, but not both at once.
What changes occur in the ovaries with age. Source: missis.info
After postmenopause occurs, the right and left organs will be the same size. As for the norms, they are as follows:
- The volume of the ovary should be 2-4 cm3;
- The length of the reproductive organ is in the range of 19-24 mm;
- The thickness of the paired gonad ranges from 8 to 11 mm;
- The width of the organ reaches 11-14 mm.
After a woman reaches menopause, the size of her ovaries will change over the course of several years. The permissible deviation is a fluctuation of 3 mm up or down. This individual feature is associated with the fact that single follicles are still being produced.
Formula
In the life of every woman, a situation may arise when she needs to calculate the size of the reproductive organ. For these purposes, you can resort to using a simple formula.
You need to take the only constant digit, then multiply it by the length.
The resulting number is multiplied by the width of the organ, and this result is also multiplied by the thickness of the organ, as a result you can get the volume.
Everything described is presented in the following form: 0.532 length width * thickness = volume.
Thanks to this, it is possible to determine as accurately as possible what kind of ovarian reserve an individual woman currently has. Ovarian reserve is the number of eggs that are ready for fertilization. If the indicator is less than 8, then it is considered underestimated, and if more than 12, then it is overestimated.
Pathologies
Often, during an ultrasound diagnostic examination, the doctor tells the patient that there is an enlargement of the ovaries. A significant deviation of parameters from the norm, in most cases, indicates the development of a serious pathological process. This condition cannot be left without timely and proper treatment.
Experts identify the following reasons why ovarian size changes:
- The production of a large number of follicles, which occurs with hormonal dysfunction;
- Polycystic ovary syndrome, which often affects organs on both sides at once;
- Progressive endometriosis, characterized by the growth of the mucous layer beyond the uterus, the formation of a cyst, and disruption of the stability of the menstrual cycle;
- An inflammatory process that affects the ovaries, during which they take on the shape of a ball (oophoritis or adnexitis);
- The development of a very rare pathology called ovarian pregnancy, which can affect two organs;
- Ovarian torsion requiring immediate surgical intervention;
- Formation of neoplasms of a benign or malignant nature.
It is necessary not only to be able to correctly calculate the volume of the ovary, but also to promptly identify deviations in the size of the organ. If the parameters have been increased, it is imperative to regularly visit a gynecologist, who should conduct certain examinations to help determine the cause of the development of this condition.
When an organ exceeds its normal size or increases in diameter very quickly, a consultation with an oncologist may be required. If the cause is determined in a timely manner, treatment will be quick and not associated with various complications. That is why women are advised to be attentive to the health of their reproductive system and not to neglect visits to the doctor.
Structure (video)
Source: https://uterus2.ru/other/kak-poschitat-obem-jaichnika.html
Pathologies during menopause
Normally, the ovaries should shrink. When an enlargement of organs is detected during ultrasound diagnostics, it is necessary to undergo a more thorough examination in order to diagnose the emerging pathology.
- Cyst. In menopausal women, only 30% have both organs affected. In the vast majority of cases, pathological changes occur in only one ovary - a follicular cyst is formed. These are round anechoic formations with a thin-walled capsule. They occur due to hormonal disorders and can resolve on their own over 2-3 menstrual cycles. When this does not happen, treatment is carried out. If an endometrioid cyst develops, it has a harder capsule and is capable of degenerating into a malignant neoplasm. Therefore, it is removed through surgery.
- Polycystic. With this disease, several cysts can form in the ovary at the same time. Such formation during menopause occurs more often than single cysts. This is due to the fact that the level of female sex hormones has decreased significantly, and the amount of male hormones, on the contrary, has increased. This result is caused by long-term use of oral contraceptives, which were not prescribed by a gynecologist and were not suitable for a particular body. Polycystic disease can be a side effect of taking hormone replacement therapy during menopause.
What does it mean that the ovary is not visualized: possible reasons
Thanks to the pelvic organs, the most important event in the life of every girl occurs - the onset of pregnancy, which the majority of the female population dreams of.
Therefore, after undergoing an ultrasound examination, some are shocked and puzzled by its results: what does “the ovary is not visualized” mean, what is it and is there any threat? The task facing a woman in such a situation is not to lose heart.
There are many reasons why the ovaries are not detected. They require more detailed consideration.
Anatomical location of the pelvic organs
Before considering the reasons why the ovaries are able to hide from view, it is necessary to understand the structure of the pelvic organs. It contains the following organs:
- rectum, through which processed food comes out,
- the bladder in contact with the walls of the vagina and uterus,
- the vagina, which is adjacent to the cervix and passes through the urogenital diaphragm,
- the uterus, which is pear-shaped and consists of muscles, performs the reproductive function,
- two ovaries, which produce hormones and are responsible for the maturation of eggs,
- fallopian tubes that connect to the ovaries on either side of the uterus.
Why are the ovaries not located on ultrasound?
The specialist may say that the ovaries are not located. What does it mean? Why is this happening? In simple words, if the ovary is not visible on an ultrasound, this means that the monitor shows the absence of an organ, i.e. it is not defined.
With its presence, on the ultrasound picture in the conclusion they write that they are determined.
In frequent cases, organs may not be located due to the incompetence of the gynecologist, who, due to his incompetence, simply could not see the organs on the monitor or adjust the sensors.
Normally, the contours of the ovaries in a healthy woman are uneven and clear. Fuzzy contours may indicate inflammation, cystic formations, or the presence of a corpus luteum. Blurred - they speak of a disease such as salpingoophoritis - inflammation of the uterine appendages. With a fuzzy outline and reduced size of the ovaries, the ultrasound picture indicates the probable onset of menopause.
Other cases of an undetectable left or right ovary include pathologies, endocrine disorders, and body characteristics.
Visualization also depends on the correctness of the ultrasound examination and the operation of the instruments.
During transabdominal ultrasound, the patient should drink a lot of water to fill the bladder, since if there is a lack of fluid, the left ovary may disappear behind the uterus.
Before a transvaginal ultrasound, you should empty yourself, because the sensor is inserted into the vagina and its location to the organs becomes close, and the liquid during this study makes it difficult to see what is happening inside.
Is it possible to do ultrasound diagnostics during menstruation? Read the article Ultrasound of the pelvic organs and menstruation
Intestinal disorders
The first most popular organic reason for not seeing the left or right ovary is a large accumulation of intestinal gases, flatulence, and fullness of the intestines after eating. As a rule, in the next study the organ appears in the field of view.
Previous surgical interventions
After gynecological operations, the organ is not located, because the stress suffered by the body can disrupt its functioning for a certain time, as a result of which the organ may shrink, down to the size of a pea.
Taking birth control pills
OK drugs are used to treat hormonal disorders and contraception. They suppress the hormones produced by the ovaries in order to prevent the eggs from maturing, thereby eliminating the possibility of ovulation for fertilization.
Since hormones are closely related to processes in the pelvis, internal organs may become invisible to the equipment due to the effect of hormonal pills on reproductive function. While taking contraceptives, ultrasound is less informative.
Anovulatory cycle
It happens that the ovary is not examined by a specialist during the examination due to the lack of ovulation. There are two reasons for its absence:
- temporary hormonal imbalance, in which the body’s normal state returns in the next menstrual cycle.
- serious hormonal disorders or pelvic diseases (for example, polycystic disease).
If more than two cycles in a row the ultrasound does not show a normal result, there is no ovulation, most likely it is necessary to examine the endocrine system.
Hormonal disorders
If the patient refuted the reasons listed above, and the ovary was not visualized after repeated examination, it is recommended to take tests for female sex hormones:
- FSH,
- Prolactin,
- Estradiol (estrogens),
- LG,
- AMG.
Remember! Only an experienced specialist can accurately determine the reason why the ovaries are not visualized
What diagnostics are needed after menopause?
In order not to miss the pathological processes occurring in the organs of the reproductive system, a woman should undergo a routine medical examination by a gynecologist at least once a year. Doctors advise doing it more often – once every six months. The doctor will conduct a gynecological examination and refer the lady for an ultrasound of the pelvic organs.
This study allows you to assess the condition of the ovaries and uterus. The specialist will determine the size and structure of the organs, and also assess compliance with normal parameters for a particular age. If a neoplasm appears on the organs, then with the help of this study it is possible to accurately determine its location and size.
A woman can always find time to visit a gynecologist if she wishes. Regular ultrasound examinations during menopause will detect the occurrence of pathology at the earliest stages, despite the natural reduction of organs. When the ovary is abnormally enlarged, the woman will be referred for consultation to an oncologist.
If the tumor is detected at the initial stage of development, it will be easier to treat it. Most oncologists are of the opinion that once a woman is diagnosed with menopause, any cyst or tumor on the ovary should be removed. The size of the tumor is not significant. This position is associated with a high risk of degeneration of a benign neoplasm into a malignant one against the background of prolonged low estrogen levels.
Ladies who have experienced menopause should understand that the cessation of menstrual function does not lead to the absence of problems in the reproductive system, but rather, on the contrary, requires increased attention to it. The work of the ovaries ceases with the onset of menopause, but they are susceptible to the development of pathologies and cancerous tumors.
Carrying out regular medical examinations will help to detect a tumor that has just appeared and prevent its growth until the last stage of the disease, when treatment does not always give a positive result. We wish you good health!
What do you know about changes in the ovaries during menopause?
When is it better to do an ultrasound of the ovaries in women and what will it show?
An important indicator of women's health is developed, normally functioning sex glands.
The ultrasound method helps to analyze their condition. Ultrasound of the ovaries in women allows us to identify deviations in their function, size and location, as well as detect possible neoplasms.
What is transvaginal ultrasound?
The most popular method for examining the pelvic organs is the transvaginal method . It is highly accurate because it is carried out through the thin vaginal wall.
Also, the positive side of the procedure is that the method is quite simple to carry out and can be used repeatedly without causing inconvenience to the patient.
The ultrasound machine sensor is a long rod about three centimeters in diameter. There is a channel inside the rod through which a needle is passed if a biopsy is necessary.
Transvaginal ultrasound can examine the uterus, ovaries, bladder and fallopian tubes. Due to its high accuracy, it provides objective information about the condition and pathology of these organs.
Indications for the procedure
For gynecological problems, a woman is prescribed an ultrasound of the ovaries to identify possible pathologies.
The most accurate data is obtained by multiple scans during one cycle at different stages : after menstruation, during ovulation, before menstruation, during menstruation. This helps to analyze the condition and functioning of the glands in each phase.
Many patients wonder whether it is possible to perform a transvaginal ultrasound during menstruation?
Doctors say that it is not only possible, but also necessary for a more accurate diagnosis.
With heavy menstruation in the first days, the patient may experience some awkwardness, so you can use this method on the third or fourth day after the start of menstruation .
Ultrasound of the ovaries is prescribed in the following cases:
- irregular menstrual cycle;
- pain in the lower abdomen;
- copious or scanty bleeding;
- painful menstruation;
- suspicion of inflammation;
- suspicion of a cyst or tumor;
- diagnosis of infertility;
- preparation for IVF;
- preventive examination.
The method is used to diagnose diseases such as:
- cyst;
- inflammation;
- ectopic pregnancy;
- accumulation of fluid in the fallopian tubes and pelvis;
- endometriosis;
- fibroids, teratoma;
- fibroma;
- polyps;
- cysts and tumors, their rupture (apoplexy);
- blister skid;
- chorionepithelioma.
Read our article about what an ovarian cyst is.
(The picture is clickable, click to enlarge)
(The picture is clickable, click to enlarge)
Timely diagnosis by ultrasound makes it possible to identify diseases and disorders of the ovaries in the early stages and begin treatment.
How to prepare?
No special preparation is required for ovarian ultrasound, which is a positive feature of the method.
The study is carried out on any day of the menstrual cycle, including during menstruation. However, for a planned one-time scan, it is recommended to choose the time from the fifth to the eighth day of the cycle . This helps assess the condition of the organs after menstruation, but before ovulation.
A distinctive feature of the transvaginal examination is that it is done on an empty bladder . The doctor asks the patient not to drink an hour before the procedure and to go to the toilet before it. If a woman suffers from increased gas formation, then she should take the appropriate drug several hours before the procedure.
How do they do it?
During a transvaginal ultrasound of the ovaries, the woman lies on her back on a special chair, bending her knees and spreading them apart.
https://www.youtube.com/watch?v=d1ZZQQc9cfE
This creates an optimal angle for scanning organs , and also facilitates the penetration of the sensor without causing discomfort.
The doctor places a condom on the rod-shaped sensor and lubricates it with gel. It is used to increase contact with the vaginal wall and eliminate discomfort during insertion. The sensor, or transducer, is carefully inserted into the vagina to a shallow depth. Based on the data displayed on the screen, the doctor makes a conclusion about the condition of the organs.
The duration of the procedure is no more than five minutes .
Decoding the results and how to calculate the volume?
When examining the ovaries, the doctor analyzes the data obtained. These include:
- dimensions;
- structure;
- location;
- the presence or absence of cysts and tumors.
On the screen picture, the ovaries are displayed as small, oval-shaped, tuberous formations. The tubercles are maturing follicles, their size depends on the day of the cycle : the further from its beginning, the larger the follicles.
The sizes of healthy ovaries, including those in nulliparous women, vary:
- length 20–37 mm;
- width 28–30 mm;
- thickness 14–22 mm;
- volume 4–10 cc.
To calculate the volume of an organ , the doctor uses a simple formula: size indicators (length, width, thickness) are multiplied among themselves and by a factor of 0.532.
In addition to the parameters of the glands themselves, the follicles are also important. Their number and normal sizes depend on the day of the cycle:
- 5–7 days. Up to seven small follicles (from two to six millimeters).
- 8–10 days. The dominant follicle grows up to fifteen millimeters, the rest up to ten.
- 11–14 days. The main follicle reaches two centimeters, ovulation begins.
- 15–18 days. The main follicle burst, and in its place was a yellow body up to two centimeters in diameter.
- Days 19–23. The corpus luteum grows up to 27 mm.
- 24–27 days. The corpus luteum decreases to one and a half centimeters.
Diagnostics on different days of the cycle allows you to track the process of follicle development, which helps to identify the disease, as well as find out the cause of infertility.
What else does the doctor see on an ultrasound?
There are frequent cases of pathology that are detected by ultrasound. Let's look at a few cases and explain what their reasons are .
Why is the ovary not visible, or the outline is unclear?
The fact that the ovary is not visualized on the monitor during examination indicates a congenital developmental pathology, adhesions, or premature depletion. However, do not be afraid to do additional research. Often, bloating makes it difficult to detect the gland.
A fuzzy outline occurs during the development of the corpus luteum, as well as with pathologies such as cysts and inflammation. The latter is also indicated by blurring the contour of the organ.
Ovarian enlargement
The size of the gland changes slightly during the cycle due to the growth of follicles. However, ovaries that are larger than normal are a reason to be wary. The reason for this phenomenon in inflammation of the organ may lie in the cyst.
If a pathology is suspected, an additional examination is carried out with a blood test to exclude the possibility of the woman’s anatomical features.
No follicles
The function of follicles is to form and develop eggs. The absence of follicles on one gland significantly reduces the possibility of conceiving a child, while bilateral damage reduces it to zero .
Increased echogenicity of the stroma
The stroma is the membrane of the ovary, penetrated by a large number of vessels. Its main function is to nourish maturing follicles. Normally, the stroma has average echogenicity. An increase in echogenicity (vessels are better visible) indicates inflammation of the organ or polycystic .
Multifollicular ovaries (see photo) - a sign characteristic of polycystic disease. With this disease, the ovary develops many follicles that do not mature. This complicates conception and leads to infertility.
(The picture is clickable, click to enlarge)
What does cancer look like?
When confirming the diagnosis of ovarian cancer, ultrasound reveals a large multilocular formation with thick walls. papillary growths develop on the tumor .
(The picture is clickable, click to enlarge)
Ovarian diseases seriously worsen a woman’s health and condition. Ultrasound examination of these organs, when carried out regularly, makes it possible to identify pathology at an early stage, which means timely initiation of treatment. The advantage of the method is its painlessness, accuracy and speed of diagnosis.
Find out how the whole process goes in the video:
Source: https://opochke.com/zhenskoe/kista-yaichnika/uzi-u-zhenshhin.html
Norms and reasons for changes in ovarian size during menopause
The ovaries are the most important components of the reproductive system of the female body. They are located on the sides of the uterine organ, at the same symmetry relative to each other. In the cavity of these organs, the processes of maturation of eggs occur, their release from the follicular membranes and subsequent movement along the fallopian tube, where the moment of its meeting with the sperm and fertilization occurs. Due to the fact that pathological changes in the functionality of the ovaries can lead to serious changes in the body’s fertility and general health, the normal size of the ovaries during menopause plays an important role, especially with ultrasound of the pelvic organs.
Normal ovarian sizes during the fertile period
The size of the ovaries in a young and healthy female body in the fertile period can change under the influence of hormonal levels and general health. Also, the sizes of both ovaries can differ up to several millimeters in normal conditions. A sharp and disproportionate growth of the ovaries is evidence of the development of any neoplasm of various etiologies or an inflammatory process.
Indications of the size of these organs depend on a certain number of reasons that tend to influence the reproductive glands of women at various stages in the menstrual cycle.
For the most accurate examination of the condition of the ovaries and the correct determination of their size, ultrasound research methods are carried out on days 5-7 of menstruation. The main indicator that you should pay attention to is not the width and length of the ovaries, but the volume of their cavity. Judging by them, the development of a tumor-like neoplasm, cystic lesion, inflammation, or whether this is a normal condition is established.
Normal indicators of ovarian volume are considered:
- volume readings from 4 and not more than 10 cm 3;
- lengths – 21-36 mm;
- width – 17-31mm;
- thickness – 16-23 mm.
The range in ovarian normal indicators is quite large, so the data obtained from an ultrasound examination of the reproductive system cannot be the only basis for making an accurate diagnosis. This requires other diagnostic methods.
Causes of changes occurring in the ovaries
Throughout the life of the female body, the ovaries tend to change slightly in size, which depends on:
- age indicators;
- number of births and abortions;
- day of menstruation;
- use of contraceptives containing hormonal substances;
- taking hormonal medications.
With the onset of puberty, the ovaries begin to become involved in the functioning of the woman’s reproductive system and subsequently, within normal limits, can change in size. During pregnancy, these organs, under the influence of increased blood flow necessary to ensure adequate nutrition of the fetus, increase in size. Moreover, with the increasing period of pregnancy, the ovaries can change their location, since the growing uterine organ with its dimensions displaces all nearby organs and tissues to a certain level. The size of the woman’s gonads increases by a couple of millimeters, and the previously occurring ovulation processes cease during pregnancy. Instead, the ovaries begin to produce progesterones, which play a critical role in normal gestation and an easy delivery process.
Pathological causes of changes in the gonads
When determining the possible development of a pathological process, it is necessary to take into account the indications of the norm of the ovaries in the fertile period. Evidence of the onset of development of a pathological change is the size of the ovaries doubling two or more times.
When determining the volume of the ovaries, pathology includes their increase by 1.5-2 mm 3.
When determining such indications during an ultrasound examination of the reproductive system of organs in the female body, this may be evidence of the development of the following pathological processes:
- Cystic lesions of the ovarian cavity with various etiologies and localizations.
- The development of polycystic disease, that is, multiple formation of tiny cysts.
- The appearance of benign neoplasms.
- The appearance of neoplasms with a malignant course.
- Development of metastases.
- Hereditary factor or congenital pathological development of the reproductive organs.
The reason for urgent surgical intervention may be pathologies such as purulent inflammation of the ovaries in menopause or their torsion. With such a course of dysfunction of the genital organs, if timely surgery is not performed, then everything can become complicated to the point of irreversible damage or death.
The most dangerous pathological change for a woman’s life is oncological processes.
- Cancer , localized in the organs of the reproductive system of the female body, ranks second among all causes leading to death, after cancer of the mammary glands. If an ultrasound specialist is able to discern the development of a cancerous tumor in the first stages of its development, then the woman has every chance to continue living, actively fighting against cancer. And sometimes even a full recovery is possible.
- The clinical picture will be much worse if the malignant neoplasm reaches an impressive size and causes symptoms of metastases. Therefore, a timely ultrasound examination will help to promptly identify the pathology and take the necessary measures to eliminate it.
A sharp decrease in the size of the ovaries during the fertile period is also dangerous. Such changes in the ovaries are generally called premature menopause, since a woman’s gonads simply fade away and cease to perform their functionality in the reproductive performance of the female body. Such a pathological change can occur from 36 to 40 years. Moreover, the uterine organ begins to shrink, and the uterine walls become thinner; not a single follicle is observed in the ovaries themselves. Under the influence of these atrophic processes, natural menstruation stops. After which, after a short period of time, menopausal symptoms may begin to develop in the female body:
- Increased sweating.
- Psycho-emotional state disorder.
- The appearance of insomnia.
- A sharp decrease or gain of extra pounds.
- Attacks of hot flashes and heat.
If these manifestations are diagnosed in a timely manner, then by taking hormone replacement therapy it will still be possible to restore reproductive functionality and safely conceive and give birth to a child.
In recent decades, hormonal drugs have been widely used for the treatment and prevention of gynecological diseases, as well as for contraception. More than 150 million people in the world take one or another hormonal drug every day, and adverse reactions occur in 30% of cases [7]. The body's reaction in individual women is expressed in a number of complications associated with changes in organs and systems and the formation of such syndromes as ovarian hyperinhibition syndrome, hyperinhibition of the hypothalamic-pituitary system, ovarian hyperstimulation syndrome, etc. [14]. In most cases, when using hormonal drugs, the generative function is preserved. However, pregnancy itself leads to significant hormonal and humoral changes, and it can be assumed that with a pathological reaction to hormones in the pregestational period, deviations from the “pregnancy norm” may occur [13].
During pregnancy, the cyclic processes associated with folliculogenesis and ovulation cease in the ovaries. From the 3-4th month of gestation, the corpus luteum of pregnancy undergoes regression, and its functions are performed by the placenta. The size of the ovaries during pregnancy corresponds to the pre-gestational size. The literature describes cases of an increase in ovarian size that persists up to 16 weeks of pregnancy, with stimulation of ovulation, multiple pregnancies (ovarian hyperstimulation syndrome, multifollicular ovaries (MFN), luteal ovarian cysts). A number of works provide information on the formation of theca lutein cysts (in the nomenclature of ICD-10 N83.2 - “theca lutein cysts” in the WHO histological classification, 2003 - multiple luteinized follicular cysts - hyperreactio luteinalis
) in any trimester of pregnancy due to increased serum levels of human chorionic gonadotropin in trophoblastic disease, non-immune hydrops fetalis, Rh isoimmunization, chronic renal failure. Isolated cases of symmetrically enlarged MFNs have been described in the first trimester of physiological pregnancy as a reaction to hormonal changes [2, 6, 8, 12, 17]. In the second half of pregnancy, cases of changes in the condition of the ovaries such as “ovarian hyperstimulation syndrome” have not been described.
The purpose of this study was to study the pathogenetic relationships in the placenta-ovarian system in pregnant women during the formation of MFN in late stages of gestation in order to optimize obstetric tactics for this pathology.
Material and research methods
The study was conducted on the basis of the maternity ward of City Clinical Hospital No. 2 named after. ON THE. Semashko, Samara, where in the period 2004-2008. 19,500 pregnant women gave birth, 4,000 of them by caesarean section. For an in-depth analysis, 2 clinical groups were formed: Group 1 (main) consisted of 48 women who had symmetrically enlarged ovaries due to multiple follicular cysts (MFC) in the second half of pregnancy and during cesarean section. Group 2 (control) included 30 healthy women who delivered abdominally and whose ovaries were without pathological changes. The groups were matched by age and parity. The main criterion for including pregnant women in the study was the normal size and structure of the ovaries in early pregnancy. According to ultrasound data at 12-13 weeks of gestation in pregnant women of the 1st and 2nd clinical groups, the ovaries, respectively, had the following characteristics: length - 30±3.5 and 32±4 mm (p>0.05); width - 18±4 and 19±3 mm (p>0.05); thickness - 17±2.5 and 18±3 mm (p>0.05); number of follicles - 1.3±0.7 and 1.4±0.8 (p>0.05).
Examination of pregnant women in the dynamics of gestation was carried out in accordance with the generally accepted management program: ultrasound, Doppler ultrasound (USD), cardiotocography (CTG), clinical and laboratory examination. In cases where MFN was detected by ultrasound and in the control group, an additional in-depth ultrasound assessment of the condition of the ovaries was carried out [4]. For each ovary, the following indicators were determined: volume, area, number of antral follicles with a diameter of 7-10 mm, average follicle diameter.
At the same time, ultrasound scanning of intraovarian blood flow was performed. To obtain a Doppler curve, loci were selected that were located in the thickness of the ovary, were not adjacent to the walls of the follicles, and were of the arterial type. In this case, the pulsatility index (PI), resistance index (RI), systolic-diastolic ratio (SDR), and time-averaged maximum blood flow velocity (MBV) were taken into account. Ultrasound scanning was performed using a transabdominal technique using a Philips Tangens device with color Doppler mapping.
The levels of hormones in the blood serum of pregnant women: human chorionic gonadotropin (hCG), estriol (E3), placental lactogen (PL) were determined by radioimmunoassay [15].
The study of the histological structure of the ovaries and placenta was carried out after staining serial sections with hematoxylin and eosin according to Van Gieson. Histological sections were studied by light-optical and telemetric methods using an SSD KOSOM KSS-310 RD video camera and a light microscope. The specific volumes of the structural elements of the placenta and the vascular index in the stem and terminal villi (SIst, SIt) were determined. The placental index was calculated as the ratio of the weight of the placenta to the weight of the newborn [10].
In the blood serum of pregnant women, the concentrations of placental growth factor (PPF), tumor necrosis factor alpha (TNFα), tumor marker CA-125, and histamine were determined using enzyme immunoassay methods, biochemical assays and reagent kits [3, 16].
All pregnant women had their medical history, ultrasound and laboratory data during gestation, intraoperative findings, and histological examination data analyzed. The obtained results were processed by the method of variation statistics using the Student's t test (probability 95%). Statistical data processing was carried out using the Statistica 6.0 application package.
Research results and discussion
From the anamnesis it was revealed that the average age of women in the 1st group was 27.5±1.5 years, in the 2nd group - 28±1.2 years (p>0.05). Menarche in women of the 1st group from 14.5±0.4 years, in the 2nd group - from 12.5±0.5 years (p<0.05). In 24 (50%) women of group 1, gynecological diseases were detected: 5 had uterine fibroids, 3 had endometriosis of the uterine body, 5 had chronic salpingoophoritis, and 11 had infertility of mixed origin. Polycystic ovary syndrome and diabetes mellitus were not observed in any woman. All women had a singleton pregnancy, there were no clinical and laboratory signs of isoserological incompatibility, non-immune hydrops and fetal development abnormalities. Indications for surgical delivery were placenta previa, anatomically narrow pelvis, breech presentation, placental insufficiency, transverse position of the fetus, and uterine scar. In pregnant women in the control group, indications for cesarean section were anatomically narrow pelvis, breech presentation, uterine scar, and abnormal fetal position. Among pregnant women of both groups 1 and 2, primiparous women predominated - 66.6 and 70%, respectively.
An intraoperative examination of the ovaries in women of the 1st clinical group revealed symmetrically enlarged 1.5-5 times pale pink ovaries with a smooth, shiny surface with an enhanced vascular pattern. The ovaries had a soft-elastic consistency with many diffusely located cysts, which was a deviation from the “norm” of late pregnancy.
In a physiologically proceeding pregnancy (2nd clinical group), intraoperatively the ovaries had the following characteristics: length - 29±4 mm, width - 17±3 mm, thickness - 19±3 mm, surface pale pink, smooth, shiny.
Clinical example No. 1. Pregnant M., 26 years old. Before pregnancy, for the purpose of contraception, she took combined oral contraceptives (COCs) for a year. After stopping taking COCs, the menstrual-ovarian cycle lengthened from 28 to 35 days, the duration of menstruation decreased from 5-6 days to 3 days, and the amount of blood lost also decreased. This is the first pregnancy that occurred spontaneously a year after stopping taking COCs. At 12 weeks of pregnancy and 22 weeks of pregnancy, an ultrasound was performed - without any features. An ultrasound scan at 34 weeks of pregnancy revealed symmetrically enlarged ovaries measuring 12×10×7 cm (right) and 14×11×7 cm (left). Serum concentration of CA-125 is 62 U/ml. She was delivered at 39 weeks by cesarean section due to placental insufficiency and chronic fetal hypoxia (Fig. 1).
Figure 1. Multifollicular ovaries in pregnant M., 26 years old, who took COCs before pregnancy. Macroscopic specimen (own observation): a - symmetrically enlarged ovaries with many diffusely located follicles, with an enhanced vascular pattern.
Figure 1. Multifollicular ovaries in pregnant M., 26 years old, who took COCs before pregnancy. Macroscopic specimen (own observation): b — left ovary (same picture).
Clinical example No. 2. Pregnant N., 25 years old. Before pregnancy I did not use hormonal drugs. Menarche at 14 years old. The menstrual-ovarian cycle is unremarkable. The first pregnancy occurred spontaneously. Ultrasound was performed at 12, 24, 28, 34, 39 weeks of gestation. Ultrasound at 24 weeks revealed for the first time symmetrically enlarged multifollicular ovaries measuring 12×9×6 cm (right) and 15×10×7 cm (left). During subsequent ultrasound examinations, the size of the ovaries remained virtually unchanged. The concentration of CA-125 in the blood serum during the dynamics of pregnancy ranged from 49-66 U/ml. The oncologist was consulted twice: surgical delivery with ovarian biopsy was recommended. Delivery was allowed at 39 weeks. The left ovary measuring 17×14×8 cm was removed intraoperatively (Fig. 2).
Figure 2. Multifollicular ovaries in pregnant N., 25 years old, who did not take hormonal drugs before pregnancy. Macroscopic specimen (own observation): a - symmetrically enlarged ovaries, pale pink in color, with a smooth shiny surface, many large follicles.
Figure 2. Multifollicular ovaries in pregnant N., 25 years old, who did not take hormonal drugs before pregnancy. Macroscopic specimen (own observation): b — left ovary on a section (same picture).
Histological examination of the biopsy material of the MFN taken from women of the 1st clinical group revealed multiple cysts lined with single- and multirow follicular epithelium, vascular congestion, edema and decidual reaction of the ovarian stroma. Moderate fibrosis of the capsule was detected during histological examination in isolated cases and in limited areas of the ovaries (Fig. 3).
Figure 3. Histological preparations of multifollicular ovarian tissue. a - multiple cysts lined with single- and multi-row follicular epithelium (hematoxylin and eosin staining), uv. 120.
Figure 3. Histological preparations of multifollicular ovarian tissue. b — multiple follicular cysts, decidual reaction of the ovarian stroma (hematoxylin and eosin staining), uv. 60.
Figure 3. Histological preparations of multifollicular ovarian tissue. c — fibrosis of the ovarian capsule, many diffusely located cysts lined with follicular epithelium, edema and decidual reaction of the stroma (Van Gieson staining), uv. 60.
The absence of macro- and microscopic signs of the presence of a significantly thickened capsule over the entire surface of the ovaries, the short existence of this pathological process (second half of pregnancy, the postpartum period), the absence of clinical and laboratory signs specific to polycystic ovary syndrome distinguishes, on the one hand, the described changes in the ovaries from the condition , characteristic of polycystic ovary syndrome, and the lack of luteinization of ovarian tissue distinguishes them, on the other hand, from luteinized ovaries (thecallutein cysts). The term MFN to denote the described pathology was chosen as optimally reflecting the essence of the changes - the presence of many follicular cysts clearly visible over the entire surface of the ovary, although in this clinical situation there is pronounced edema caused by increased stromal blood flow (due to the peculiarities of blood flow in the genital organs during pregnancy and the enhanced effect of vasotropic drugs). humoral factors of placental origin), as in ovarian hyperstimulation syndrome [4, 6, 8, 14].
Histological assessment of the placentas in all women of the 1st clinical group showed characteristic morphological signs of chronic placental insufficiency. According to the classification of A.P. Milovanova [9], 43 (89.6%) pregnant women had placental insufficiency of the 1st degree and 5 (10.4%) had placental insufficiency of the 2nd degree with moderate and well-expressed compensatory and adaptive reactions due to the growth of vessels in the terminal, intermediate, and stem villi and proliferative activity of syncytiotrophoblast: increased SIt, the number of syncytial nodules (Table 1).
Among the disorders of placental villous maturation, the dissociated variant predominated - 32 (66.6%) cases. In histological sections in this group of observations, along with mature ones, fields and groups of villi with signs of immaturity were identified. The terminal villi were large with loose and edematous stroma. A sufficient number of capillaries were noted in the terminal villi. However, there were signs of chorangiosis, characterized by a predominantly central and paracentral arrangement of capillaries and reduced formation of syncytiocapillary membranes. In the peripheral parts of the placenta, involutive-dystrophic changes were detected, including due to diffuse deposition of fibrinoid and calcifications. In 16 (33.4%) cases, placental angiomatosis was detected, which was characterized by a predominance of villi with a large number of fetal capillaries and syncytiocapillary membranes. In histological sections of the peripheral parts of the placenta, villous fields with symptoms of both chorangiosis and compensatory angiomatosis were observed (see Table 1).
A morphological study of placentas in the control group revealed villous maturity corresponding to the end of the third trimester of physiological pregnancy, a sufficiently large volume of intervillous space, well-vascularized terminal villi with a subepithelial arrangement of capillaries, a sufficient number of syncytiocapillary membranes and syncytial nodules. Moderately expressed involutive-dystrophic processes were more represented in the paracentral and marginal zones of the placenta and were expressed in the accumulation of fibrinoid in the stroma of the villi and intervillous space. The vascular index in the supporting and intermediate villi of the control group did not differ significantly from the corresponding indicator in the main group (p>0.05), while SIt (in the terminal villi) was significantly lower than in the main group (p<0.05), which evidenced the activation of angiogenesis in the main clinical group (see Table 1).
Consequently, a histological assessment of the placentas made it possible to identify the main morphological manifestations of placental insufficiency in group 1, characterized by dissociated and angiomatous variants of villous maturation, the phenomena of chorangiosis, compensatory angiomatosis and the proliferative activity of syncytiotrophoblast.
The placental index in the main group was 17.7±1.4%, in the control group - 17.2±1.2% (p>0.05), which indicated the absence of placental hypo- and hyperplasia in the examined groups [10, 13 ].
In the pregestational period, out of 48 women of the main group, 16 (33.3%) used COCs as contraceptives (from 6 months to 4 years, on average 1.5±0.5 years), 27 (56.3%) women received treatment hormonal drugs for gynecological or obstetric pathology - 15 women were treated with antigonadotropins, GnRH agonists, progestins and long-acting gestagens for fibroids, endometriosis, ovarian cysts against the background of chronic salpingoophoritis, infertility; 4 women took uromocriptine for hyperprolactinemia; 5 women underwent stimulation of ovulation with antiestrogens; 3 women received duphaston during pregnancy, 5 (10.4%) did not take hormonal drugs.
A study of the anamnesis in women of the 1st group made it possible to identify possible factors of increased risk of hyperergic (abnormal) ovarian reaction in late pregnancy: use of COCs; the presence of gynecological diseases (fibroids, endometriosis, ovarian cysts, chronic inflammatory diseases, infertility), in the treatment of which hormonal drugs were used; stimulation of ovulation; hormone therapy during pregnancy.
Over 5 years of observation, the prevalence of this pathology, according to our data, was 0.25% of all births; intraoperatively, such changes in the ovaries were detected in 1.2%, in the indicated risk groups - in 2.4%. Of the 48 cases of identified MFN, in 27 (56.2%) cases, pathological changes were diagnosed by ultrasound during pregnancy 22-36 weeks, in 21 (43.8%) cases during cesarean section.
In 27 women with MFN, in-depth ultrasound of the ovaries was performed to determine diagnostic criteria at 22-24 weeks and 34-36 weeks of pregnancy.
When analyzing the ultrasound characteristics, it was found that the average ovarian volume, number of follicles and ovarian area were significantly higher in women of the main group than in the control group (Table 2).
A comparative analysis of the indicators of blood flow velocity curves in the arteries of the ovarian stroma revealed a significant decrease in PI in the vessels of women of the main group compared to the control group, and a tendency to a decrease in PI was also noted (Table 3).
Analysis of ultrasound parameters (see Table 2 and Table 3) made it possible to identify threshold values characteristic of this pathological symptom complex: ovarian volume more than 12 cm3, area more than 6 cm2, number of cysts with a diameter of 7-10 mm more than 10, PI less than 1 ,0.
All patients of the 1st (main) group underwent ultrasound examination of the pelvic organs 5-7 days and 5-6 weeks after birth. During dynamic ultrasound monitoring of the condition of the ovaries in the postpartum period, a significant decrease in the volume, area and number of follicles was noted by the 5-7th day, PI increased and was more than 1.1. When examined 5-6 weeks after birth, ultrasound parameters corresponded to the physiological norm (Table 4).
To assess the hormonal influence on the formation of the identified changes in the ovaries, serum levels of hCG, E3, and PL were determined in women of the main and control groups at 22-26 weeks and 34-36 weeks of pregnancy (Table 5).
The results obtained for the content of hormones synthesized in the fetoplacental complex indicated the absence of a significant difference in the examined groups (p>0.05). The comparability of the values of hCG, E3 and PL parameters in the main and control groups can be explained by the severity of compensatory processes in the fetoplacental system during placental insufficiency and the leading role of hemocirculatory and vascular changes in its development. At the same time, a fairly high level of hormones of the fetoplacental complex in the 1st main group of pregnant women with placental insufficiency indicates the possibility of their participation in a complex effect on the ovaries.
It is reliably known that the vascular network of the placenta is formed by angiogenesis. This is a complex process that consists of several stages regulated by vascular endothelial growth factors, cytokines (TNFα, IL-1, IL-4, etc.), hormones, and biologically active substances (histamine). All stages of angiogenesis depend on the balance of proangiogenic and antiangiogenic factors. FRP, TNFα, histamine are angiogenic factors that potentiate the proliferation of endothelial cells and increase vascular permeability. The statement that hypoxia can stimulate angiogenesis supports the concept of accelerated placental maturation in various pathologies. In turn, increased dysfunction of the placenta (placental dysfunction) leads to changes in the content of angiogenic factors in the peripheral blood of pregnant women [3, 9, 11, 18, 19].
Over the past decade, a lot of data has begun to appear indicating the important role of vascular factors in the formation of ovarian hyperstimulation syndrome and the formation of MFN [11, 14].
This scientific information served as the basis for determining the concentrations of PRP, TNFα, and histamine in the peripheral blood of pregnant women at 22-24, 34-36 weeks. To exclude malignant degeneration, determination of the level of tumor marker CA-125 was used (Table 6).
The results of laboratory tests showed a significant difference between all indicators in the main group compared to the control group. An increase in the content of TNFα and histamine reflects the dynamics characteristic of pregnancy complicated by placental insufficiency, while the increase in the level of FRP, which is not entirely characteristic of this pathology, can be explained by the increased activity of angiogenesis and vascular endothelium in the placenta [9].
The CA-125 marker in the main group was 1.5-2 times higher than in the control group, but was within limits not typical for oncopathology [5]. By the end of the 1st week of the postpartum period, women in the main group showed positive dynamics in all indicators and their stabilization at the level of the control group by the 6th week after birth (see Table 6).
Based on the obtained clinical, morphological, laboratory and instrumental data, it can be assumed that there is a clinical syndrome of placental ovarian stimulation. It is hoped that subsequent scientific research will expand our understanding of the nature of the complex relationships in the placenta-ovary system as an integral part of the functional mother-placenta-fetus system.
conclusions
1. In late pregnancy, in 0.25% of cases, an abnormal reaction of the ovaries develops, morphologically expressed in stromal edema and polycystic disease, an increase in the size of the ovaries by 1.5-5 times, which is a deviation from the “pregnancy norm” and may be associated with the influence placental angiogenic and other factors.
2. In each case, the tactics for managing a pregnant woman with ovaries changed in late gestation according to the type of “hyperstimulation syndrome” should be determined individually, since the reason for choosing the method of delivery is not the ovarian formation with a characteristic ultrasound picture, but the obstetric situation. Indications for surgical delivery from the ovaries may be: sharply increased sizes (more than 15 cm) or possible complications from the ovaries (rupture, torsion). In the absence of complications, the ovaries are preserved, and a biopsy is performed if necessary. A biopsy must be performed if there is no certainty that the changes are benign.
3. In the postpartum period, dynamic ultrasound monitoring of the condition of the ovaries is necessary.
4. Women with this abnormal ovarian reaction during pregnancy should be considered at risk for developing disorders in the reproductive system. Hormonal contraception is not indicated for them; if possible, treatment with hormonal drugs should be excluded. These women are likely to develop syndromes of hyperinhibition of the hypothalamic-pituitary-ovarian system, resistant ovaries, hyperstimulation and premature ovarian failure.
Ovarian changes during menopause
Atrophic changes characteristic of the female body during the menopausal period also apply to these organs of the reproductive system.
The size of the ovaries decreases during menopause. Their structure also undergoes changes, during which hormone-secreting tissues begin to be replaced by connective tissues. The number of follicles is reduced, until they disappear completely.
The development of a functional cyst in menopause should not occur. All neoplasms that arise at this age are already referred to as tumors.
Taking into account the fact that after the age of 55, the likelihood of developing cancer in women increases several times, medical specialists should pay special attention to the state of a woman’s health during diagnostic testing during the menopausal period, especially her mammary glands and reproductive system.
Every woman, in turn, should not forget that the absence of a menstrual cycle does not mean that there cannot be problems with gynecological health.
Regular visits to the gynecological office (at least once every six months) will help eliminate the likelihood of developing many serious pathologies, even preventing the development of oncology to a stage that is no longer amenable to any treatment method.
Any cystic ovarian lesion in menopause should be treated with surgery to prevent complications.
Symptoms of pathological changes in the ovaries
The most insidious thing about the development of tumors in menopausal women is that they do not cause any clinical manifestations. And only sometimes (no more than 30%) can they make themselves felt with blurred manifestations, relating equally to neoplasms of both a malignant and benign nature.
In most cases, among those representatives of the fairer sex who ignore the need for regular examination by specialists, such diseases are detected only in the event of complications characterized by torsion or rupture of the ovary, or acute pain symptoms in the lower abdomen. Also, the increasing manifestation of ascites and symptoms of compression near located organs indicates the development of metastases against the background of the main pathological process.