How to measure the uterus during pregnancy
In the first three months, the small size of the uterus allows an assessment to be made based on vaginal palpation, which will provide information to the doctor about the formation of the baby.
Over time, the baby inside the womb forms faster; at 12-14 weeks, the first ultrasound is scheduled, where specialists take measurements and look at the length of the cervix. And from this same period, when the reproductive organ leaves the pelvic area, it is possible to measure the fundus height (FHR). As soon as the uterus has increased in size and is located in the abdominal cavity, the gynecologist begins dynamic monitoring of the growth of the abdomen. At each visit, the woman assumes a horizontal body position, and the doctor measures the abdomen with a centimeter from the pubic bone to the bottom. Each measurement is entered into a special table, which will allow you to see the child’s condition over time.
In the first weeks of gestation, body size remains virtually unchanged. Only an ultrasound examination will be the most informative during this period, and pregnancy is determined using tests and the appearance of the genital organs.
Table of uterine sizes by week of pregnancy
| Period (weeks) | VDM (cm) |
| 8-9 | 7-9 |
| 10-13 | 9-12 |
| 14-16 | 13-16 |
| 17-19 | 15-20 |
| 20-23 | 19-24 |
| 24-27 | 23-28 |
| 29-31 | 29-32 |
| 32-35 | 31-33 |
| 36-38 | 32-38 |
| 39-41 | 37-40 |
| 36-38 | 32-38 |
| 39-41 | 37-40 |
Normal cervical size during pregnancy
The cervix consists of a supravaginal part and a vaginal part, which can be seen during examination on a gynecological chair. The inner part is closed by a muscle ring and a mucous plug, which protects the baby from the penetration of harmful bacteria and keeps the fetus inside the womb until labor begins. By week 37, when the baby is fully formed, the cervical canal softens and begins to open, the body prepares for the birth of a new life.
Normal cervical sizes are determined depending on the stage of gestation:
- from 16 to 20 – 40-45 mm;
- from 25 to 28 – 35-40 mm;
- from 32 to 36 – 30-35 mm.
The normal cervical length is a very important diagnostic indicator, since this parameter, if it is significantly less, allows you to prevent miscarriage and preserve intrauterine development. The size of the uterus during twin pregnancy allows us to assess the internal os. Because the pressure in this case increases significantly and contributes to premature opening.
Brown and bloody discharge during pregnancy
During pregnancy, brown (blood-colored) discharge and bloody discharge from the genital tract at any stage cannot be considered normal. This color of discharge is an “alarm bell” through which the body reports that “problems” have arisen.
Causes of brown and bloody discharge during pregnancy:
1. The main reason for brown discharge (especially in the first trimester) is the threat of spontaneous miscarriage:
- If the discharge is insignificant, slightly colored and appears once, then most likely there is nothing to worry about. Perhaps their cause was a single episode of hypertonicity associated with overwork or nervous stress.
- Abundant dark brown discharge from the genital tract, accompanied by nagging pain in the lower abdomen, indicates detachment of the fertilized egg. Moreover, the intensity of discharge of this color is directly proportional to the size of the detachment area. The appearance of bloody discharge indicates a worsening situation and, possibly, a miscarriage.
2. Ectopic pregnancy, as well as the risk of miscarriage and premature birth in the second and third trimesters.
3. In the later stages: premature placental abruption or placenta previa. In both cases, bleeding is usually profuse and is accompanied by hypertonicity of the uterus, as well as pain in the back or abdomen, depending on the location of the detachment site itself. In addition, the expectant mother may feel dizzy due to a decrease in hemoglobin due to excessive bleeding.
Regardless of the reason for the appearance of bloody discharge, in all of the above cases, you must immediately consult a doctor in order to select adequate therapy or timely hospitalization.
Discharge during pregnancy can be both normal and a reason to visit a doctor
Pay attention to their color, smell and abundance. Tell your doctor if you have any associated pain in your back or lower abdomen
Odorless mucous discharge is completely natural, but if the discharge is white/yellow/brown/bloody, treatment may be required. Attentive attitude to your body and the ability to recognize the first “alarm bells” will allow you to avoid the “unpleasant moments” of pregnancy and successfully reach the “finish line” - childbirth.
Why does the uterus not match the gestational age?
The discrepancy between the parameters of the womb and the gestation period occurs for various reasons. Basically, the situation is associated with the presence of infectious diseases, pathological disorders or placental insufficiency. With hypoxia, impaired blood coagulation parameters or limited supply of nutrients, the fetus may freeze and die; in this case, the parameters will be less than the term.
The reasons when the size of the uterus is longer than the term most often indicate the formation of more than one fetus or the development of a large baby, polyhydramnios. When making a diagnosis, doctors must conduct appropriate tests and procedures to eliminate disruptions in the endocrine system.
If the size of the uterus does not correspond to the period after 28 weeks, this may indicate an initially incorrect calculation of the period of conception or minor deviations. Therefore, it is necessary to normalize the psychological state of the pregnant woman with the help of natural sedatives, so as not to aggravate the pathology.
Any pronounced deviation from the norm becomes the reason for additional ultrasound studies, where the state of the amniotic fluid is determined and development indicators inside the womb are compared. They also consult with a geneticist, who will determine what will be normal in each individual case.
From the moment of conception until birth, the size of the fetus gradually increases. The growth of the uterus observed during the weeks of pregnancy is a normal physiological process. Based on the dynamics of this indicator, an experienced gynecologist monitors the changes in the mother’s condition and the development of the embryo, can promptly notice any complications or pathologies that have arisen and take measures to eliminate them. Measurements are taken and recorded by a doctor during regularly scheduled examinations; from the second trimester, a woman can perform them independently, at home.
If your belly size is not normal...
The rate of enlargement of the uterus, and therefore the growth of the abdomen, must quite strictly correspond to the above parameters, since they are an important indicator of the normal course of pregnancy.
In the early stages, when the uterus is not yet palpable through the anterior abdominal wall, the discrepancy between its size and the expected duration of pregnancy may be a sign of an ectopic pregnancy, while the fertilized egg most often develops in the fallopian tube.
Exceeding the expected size of pregnancy is characteristic of such a pathology as chorionepithelioma - a tumor that develops from placental tissue and represents a large number of small bubbles. With this tumor, the fetus dies, and timely treatment is necessary to preserve the health of the mother.
In later stages of pregnancy, a lag in the rate of increase in the uterine fundus most often occurs with fetal malnutrition, that is, with a delay in its growth. With this pathology, the baby is born even with timely birth with a weight of less than 2600 g, and its adaptation to extrauterine life is difficult.
Oligohydramnios in pregnant women can also cause the uterus to be smaller than expected. Among the possible causes of this complication are maternal hypertension, infectious and inflammatory diseases, inflammatory diseases of the female genital area, damage to the fetal excretory system, placental insufficiency, gestosis - a serious complication of pregnancy in which generalized vasospasm is observed; it is usually manifested by edema, increased blood pressure, and the appearance of protein in the urine.
A decrease in the height of the uterine fundus is possible with a transverse position of the fetus, when the baby in the uterus is positioned so that the head and pelvic end are on the sides. If the fetus is in a transverse position, delivery through the natural birth canal is impossible.
The size of the uterus is larger than the expected gestational age also occurs with multiple pregnancies. As you know, multiple pregnancy is a high-risk pregnancy: it increases the likelihood of various complications.
Will stretch marks appear during pregnancy? The skin on the abdomen stretches as pregnancy progresses. Will this process pass without a trace? It must be said that skin damage - so-called stretch marks - as a result of an increase in the volume of the uterus depends, of course, on the rate of growth of the abdomen, but for the most part their appearance is determined by the characteristics of the skin of the expectant mother. Of course, the likelihood of stretch marks slightly increases if the fetus is large, quickly gains weight, or if there is polyhydramnios, but the condition of the collagen and elastin fibers is decisive. To prevent stretch marks (striae), especially during intensive abdominal growth - in the third trimester of pregnancy - you can use products that improve skin condition. This is a special cosmetics for pregnant women, containing vitamins A, E, as well as substances that improve blood circulation in the skin. Since skin often becomes drier during pregnancy, you can also use moisturizing creams for pregnant women; they will also help prevent stretch marks. You can also prevent the appearance of stretch marks with the help of massage, which improves blood circulation in the skin. The technique of this massage is not complicated: you should stroke the stomach in a circular motion, pinching the skin along the periphery of the abdomen. If there is a threat of miscarriage, such a massage should not be performed, as it can provoke an increase in the tone of the uterus.
The uterus can enlarge with significant polyhydramnios - a condition when the amount of amniotic fluid exceeds the norm, reaching 2-5 liters, and sometimes 10-12. This pathology occurs in diabetes mellitus - impaired absorption of sugar, Rh-conflict pregnancy - when the body of a Rh-negative mother produces antibodies against Rh-positive erythrocytes of the fetus, in acute and chronic infections, and in fetal developmental anomalies. Of course, all these conditions require close attention from doctors.
The uterus may grow faster than usual if the fetus is large. In turn, a large fetus may be a consequence of both genetic characteristics and diabetes in the expectant mother during this pregnancy. A large fetus increases the risk of complications during childbirth, and diabetes requires treatment.
Thus, changes in the rate of increase in the height of the uterine fundus can serve as an indicator of various pathologies of the mother and, more often, the fetus. Therefore, if at the next appointment the doctor discovers that the height of the uterine fundus does not correspond to the gestational age, he prescribes additional studies to clarify the factors that caused the decrease or increase in the rate of abdominal growth.
What is the size of the uterus by week of pregnancy
The dimensions of the uterus in nulliparous women average from 4.5 to 7 cm in length and from 4.5 to 6.5 cm in width, thickness - 3.5-4 cm. Individual parameters may deviate from the physiological norm by 2-3 see. After pregnancy and implantation of the embryo, the organ begins to enlarge (under the influence of fetal growth), continuing until the last prenatal weeks. By birth, the size of the uterus reaches 33-40 cm.
By changing the location of the uterus and its growth parameters, an experienced specialist can determine the duration of pregnancy, the nuances of its course, and the characteristics of fetal development. To track the dynamics of organ enlargement, at each scheduled examination, the gynecologist takes measurements of the volume of the abdomen and the width of the pelvis. With the beginning of the second trimester, the indicator of the height of the uterine fundus (VSD or VDM) is introduced.
What is the uterus and where is it located?
The uterus is an organ of a woman’s reproductive system in which the fetus develops from the moment the fertilized egg leaves the fallopian tube until the child is born. Its shape resembles an inverted pear.
The uterus is located in the pelvis between the bladder and rectum. Its position can change during the day: when the organs of the urinary and digestive systems are filled, it moves slightly, and after urination or defecation it returns to its original place. But the most noticeable change in the position of the uterus is observed simultaneously with its growth during pregnancy, as well as after childbirth.
Features of changes in the uterus during pregnancy
The process of organ enlargement occurs gradually, measuredly, and therefore does not normally cause the woman any discomfort. Nagging pain and other unpleasant symptoms occur against the background of sprained ligaments or the formation of adhesions during polyhydramnios, multiple pregnancies, or due to scars after previous surgical operations. The size of the uterus depends on the trimester and changes as follows:
- First trimester. The uterus is located behind the pelvic bone and is shaped like a pear. In the sixth week, the size of the organ reaches the volume of a chicken egg, in the eighth - that of a goose egg. By the end of the trimester, the uterus takes on a round shape and increases three times its original size.
- Second trimester. The organ is centered in the pelvic region, acquires symmetry, and begins to be palpated through the abdominal wall as it emerges from behind the pubic bone.
- Third trimester. The organ again takes on the shape of an egg, stretching towards the bottom. The uterine cavity increases 500 times compared to the beginning of pregnancy, the weight of the organ changes on average from 50 g to a kilogram (muscle fibers lengthen, thicken, and the vascular network develops).
The height of the uterine fundus increases week by week in each trimester in parallel with the development of the fetus. It goes through the following main stages:
- 8-9 weeks of obstetric period - the average volume of the organ corresponds to a goose egg, it cannot be felt through the abdominal wall.
- 10-13 – the organ rises above the pubic bone; The activity of the functions of the placental system increases, the corpus luteum gradually disappears. The fetus develops its vascular system and begins to make its first movements. VDM - about 11 cm.
- 14-16 – completion of the formation of the internal organs of the embryo. The uterus reaches a size of 14-15 cm. At week 16, the position of the fundus height reaches the middle between the navel and the top of the pubic bone.
- 17-19 – the fetus develops its immune system, limbs, and cerebellum. The organ increases in size to 19-20 cm.
- Week 20 and beyond - the gap between the fundus of the uterus and the pubis reaches 21 cm, then this figure increases by an average of 1 cm per week. The VDM is located approximately two fingers' length below the navel.
- 23-24 – the weight of the fetus reaches 0.6 kg or more, its muscles and bones develop, and the respiratory system is formed. VDM – 24 cm.
- 28 – VDM is about 28 cm, located 2-3 cm above the navel.
- 29-30 – the size of the organ reaches 31-32 cm.
- 32 – the uterus is located in the center between the navel and the xiphoid process of the sternum, the IMD is about 34 cm.
- 38 – gradual descent of the organ begins, accompanied by strong pressure on the diaphragm and stomach.
- 40 – the size of the uterus ranges from 32-34 to 40 cm, depending on the physiological characteristics of the mother’s body, the size of the fetus, and a number of other factors.
What is an organ
The uterus is the most important female organ, without which girls would not have the function of childbearing.
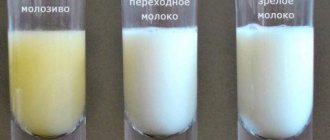
During pregnancy, it increases several times (can increase several dozen times), and after childbirth takes place, it takes on the same size as it was before the woman conceived and carried the fetus. The uterine walls have three layers, each of which is needed for a reason. The first layer, the endometrium, leaves the uterus along with the blood when menstruation occurs and when a woman becomes pregnant, the endometrium allows the fetus not to starve in the early and later stages.
The second layer of myometrium is muscle. It is thanks to this layer that the uterus grows and decreases in size. In the early stages, in the first 4 or 5 months of pregnancy, the myometrial muscle fibers lengthen up to 11 times and thicken approximately 6 times. When the fetus is about 5 months old, their thickness reaches 4 centimeters. After twenty weeks of pregnancy, the uterus grows in volume, stretches, and the walls become thinner. In the last week, the walls can be only half a centimeter thick, and the uppermost layer, the perimeter, is almost invisible.
We will tell you how the uterus develops during pregnancy (data indicating normal development). When a woman is pregnant, not only does the size of the uterus change, but its density and shape also change.
In the early stages (about 5 weeks), the uterus begins to slowly enlarge. At first it looks like a ball, and then grows in transverse dimensions. In the early stages of pregnancy, the uterus often turns out to be asymmetrical; one of the corners of the organ may protrude, but soon the entire free volume will be filled by the growing fetus, and the protrusion will go away.
The increase occurs especially quickly at 3 months. By the end of the third month, the size may differ from the original by four times! In the second trimester, a woman’s uterus “comes out” of the small pelvis, and can now be checked by touch. From this time on, the gynecologist takes another measurement - the height of the uterine fundus (it rises) and the volume of the abdomen. Before taking measurements, you need to go to the toilet.
Normal fundal height indicators during different periods of pregnancy should be as follows:
- 16 weeks – about 7 centimeters,
- 20 weeks – 13 centimeters,
- 24 weeks – up to 28 centimeters,
- 32 weeks – from 28 to 30 centimeters,
- 36 weeks - up to 34 centimeters, at this time the bottom is located approximately at the urinary process,
- by the fortieth week (by the time you are supposed to give birth), the uterus, on the contrary, begins to drop to 28 centimeters.
The height of the uterine fundus (UFH) does not form independently; it rises depending on the size and weight of the fetus, its location in the organ, and the amount of fluid that is near the fetus.
Uterus size chart by week
Indicators of the height of the fundus and the size of the uterus are physiological, therefore deviations from the fixed norms within 2-3 cm in most cases arise due to the characteristics of the mother’s body and the individual nuances of the course of pregnancy. The dynamics of changes in the size and position of the organ in accordance with different periods are presented in the table:
Based on the dynamic development of the uterus and the height of its fundus, the doctor assesses the successful course of pregnancy. How to correctly measure the changing size of an organ? What deviations affect the increase? What to do if there is a threat of miscarriage?
The uterus of a nulliparous woman has very modest dimensions: 5.0 – 6.0 cm in length; 3.4 – 4, 0 – in width. Its weight is about 50 grams. Over 9 months of gestation, the organ undergoes enormous changes, increasing in size, thinning, reaching a weight of up to 4 kg along with the fetus. This transformation, recorded weekly in a special table of indicators, constitutes the dynamic course of pregnancy.
How is the condition of the uterus assessed?
If in the first trimester of pregnancy the condition of the uterus is assessed during a bimanual examination, then from about the fourth month, to assess the progression of pregnancy and the condition of the uterus, the obstetrician-gynecologist uses four external obstetric examination techniques (Leopold's techniques):
- During the first external obstetric examination, the doctor places the palms of both hands on the uppermost part of the uterus (fundus), and the UMR is determined, the correspondence of this indicator to the gestational age and the part of the fetus located in the fundus of the uterus. it is performed by alternately palpating parts of the fetus with the right and left hands. When the fetus is positioned longitudinally, the back is palpated on one side and small parts of the fetus (arms and legs) on the other. The back is palpated in the form of a uniform area, small parts - in the form of small protrusions that can change their position. The second technique allows you to determine the tone of the uterus and its excitability (contraction of the uterus in response to palpation), as well as the position of the fetus. In the first position, the fetal back is turned to the left, in the second - to the right.
At the third appointment, the obstetrician-gynecologist determines the presenting part of the fetus - this is the part of the fetus that faces the entrance to the pelvis and is the first to pass through the birth canal (usually the fetal head). The doctor stands on the right, facing the pregnant woman. With one hand (usually the right) palpation is carried out slightly above the symphysis pubis, so that the thumb is on one side, and the other four are on the other side of the lower part of the uterus. The head is palpated in the form of a dense round part with clear contours, the pelvic end is felt in the form of a voluminous softish part that does not have a round shape. When the fetus is in a transverse or oblique position, the presenting part is not determined. At the fourth appointment, palpation (feeling) of the uterus is carried out with both hands, and the doctor stands facing the pregnant woman’s feet. The palms of both hands are placed on the lower segment of the uterus on the right and left, with outstretched fingers carefully palpating the height of its standing and the presenting part of the fetus. This technique allows you to determine the location of the presenting part of the fetus relative to the entrance to the mother’s pelvis (the presenting part is above the entrance to the small pelvis, pressed against the entrance, descended into the pelvic cavity). If the head is present, the obstetrician determines its size, the density of its bones and its gradual descent into the pelvis during childbirth.
All techniques are carried out very carefully and carefully, since sudden movements can cause reflex tension in the muscles of the anterior abdominal wall and increase the tone of the uterus.
During an external obstetric examination, the doctor assesses the tone of the uterine muscles. Normally, the wall of the uterus should be soft, but with the tone of the uterus during pregnancy it becomes hard. Increased tone (hypertonicity) of the uterus is one of the signs of a threatened miscarriage; it can occur at any stage, and the woman usually feels pain in the lower abdomen and lower back. The pain can be minor, nagging or very severe. The severity of the pain symptom depends on the threshold of pain sensitivity, duration and intensity of uterine hypertonicity. If the increased tone of the uterus occurs for a short time, then the pain or feeling of heaviness in the lower abdomen is most often insignificant. With prolonged hypertonicity of the uterine muscles, the pain symptom is usually more pronounced.
Content
- Measurements using Leopold's method
- Fundal height of the uterus in early stages
- When can an organ be measured?
- Parameters of the uterus during pregnancy
- Uterine wall thickness
- Location
- Dimensions for anatomical defects
- Gradual changes in the uterus during pregnancy
- Uterus sizes by week
- When can you feel the uterus yourself?
- Neck sizes in table
- Normal sizes of the uterus by week of pregnancy in the table
- What can affect the height of the uterine fundus?
- Changes in the uterus during multiple pregnancy
- Techniques to support a thin uterus or an exhausted cervix when there is a threat of premature birth
- Why the size of the uterus does not correspond to the term
Pain in the uterus at the beginning of pregnancy: why the uterus hurts in the early stages
In early pregnancy, women often experience pain in the uterus. This symptom can have several possible causes, and although most of them do not indicate serious health problems, in some cases women need medical attention.
At the very beginning of pregnancy, the uterus is significantly smaller in size compared to the second and third trimesters. Therefore, pain in this part of the body is usually not associated with the pressure that an enlarged uterus puts on other organs.
In addition, women during this period do not yet have time to gain weight, which means that it also cannot be the cause of discomfort.
However, uterine pain is one of the most common symptoms of early pregnancy. In this current article, we will look at potential causes of this pain, which include adjustments in hormonal levels and changes in muscles.
Uterine round ligament pain
The source of pain in the lower abdomen may be the round ligaments of the uterus
Pain in the round ligaments of the uterus occurs because the uterus enlarges and the ligaments that support it stretch to accommodate the developing fetus. This pain usually occurs in sharp, stabbing attacks on one or both sides of the uterus. The attacks can be sudden and last only a few seconds.
Pain in the round ligaments of the uterus occurs without warning. Some women experience particular discomfort when changing body position in bed. Additionally, the problem may occur when a pregnant woman gets out of a chair or bed.
Pain in the round ligaments of the uterus can cause some discomfort, but it does not indicate the development of serious health problems.
Pelvic floor muscle pain
Many women experience pain in the pelvic floor muscles while bearing children. This symptom can occur in the early stages of pregnancy, especially in those women who have already given birth to children. A stretched uterus is one cause of this pain, although hormonal changes can also affect the pelvic floor muscles.
Pain in the pelvic floor muscles manifests itself in different ways. Women can feel it in the area of the uterus itself, as well as in the area of the bladder, vagina, back or abdomen.
This type of pain does not indicate problems with the developing fetus, but it should be understood that it may get worse as the pregnancy progresses.
Spasms
Early pregnancy is often accompanied by cramps similar to those that occur during menstruation. This symptom may develop against the background of increased progesterone levels or an enlarged uterus.
Some women worry that cramping may be a sign of miscarriage. Intense cramps that get steadily worse can indeed indicate pregnancy loss, especially when they are accompanied by bleeding. However, in many cases, cramping is only a temporary symptom and is not an indicator of any problems.
Why determine the height of the uterine fundus during pregnancy?
The female uterus is a unique organ that can stretch during pregnancy and return to its original size after childbirth. The uterus consists of a larger part (body) located above and a smaller part (cervix) located below. The isthmus connects the body and the cervix. The fundus of the uterus is the highest part of the body of this organ.
The wall of the uterus consists of the following layers:
- internal (endometrium),
- middle (myometrium),
- external (perimetry).
The myometrium, or muscular lining, makes up the bulk of the uterine wall. It is due to changes in the myometrium that the size of the uterus increases during pregnancy.
By mid-pregnancy, the walls of the uterus thicken to 3-4 cm, due to the division of myometrial muscle cells. Then the size of the uterus increases only due to stretching and thinning of its walls.
In the last weeks of pregnancy, the thickness of the uterine walls is 0.5-1 cm.
In a woman of reproductive age outside of pregnancy, the length of the uterus is 7-8 cm. By the end of pregnancy, the uterus reaches a length of 37-38 cm. Moreover, in the case of multiple pregnancy, polyhydramnios, it can reach even larger sizes.
In the second trimester of pregnancy (13-14 weeks), a woman’s uterus extends beyond the pelvis. At this stage, the obstetrician-gynecologist can already palpate it through the anterior abdominal wall. It is at this time that the doctor begins to measure the height of the uterine fundus during pregnancy (UFH).
Method for measuring the uterus during pregnancy
The measurement is carried out using the “Leopold technique” - a special obstetric technique.
- The measurement is carried out with an empty bladder.
- The woman lies on her back on the couch.
- Raising your hand from the pubic area along the midline of the abdomen, you feel the area where the dense tissue becomes soft and loose - this is the border of the uterus, called the bottom.
- Using a soft ruler, measure the distance from the pubic bone to the bottom.
With physiologically correct development, the distance in centimeters coincides with the period established in weeks. Possible error: 1 – 2 cm. This calculation is applicable up to 37 – 38 weeks. Later, the uterus settles into the pelvic cavity in preparation for childbirth.
Is it possible to take measurements at an early stage?
In the first weeks, pregnancy manifests itself only with slight tension - an increase in the tone of the uterus. Its walls soften, which promotes stretching and increase in mass. But the organ is located within normal boundaries, so it is impossible to measure its size using the described method.
From when can measurements be taken?
No visual changes are observed until 6 weeks. The fact of conception is established using hCG analysis and a urine test. Monitoring the correct formation of the placenta and embryo is carried out by ultrasound examination.
Only from the 12th week the uterus extends beyond the symphysis pubis and can be felt in the lower abdomen. From this point on, weekly growth measurements are taken and development dynamics are monitored.
What is considered normal?
Pregnancy is characterized by an increase in the size of the uterus, a change in its consistency (density), and shape.
Enlargement of the uterus begins at 5-6 weeks of pregnancy (with 1-2 weeks of delay), while the body of the uterus increases slightly. First, the uterus increases in anteroposterior size and becomes spherical, and then the transverse size also increases. The longer the pregnancy, the more noticeable the enlargement of the uterus becomes. In the early stages of pregnancy, asymmetry of the uterus often occurs; during bimanual examination, a protrusion of one of the corners of the uterus is palpated. Protrusion occurs due to the growth of the fertilized egg; as pregnancy progresses, the fertilized egg fills the entire uterine cavity and the asymmetry of the uterus disappears. By 8 weeks of pregnancy, the body of the uterus increases approximately 2 times, by 10 weeks - 3 times. By 12 weeks, the uterus enlarges 4 times and the fundus of the uterus reaches the plane of exit from the small pelvis, i.e., the upper edge of the symphysis pubis.
From the second trimester of pregnancy (from the 13-14th week of pregnancy), the uterus extends beyond the pelvis and can be palpated through the anterior abdominal wall. Therefore, starting from this period, the obstetrician-gynecologist measures the height of the uterine fundus (VDM - the distance between the upper edge of the symphysis pubis and the highest point of the uterus) and abdominal circumference. All measurements are recorded in the pregnant woman’s individual chart, which allows us to track the dynamics of uterine growth and estimate the growth rate. VMR is measured with a centimeter tape or a pelvisometer (a special device for measuring the distance between two points) with the pregnant woman lying on her back. Before measuring and examining, you must empty your bladder.
The normal (physiological) course of pregnancy is characterized by the following indicators of AMR:
- at 16 weeks of pregnancy, the fundus of the uterus is located in the middle of the distance between the navel and the pubic symphysis, the IMD is 6-7 cm; are based only on the size of the uterus. Other indicators are also taken into account, such as the date of the last menstruation, the date of the first fetal movement, and the results of an ultrasound examination.
Parameters of the uterus during gestation
Fetal growth causes changes in several directions. They all have a role in controlling proper development.
Myometrial thickness
The uterus is a muscular organ. Conception stimulates active growth of myocytes. During the first half of gestation, the wall of the organ thickens 3–4 times; further increase, in the second half of gestation, occurs due to stretching of the muscle fibers. Around the middle of the term, the thickness of the wall is 3.5 - 4 cm. By the end of the third trimester, during the period of intensive growth of the child, the wall thins to 1 - 0.5 cm.
The volume of the organ increases 400 times at the time of delivery. In multiple pregnancies, these indicators are even higher, and the thinning of the wall is stronger.
Location in the cavity
In thin ladies, a noticeable increase in the abdomen can be observed as early as 6 weeks of pregnancy. First, changes occur in the anteroposterior direction, and the uterus takes on the shape of a ball. Later, transverse growth begins. By 8 weeks, the volume of the organ doubles, and by 10 weeks, it triples.
In the early period, the fertilized egg is located in one of the halves of the uterus, which causes visual asymmetry of the abdomen. As it develops, the embryo fills the entire cavity, and the abdomen becomes uniform. It matters in which part the embryo is attached. If its introduction occurred on the posterior wall of the cavity, the abdomen is hardly noticeable, but if on the anterior wall, a round protrusion is visible in the early stages.
Changes in pathological features
The location of the uterus and its parameters change depending on the anatomical features of the organ. In pre-pregnancy life, a woman may not be aware of any abnormalities. But during the development of the embryo, an anatomically abnormal uterus can become a threat to pregnancy.
Attention! These features do not affect a woman’s daily life in any way, but pose a threat during pregnancy.
Briefly about the structure of the uterus
To understand how the uterus changes in the early stages of pregnancy, you should know what it is like before it. This organ has the shape of a pear and includes the neck, isthmus and body. The layer that holds the fertilized egg is called the endometrium. In many ways, it ensures that the embryo remains inside, especially at first.
The structure of the uterus and the passage of the egg through the monthly cycle
By the time of implantation, the upper section of the mucosa should be quite loose and thick. In addition to the endometrium, two more layers are distinguished: the myometrium (muscle base) and the perimeter (the outer part of the uterus). Their integrity and adequate functioning are also necessary for a healthy pregnancy. The parameters of the uterus before its onset have the following values:
- length 7 cm;
- transverse size 4 cm;
- thickness 4-5 cm.
In women who already have a child, the size is slightly larger, and the weight of the organ is 20-30 g higher.
Appearance
Many women would like to know what the uterus looks like in early pregnancy. For a specialist, the appearance of an organ can be one of the signs of the condition. And although upon examination only a part of it called the cervix is visible, and not entirely, but partially, the changes occurring with it will clearly indicate the presence of a new organism in the uterus. Usually the pink shell is made bluish in color. The sign is caused by the flow of a significant volume of blood into this area, as well as the dilation of blood vessels and the appearance of new capillaries necessary to improve oxygen metabolism. All these criteria are important for the healthy development of the embryo. The blueness of the mucosa is noticeable at a very early stage, almost immediately after implantation of the embryo.
What the doctor will see and feel when examining the cervix
The size of the organ at the beginning of the process
At the initial stage of its development, the fetus is still very small. It's just a collection of cells that take up very little space. You can find out the size of the uterus in the early stages of pregnancy by its duration:
- by 4 weeks the size corresponds to a chicken egg;
- by 8 weeks the parameters double and resemble a goose egg;
- by 12 weeks the uterus can be compared to the head of a newborn;
- by week 16, the organ is similar in size to a small melon, because the height of the fetus reaches 13 cm.
The size of the uterus in the early stages of pregnancy can be smaller (if the parents are not very tall, and therefore the fetus is small). But in any case, the situation will have to be monitored, since it may be a reflection of anomalies in the development of the condition. A larger organ at each of the listed stages occurs with multiple pregnancy.
In the early stages of pregnancy, the uterus enlarges due to the stretching and growth of muscle cells, that is, the myometrium. They have the ability to divide, form new fibers, make them longer and denser. This can be prevented by scar inclusions that appear as a result of illness or previous births via cesarean section.
You can determine what kind of uterus you have during early pregnancy, taking into account its size, using an ultrasound or examination by a specialist. The highest point of the organ, called the bottom, is important. Its height corresponds to the period of pregnancy.
Form
The normal pear shape of the uterus changes from the time the embryo is implanted in it. If an increase in size is obvious from 4 weeks, then the shape takes on a slightly different shape even earlier. At the point where the embryo is screwed into the mucosa, a small protrusion forms. The uterus appears asymmetrical. As the fetus grows, its gradual transformation into a ball is noted. The change in shape is caused not only by the growth of the embryo, but also by the tissues that ensure its existence.
Consistency
Changes in the uterus in the early stages of pregnancy concern not only its size and configuration, they are more global in nature. This is expressed in the fact that the tissues become different from what was observed before. Changes are noted in all layers of the organ. One of them has already been mentioned: the endometrium is made more pliable so that the fertilized egg can firmly attach itself to it and exist comfortably.
An important sign that what is happening is correct is that the uterus becomes noticeably softer to the touch in the early stages of pregnancy. This is ensured by relaxation of its smooth muscles. This quality is also a necessary condition for the safety of the embryo. The contractility of the organ decreases. If this does not happen, there is a high probability of fetal rejection.
The hardest part of the uterus is the cervix. It plays the role of a boundary that fences off the approaches to the embryo. But its tissues also become more pliable than before conception.
Gradual changes in the uterus
The enlargement of the organ occurs gradually, which allows the female body to adapt to the new reality. The growing fetus compresses the surrounding tissues, forcing you to change your usual lifestyle.
Lifting the uterus into the abdominal cavity
Each stage of development is accompanied by conventional boundaries:
- Week 8. The uterus increases to twice its original size, but obvious visual changes are not yet observed.
- Week 12. The uterus protrudes above the symphysis pubis; this is the peak period of pregnancy toxicosis.
- Week 14 The organ increases to 12 cm, the first movement is felt.
- Week 16 The size of the organ is 14–15 cm. All vital structures of the embryo are fully formed. The upper border of the uterus can be felt in the midline between the womb and the umbilical fossa.
- Week 18. The organ increases to 18–19 cm and moves closer to the umbilical cavity.
- From 20 weeks, the height of the uterine fundus is set at 20 cm and increases by a centimeter every subsequent week.
After 36 weeks, the size of the organ changes slightly - 5-2 mm per week.
At what time can you palpate the uterus?
A woman can independently determine the boundary at about 12 weeks. It will be felt as a small painless lump above the symphysis pubis. In the presence of pathologies (fibroids, fibroids), the organ enlarges faster. During multiple pregnancies, the size of the uterus increases at a faster rate.
Methods for maintaining pregnancy with uterine exhaustion and cervical shortening
The cervix is a dense muscular ring that holds the fetus in the cavity and prevents it from slipping into the vagina. Throughout the entire gestation period, the cervix is in good shape, gradually shortening. By the time labor begins, it opens, releasing the baby's head.
If the cervix weakens earlier, this threatens spontaneous miscarriage and fetal death. Therefore, a woman is offered to strengthen the cervix in one of two suitable ways:
- Sutures are applied in a circular manner. The procedure is performed at 14–26 weeks, and the sutures are removed just before the birth process. Cerclage – suturing – has its contraindications:
- cervix dilated by more than 4 cm;
- inflammatory process;
- integrity violation.
Cerclage prevents premature birth, but has a number of side effects: localized hemorrhages, tears in the cervical tissue, rupture of the uterine wall.
- The application of a pessary is used when the cervix is exhausted to prevent spontaneous miscarriage. The device is a silicone ring placed on the lips of the cervix. The ring evenly distributes the load on the organ, normalizes blood supply and tissue nutrition. Prevents untimely dilatation of the cervix. The pessary is installed in the late stages of gestation (28–34 weeks) when there is a threat of fetal rejection.
Why the uterus does not meet its term
The height of the uterine fundus does not always correspond to the indicated period. Deviations can be significant, although the date of conception is set correctly. Why does this situation arise?
Placental insufficiency leads to a delay in the formation of the embryo, as a result – to reduced dynamics. This condition is caused by the presence of hypothyroidism in the mother, long-term debilitating toxicosis, and severe viral infections.
The opposite situation is the increased size of the uterus in relation to gestational age. A common diagnosis is polyhydramnios - an increased amount of amniotic fluid. It occurs as a result of infection with an intrauterine infection (herpes, cytomegalovirus and others). It has been noted that polyhydramnios occurs in women with a history of surgical or spontaneous abortion.
During a dynamically developing pregnancy, the upper border of the uterus fits within the allotted weekly norms reflected in the table. But if deviations occur, do not panic; non-compliance with accepted indicators does not indicate fetal pathology. There are many reasons why the size of the uterus exceeds or falls short of normal. It is necessary to conduct an examination and adjust the timing and condition.
Current video
After childbirth
After the birth of a child and placenta, already in the first hours of the postpartum period, a significant contraction (reduction in size) of the uterus occurs. The height of the uterine fundus in the first hours after birth is 15-20 cm. Restoration of the uterus after childbirth is called involution. During the first two weeks after birth, the fundus of the uterus drops approximately 1 cm daily.
- On the 1-2 days after birth, the fundus of the uterus is at the level of the navel - IMD 12-15 cm; x factors: characteristics of pregnancy and childbirth, breastfeeding, woman’s age, general condition, number of births in history. The uterus contracts more slowly in women over 30 years of age, in weakened and multiparous women, after multiple pregnancies and pregnancies complicated by polyhydramnios, with myomema, as well as when inflammation occurs in the uterus (endometritis) during pregnancy, childbirth or the postpartum period. In lactating women, uterine involution occurs faster, since breastfeeding produces the hormone oxytocin, which promotes uterine contractions.