Throughout a woman’s life, changes in the structure of the mammary glands constantly occur, which is reflected on X-ray mammograms.
In accordance with the functional age periods, three types of mammary glands are distinguished.
I. Gland of a girl or young woman (up to 20-25 years). The structure of the gland is almost uniform, the milk ducts are almost invisible, the width of the premammary space does not exceed 5 mm. Tumor formations arising in such a gland are practically indistinguishable on radiographs. In this regard, non-contrast mammography of the mammary glands at this age is inappropriate.
II. Functionally active gland (from 20-25 to 35-40 years). On mammograms, the mammary gland has a conical or hemispherical shape, the nipple is well developed and clearly defined. Differentiation into parenchyma and stroma occurs, the premammary space expands, small shadows of venous vessels and Cooper's ligaments appear. The shadow of the glandular triangle becomes heterogeneous, with a wavy outer contour due to an increase in the size of the glandular lobules. Heavy formations appear behind the nipple - images of the milk ducts.
Based on the ratio of glandular, fibrous and adipose tissue in the reproductive period, three radiological types of the structure of the mammary glands are distinguished:
1) Fibroglandular type of structure - glandular tissue is well developed in the mammary gland, fibrous tissue is expressed in the septa and ducts, and the amount of adipose tissue is minimal;
2) Fibrous-fatty type of structure - glandular tissue is moderately expressed, the ratio of glandular and adipose tissue is approximately the same, ducts may be visible against the background of adipose tissue;
3) Adipose type of structure - glandular tissue is poorly expressed, adipose tissue predominates over dense structures.
III. During the period of fading functional activity of the mammary glands, which begins at 40-45 years, involutive changes progress.
With the most common type of fatty involution, the glandular tissue gradually disappears and is replaced by adipose tissue. The shadow of the glandular triangle decreases in size, becomes heterogeneous, light accumulations of fatty tissue appear, against which loop-mesh connective tissue cords become distinct. Subsequently, the remains of glandular tissue appear as shadows of various shapes, appearing against the background of light adipose tissue. Against the background of adipose tissue, the shadows of tortuous veins, arteries, sometimes with calcifications, and the shadows of fibrous cords are clearly visible.
With the more rare fibrous variant of involutive changes, the glandular tissue is replaced by fibrous tissue. The entire mammary gland appears dense, its structure is heterogeneous. The delimitation of the glandular triangle from the retromammary and premammary fatty tissue becomes sharp, the border is uneven, with multiple strands directed from the body of the gland towards the skin.
IV. During the period of pronounced involution (senile age), glandular tissue is completely replaced by fat. Against the background of a homogeneous, “transparent” gland, multiple fibrous strands are revealed, running in different directions, but more often towards the areola, the shadow of convoluted veins, and calcified arteries. The border between the glandular triangle and the fatty tissue of the premammary and retromammary spaces is not visible.
Age is the main factor determining the structural type of the mammary gland. However, the X-ray picture of a normal mammary gland is very variable and also depends on the constitution, the state of the endocrine system, and the phase of the menstrual cycle.
When reading mammograms, they distinguish: skin, nipple, areola, subcutaneous fat, glandular tissue, connective tissue structures.
The skin on mammograms of a normal breast is visible as a smooth, uniform darkened strip bordering the gland. High-quality mammograms show clear and even contours of the outer and inner surface of the skin. The skin is separated from the glandular tissue by a light strip of subcutaneous fatty tissue - the so-called premammary space. The thickness of normal skin is 1-2 mm. Subtle linear and triangular stripes of shading extend from the skin into the premammary space, representing Cooper's ligaments.
In the anterior part of the mammary gland, in its most protruding part, the skin gradually thickens, passing without a clear boundary into the areola. The skin in the areola area has a folded structure.
Between the skin and glandular tissue there is a layer of fatty tissue. Due to the low density of fat, fiber appears more transparent on mammograms than skin and glandular tissue. The shadows of veins are clearly visible against the background of adipose tissue. Arteries are distinguished by the deposition of calcium salts in their walls.
The glandular part of the mammary gland itself looks like a cone or disk that is convex anteriorly, the base of which is adjacent to the pectoral fascia, and the apex ends with the nipple. The glandular tissue is grouped into 15-20 lobules, shaped like pyramids, with their apex directed toward the nipple and separated by layers of connective tissue. Each lobe is divided in turn into slices. The main structural unit of the mammary gland is the acinus, which is a group of small milky passages ending in terminal vesicles. On non-contrast mammograms, neither lobes, lobules, nor ducts are perceived differentially.
Didn't find what you were looking for? Use the search:
Best sayings:
For a student, the most important thing is not to pass the exam, but to remember about it in time.
10238 – | 7597 – or read all.
Increased breast density on mammography is considered a risk factor for the development of cancer, and recognition of the type of structure is an important factor in breast imaging, increasing the sensitivity of mamographic screening. Women at risk should be screened more frequently and/or with additional views.
Classifications
Pioneers in the development of breast density classifications were Leborgne in 1953 and Wolfe in 1967, who described the increased risk of cancer in dense breasts, but the first qualitative classification of mammographic densities was described by Wolfe in 1976.
What is a “dense” mammary gland?
“Dense” mammary gland is an X-ray concept. “The structure of the mammary gland consists of different types of tissue: adipose and fibroglandular (connective and glandular). Fibroglandular tissue gives a shadow on mammographic images, which is why it is called “radiologically dense,” says Irina Solntseva.
When there is more fibroglandular tissue in the structure of the mammary gland than fatty tissue, this condition is called “dense” mammary gland. “Doctors distinguish four types of density - A, B, C and D. The first two are non-dense types of structure, and they do not cause any concern. Types C and D are those options in which dense tissue predominates in the structure of the mammary gland. With the C-type it is in slightly smaller quantities, but with the D-type it occupies almost the entire volume of the gland,” explains the specialist.
It's written in the family. How to avoid hereditary cancer Read more
A little about the structure of the breast
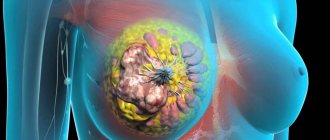
The mammary gland in women is located on the anterior surface of the chest from ribs 2-3 to 6. At rest, it is a system of blindly ending ducts; the alveoli are activated only during pregnancy, atrophying after breastfeeding.
Parenchyma
The main component of the female breast is functional epithelial glandular tissue (parenchyma). It consists of many round lobules - alveoli, and the lobules, in turn, are connected into a cone-shaped lobe (there are 20 of them in the parenchyma). The alveolar-lobular complexes are surrounded by a dense network of nerve endings, blood and lymphatic vessels and are immersed in the connective tissue stroma.
Fat and connective tissue are located between the alveoli. Cooper's ligaments, which are responsible for the shape of the breast, its support, and the attachment of the bust to the skin, also pass there. The connective tissue structures of the mammary glands are represented by a capsule and fibrillar tissue located between the glandular structures that form the walls of the milk ducts.
If we consider in more detail what parenchyma is, it is worth noting that this glandular tissue of the mammary gland is very complex in its structure. From each glandular lobule there passes a 1st order galactophthor with a diameter of up to 1 mm (milk duct), a 2nd order galactophthor with a diameter of 2 mm (intralobar duct), a 3rd order galactophthor with a diameter of up to 3 mm (extralobar duct) the milk ducts inside the nipple expand, forming a 5 mm pouch diameter The parenchyma is located in a connective sheath, and around it there is adipose tissue.
Fatty membrane
The fat layer is a necessary component of the female breast. Fat protects the mammary glands from injury and retains heat, which is extremely important for the normal production of breast milk. The amount of fat affects the size of a woman's breasts.
Fatty tissue covers the body of the mammary gland, forming retromammary (posterior) and premammary (anterior) layers. The premammary space is a clearing zone between the glandular tissue and the skin, formed due to the presence of adipose tissue there. The lipid layer in this space has a thickness of 3-30 mm. This parameter changes depending on the body type, age, and hormonal status of the woman.
Additional fabric
Some women experience additional breast tissue. It is usually located in the armpits and much less often on the back and face. The accessory tissue can be formed, it has an areola and a nipple, in which case it is called an accessory gland. If the tissue does not have ducts, then it is an additional lobe. Accessory nipples are very similar to birthmarks, but before menstruation or during pregnancy they become darker, swollen, and may leak milk. Tumorous, cystic, fibrous growths may appear in this area.
Similar article - Alt and ast are elevated in infants
Milk ducts, nipple
The milk ducts run from the tops of the lobes to the nipples. To the touch they look like tubercles and ligaments. At the end of the milk ducts there are milk pores through which lactation occurs. The nipple is a small cone-shaped seal. It has approximately 18 holes necessary for the release of milk. The nipple is surrounded by an areola, which is called the areola. There are many tubercles on the areola that prevent it from drying out.
Why should every woman know whether she has dense breasts?
Since 2021, the world's leading oncology communities have included the “dense” gland in the list of risk factors for breast cancer. Here it is worth understanding that the denser the gland tissue, the higher the risk of developing cancer. With C-type density, notes Irina Solntseva, the risks of developing breast cancer increase by about 2 times, and with D-type - by 4-6 times. And this is a really serious problem, says the specialist, because dense breast structure occurs in 60% of young women and 40% of postmenopausal women. Moreover, the risks of cancer are equally high both in youth and in adulthood.
If, according to the results of a mammography, it turns out that a woman has a “dense” mammary gland, the oncologist-mammologist evaluates what other risk factors for cancer are present in the patient. Among them:
- early onset of menstruation;
- late onset of menopause;
- long-term use of hormone replacement therapy;
- benign proliferative diseases of the mammary gland;
- hereditary factor.
In a situation where the patient has “dense” breasts, and there are also other risk factors for cancer, the oncologist can recommend an individual monitoring regimen for her. For example, reduce the period between screening examinations by scheduling mammography not once every two years, but once a year. In addition, for women with “dense” breasts, mammography alone is not enough, so the oncologist will definitely prescribe a further examination in the form of an ultrasound of the mammary glands.
Angelina Jolie syndrome. Who should have their breasts checked by a geneticist Read more
Symptoms of fibrosis
Along with understanding what localized breast fibrosis is, it is important to be able to recognize the symptoms that the disease manifests. The main features are the following:
- upon palpation, painful lesions are noticeable, having a rounded shape, which can be localized anywhere in the gland
- discomfort, heaviness in the chest
- presence of local pain, especially associated with menstruation
- heaviness and “goosebumps” during PMS
Fibrosis can localize its foci in any part of the gland, but with this disease there is no discharge from the nipples. This is the main factor that differentiates fibrosis from a number of other breast diseases.
Women of fertile age should first of all pay attention to the symptoms of the disease. Despite the lack of accurate statistics on incidence, expert estimates vary between 50-80% (in women of fertile age).
Don't ignore
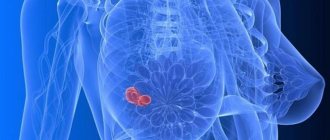
The task of doctors is to detect breast tumors at an early preclinical stage of development, because in these cases they are 95-98% curable.
It is well known that the only method of screening for breast cancer today is mammography, since its use has led to a decrease in mortality from this terrible disease. Mammography is necessary because, in addition to nodular formations, it is also capable of detecting such types of tumors as cancers in the form of an accumulation of microcalcifications or tumors in the form of a local violation of the architectonics of the mammary gland, which is not available to other diagnostic methods.
In addition to the fact that “dense” breast tissue is a risk factor for cancer, doctors note that a second important aspect is the fact that increased breast tissue density reduces the sensitivity of mammography, the main method for diagnosing breast cancer. “The mammographic density of tumor nodes is in many ways similar to dense breast tissue, so they become invisible against its background. And as a result, up to 40% of cancers are missed during mammography against the background of dense tissue,” says the expert.
That is, a third of women who already have a malignant tumor, during a mammographic examination, receive a conclusion that they do not have pathology of the mammary glands. In order not to miss tumors against the background of a dense structure, after mammography, doctors additionally prescribe an ultrasound of the mammary glands. Such a comprehensive examination can significantly increase sensitivity in detecting cancer. “It is extremely important for radiologists to describe the type of breast density in mammography protocols, so that the patient is aware of the peculiarities of the structure of her breasts and is sure to contact a mammologist-oncologist if she has a “dense” mammary gland. In these cases, an additional ultrasound examination and an individual monitoring regime are required,” the expert notes.
Tumor management. New weapons against cancer Read more
Survey technologies
If a mammogram reveals a “dense” mammary gland in a patient (density types C and D), doctors recommend undergoing an additional ultrasound of the mammary glands or a new technique for automated three-dimensional ultrasound examination. This technique allows you to obtain a three-dimensional image of breast tissue, which eliminates one of the most important disadvantages of the ultrasound method - operator dependence.
“The three-dimensional ultrasound technique is automated, which guarantees a complete examination of the entire mammary gland, without missing any area, even when examining large breasts or in the presence of implants,” says Irina Solntseva.
The sensitivity of three-dimensional ultrasound in detecting cancer against the background of a dense breast is 98-99%, therefore, it is currently the only method of ultrasound screening for breast cancer approved in the world, which is carried out additionally after mammography in cases of detection of a “dense” breast structure (types of density C and D) and the absence of focal pathology. In addition, the study is recommended for young women (under 40 years of age) who do not have any symptoms, but have risk factors for breast cancer, such as a BRCA ½ gene mutation and a family history.
Carrying out this procedure in addition to mammography against a background of dense breast tissue can detect 2.6 times more malignant tumors and 55% more invasive breast tumors.
Question answer
Can injury cause breast cancer?
Tissue modifications
Women's breasts, unfortunately, are susceptible to many diseases. That is why all representatives of the fair sex after 40 years and regardless of age (starting from 18 years), those who have had breast diseases in the female line, need to undergo mammography once a year in order to promptly identify the following changes in the mammary glands (if they available):
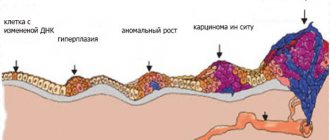
Diffuse fibrous
This pathological process is characterized by the appearance of multiple or single cystic tumors and epithelial cells in the breast. That is, diffuse breast tissue contains multiple inclusions of tissues that have a different cellular structure.
Sometimes dysplasia of the lobular structure of the glands occurs. Connective fibrosis, in which scar changes in tissues form, cannot be ruled out. In the diffuse form, there is increased breast tenderness, especially on palpation. When palpating the bust, elastic formations are easily identified. They practically disappear after menstruation, but discomfort still continues to bother the woman.
Involutively fibrous
This form is often detected in women who have entered the menopause phase. Involuting fibrotic changes are directly related to the hormonal status of women. As soon as the body reduces the production of normal amounts of estrogen, changes begin in the tissue of the mammary glands. The breasts become less elastic, lose their shape, and are painful when touched. For women in menopause, this phenomenon is quite normal. If it is observed at a younger age, examination is necessary to identify the cause.
Similar article - How to take wormwood to cleanse the body
Fibrocystic
This pathological condition is characterized by increased proliferation of parenchyma tissue ( hyperplasia of the glandular tissue of the mammary gland ) and the active formation of compactions with clear boundaries. Changes are typical for middle-aged women.
The disease occurs against the background of disorders of the menstrual cycle, ovulation, and reproductive function. It manifests itself as painful sensations in the chest due to fibrosis of the connective tissue and pressure from the dilated ducts. During palpation, you can feel granular, compacted breast tissue (if there is a fibrous form) or elastic formations that have clear contours (with a cystic form) measuring 2 millimeters or more. Over time, the tumors enlarge and cause discomfort.
To identify the disease, an ultrasound of the mammary glands is performed, which reveals an increase in fibroglandular tissue, dilation of the milk ducts, and a discrepancy between the amount and condition of the glandular tissue and the patient’s age.
The female breast is a very complex organ in its structure, the structure of which largely depends on the hormonal state of the woman. Any disturbance in hormone levels can lead to various changes in the breast tissue. Sometimes they are pathological and require treatment. To prevent the development of pathological processes, you need to learn how to independently palpate the bust for changes in the tissues, and entrust this process to a mammologist once a year.
Throughout a woman’s life, changes in the structure of the mammary glands constantly occur, which is reflected on X-ray mammograms.
In accordance with the functional age periods, three types of mammary glands are distinguished.
I. Gland of a girl or young woman (up to 20-25 years). The structure of the gland is almost uniform, the milk ducts are almost invisible, the width of the premammary space does not exceed 5 mm. Tumor formations arising in such a gland are practically indistinguishable on radiographs. In this regard, non-contrast mammography of the mammary glands at this age is inappropriate.
II. Functionally active gland (from 20-25 to 35-40 years). On mammograms, the mammary gland has a conical or hemispherical shape, the nipple is well developed and clearly defined. Differentiation into parenchyma and stroma occurs, the premammary space expands, small shadows of venous vessels and Cooper's ligaments appear. The shadow of the glandular triangle becomes heterogeneous, with a wavy outer contour due to an increase in the size of the glandular lobules. Heavy formations appear behind the nipple - images of the milk ducts.
Based on the ratio of glandular, fibrous and adipose tissue in the reproductive period, three radiological types of the structure of the mammary glands are distinguished:
1) Fibroglandular type of structure - glandular tissue is well developed in the mammary gland, fibrous tissue is expressed in the septa and ducts, and the amount of adipose tissue is minimal;
2) Fibrous-fatty type of structure - glandular tissue is moderately expressed, the ratio of glandular and adipose tissue is approximately the same, ducts may be visible against the background of adipose tissue;
3) Adipose type of structure - glandular tissue is poorly expressed, adipose tissue predominates over dense structures.
III. During the period of fading functional activity of the mammary glands, which begins at 40-45 years, involutive changes progress.
With the most common type of fatty involution, the glandular tissue gradually disappears and is replaced by adipose tissue. The shadow of the glandular triangle decreases in size, becomes heterogeneous, light accumulations of fatty tissue appear, against which loop-mesh connective tissue cords become distinct. Subsequently, the remains of glandular tissue appear as shadows of various shapes, appearing against the background of light adipose tissue. Against the background of adipose tissue, the shadows of tortuous veins, arteries, sometimes with calcifications, and the shadows of fibrous cords are clearly visible.
With the more rare fibrous variant of involutive changes, the glandular tissue is replaced by fibrous tissue. The entire mammary gland appears dense, its structure is heterogeneous. The delimitation of the glandular triangle from the retromammary and premammary fatty tissue becomes sharp, the border is uneven, with multiple strands directed from the body of the gland towards the skin.
IV. During the period of pronounced involution (senile age), glandular tissue is completely replaced by fat. Against the background of a homogeneous, “transparent” gland, multiple fibrous strands are revealed, running in different directions, but more often towards the areola, the shadow of convoluted veins, and calcified arteries. The border between the glandular triangle and the fatty tissue of the premammary and retromammary spaces is not visible.
Age is the main factor determining the structural type of the mammary gland. However, the X-ray picture of a normal mammary gland is very variable and also depends on the constitution, the state of the endocrine system, and the phase of the menstrual cycle.
When reading mammograms, they distinguish: skin, nipple, areola, subcutaneous fat, glandular tissue, connective tissue structures.
The skin on mammograms of a normal breast is visible as a smooth, uniform darkened strip bordering the gland. High-quality mammograms show clear and even contours of the outer and inner surface of the skin. The skin is separated from the glandular tissue by a light strip of subcutaneous fatty tissue - the so-called premammary space. The thickness of normal skin is 1-2 mm. Subtle linear and triangular stripes of shading extend from the skin into the premammary space, representing Cooper's ligaments.
In the anterior part of the mammary gland, in its most protruding part, the skin gradually thickens, passing without a clear boundary into the areola. The skin in the areola area has a folded structure.
Between the skin and glandular tissue there is a layer of fatty tissue. Due to the low density of fat, fiber appears more transparent on mammograms than skin and glandular tissue. The shadows of veins are clearly visible against the background of adipose tissue. Arteries are distinguished by the deposition of calcium salts in their walls.
The glandular part of the mammary gland itself looks like a cone or disk that is convex anteriorly, the base of which is adjacent to the pectoral fascia, and the apex ends with the nipple. The glandular tissue is grouped into 15-20 lobules, shaped like pyramids, with their apex directed toward the nipple and separated by layers of connective tissue. Each lobe is divided in turn into slices. The main structural unit of the mammary gland is the acinus, which is a group of small milky passages ending in terminal vesicles. On non-contrast mammograms, neither lobes, lobules, nor ducts are perceived differentially.
Didn't find what you were looking for? Use the search:
Best sayings:
Only sleep brings a student closer to the end of the lecture.
And someone else's snoring alienates him. 8944 — | 7615 - or read all.
How to protect yourself from breast cancer?
Currently, medicine does not know how to prevent the development of breast cancer, and therefore the most important and pressing task is its early diagnosis, at the stage when it is almost completely curable.
If a woman is regularly examined, the risk of missing the onset of tumor development is significantly reduced. After 40 years, all women need to undergo mammography regularly, once every 2 years, and in the case of “dense” breasts, additionally undergo ultrasound of the mammary glands with a frequency determined by a mammologist-oncologist. If a woman has complaints or there have been cases of malignant tumors in the family, then regular examinations, including examination by a mammologist and ultrasound, should begin from the age of 25-30 years. Do not forget that early diagnosis of breast cancer is a joint task between the doctor and the patient, and timely examination can save lives.
There are contraindications, you should consult a doctor